Respiratory Bronchiolitis
Martha Huller Maier, MD
Key Facts
Terminology
RB: Histologic reaction (pathologic in some) found in cigarette smokers
Usually asymptomatic
RB-ILD: Clinicopathologic syndrome found in heavy smokers
RB, RB-ILD, and DIP are part of spectrum of smoking-related lung diseases
Imaging Findings
RB: Mild patchy ground-glass opacities and centrilobular nodules more commonly found in upper lobes
HRCT often normal (sensitivity 25%)
Longitudinal observation: RB may evolve into centrilobular emphysema
Top Differential Diagnoses
Desquamative Interstitial Pneumonia
Langerhans Cell Histiocytosis
Hypersensitivity Pneumonitis
Pathology
Reactive accumulation of macrophages within lumen of respiratory bronchioles (2nd order) and surrounding alveoli
Clinical Issues
RB: Usually asymptomatic
RB: Universal histologic response in smokers, seen within 2 years of onset of smoking
M:F = 2:1
TERMINOLOGY
Abbreviations and Synonyms
Respiratory bronchiolitis (RB), desquamative interstitial pneumonitis (DIP)
Respiratory bronchiolitis-interstitial lung disease (RB-ILD)
Smoker’s bronchiolitis
Definitions
RB: Histologic reaction (pathologic in some) found in cigarette smokers
Usually asymptomatic
RB-ILD: Clinicopathologic syndrome found in heavy smokers
RB is pathologic lesion found on lung biopsy in patients with clinical condition of RB-ILD
Characterized by pulmonary symptoms, abnormal pulmonary function tests, and imaging abnormalities
RB, RB-ILD, and DIP are part of the spectrum of smoking-related lung diseases
IMAGING FINDINGS
General Features
Best diagnostic clue
RB: Mild patchy ground-glass opacities and centrilobular nodules more commonly found in upper lobes
RB-ILD: RB findings become more pronounced and widespread, especially ground-glass opacities
Mild thickening of central and peripheral airways
Patient position/location
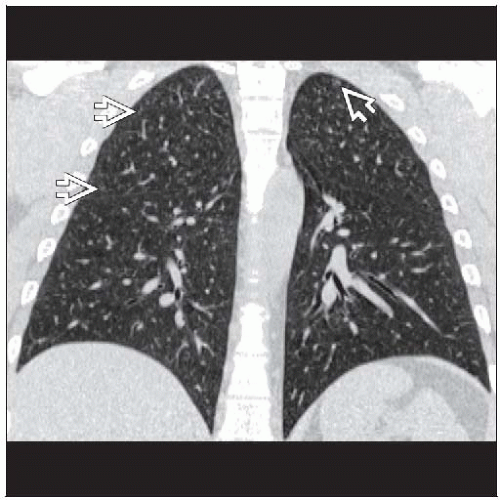
RB: Nodules most numerous in upper lung zones, sparing lung bases
RB-ILD: Distribution more extensive
May extend into lower lobes with coarse bibasilar bands of atelectasis and scarring
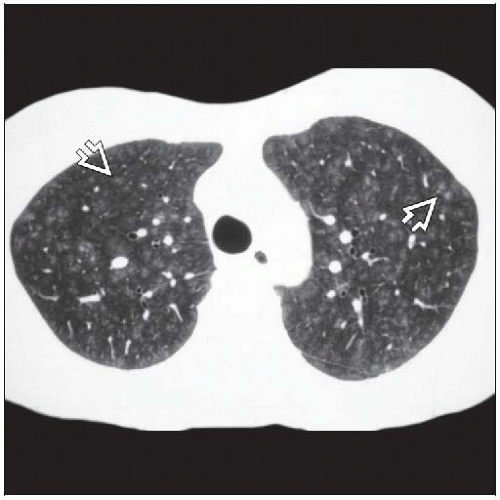
Size: Centrilobular nodules 3-5 mm in diameter
Morphology: Nodules generally ground-glass and ill defined
CT Findings
Respiratory bronchiolitis
HRCT often normal (sensitivity 25%)
Faint centrilobular micronodules (often overlooked)
Patchy ground-glass opacities
Predominantly upper lung zones
May have associated centrilobular emphysema
Respiratory bronchiolitis-interstitial lung disease
Upper lobe centrilobular nodules and patchy ground-glass opacities more pronounced
Mild reticular opacities may be present in lower lobes
Mild bronchial wall thickening
Centrilobular emphysema commonly associated; probably correlates with increased pack-year history and older age
RB & RB-ILD may be combined with other sequelae of smoking (bronchogenic carcinoma, emphysema, DIP)
Longitudinal observations
RB may evolve into centrilobular emphysema
Explains chronology (RB early, centrilobular emphysema late)
Explains location; both share location in 2nd order respiratory bronchiole and spatial distribution within upper lung zones
Radiographic Findings
Radiography
Respiratory bronchiolitis: Chest radiograph usually normal
Respiratory bronchiolitis-interstitial lung disease
Chest radiograph normal in up to 50% of patients
Normal lung volumes
Poorly defined hazy areas of increased density, upper lobes
Bronchial wall thickening
Fine reticular or reticulonodular pattern (rare)
Imaging Recommendations
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree