Retained products of conception (POCs) can occur after spontaneous or induced abortion and after delivery. They represent one of the most common reasons for presentation and hospital referral in the first trimester and postpartum period. Retained POCs can lead to endometritis, prolonged bleeding, and late complications such as intrauterine adhesions and impaired fertility. Accurate diagnosis and treatment are therefore critical to prevent both short- and long-term complications. The clinical diagnosis of retained POCs is made when symptoms, physical examination, sonographic findings, and serum β-human chorionic gonadotropin levels support the diagnosis. Unfortunately the diagnosis can be difficult because clinical and imaging findings can be nonspecific and similar to symptoms and findings occurring after normal delivery and spontaneous and induced abortion. In this chapter the clinical and imaging findings and treatment options for retained POCs will be reviewed.
DISEASE
Definition
Retained POCs refer to a portion of trophoblastic tissue that is retained in the uterine cavity after abortion or full-term delivery.
Prevalence and Epidemiology
Spontaneous abortion is the most common complication of pregnancy, occurring in at least 15% of clinically recognized pregnancies. In more than half of patients who present with symptoms of spontaneous abortion, retained POCs will be present in the uterus. These retained POCs will be due to an incomplete miscarriage in half (49%) of patients, with missed miscarriage (31%) and anembryonic pregnancy (20%) accounting for the remainder of cases. After first trimester pregnancy termination, retained POCs are uncommon, reported in 3.7% of cases.
Retained POCs are less common in the postpartum period, complicating approximately 1% of term vaginal deliveries. They represent, however, one of the most common reasons for hospital referral and readmission in the postpartum period. Retained POCs are more commonly seen with preterm delivery and with manual extraction of the placenta at delivery.
Etiology and Pathophysiology
In the first trimester, spontaneous abortion occurs with death of the embryo or failure of the early pregnancy. Subsequently, hemorrhage into the decidua basalis occurs, followed by necrosis of tissues adjacent to the bleeding. The gestational sac becomes partially or entirely detached. Uterine contractions and dilatation of the cervix subsequently occur, eventually resulting in expulsion of most or all of the POCs. An incomplete abortion occurs when POCs are only partially passed from the uterine cavity, leaving retained POCs within the uterus or cervix. In a missed abortion, the POCs are retained behind a closed cervix for days or even weeks. The cause of retained POCs from an incomplete or missed abortion is uncertain, but spontaneous resolution will often eventually occur. In a study by Sairam et al., 305 women with a mean gestational age of 8.9 weeks and an incomplete or missed abortion were managed expectantly. The overall success rate for expectant management was 86%, with a significantly higher success rate in the group with incomplete miscarriage (96%) compared with the group with missed miscarriage (62%).
Retained POCs after an induced abortion are uncommon, occurring most frequently if the abortion is attempted before 6 weeks of gestation. After pregnancy termination, retained POCs are more likely to occur when a uterine anomaly is present, and when fibroids or scarring alter the endometrial anatomy.
Retained POCs at term are suspected when visual inspection of the placenta in the delivery room reveals that the placenta is incomplete. This can be seen with placenta accreta, when the placenta is unusually adherent to the implantation site. This occurs when the underlying decidua basalis is defective or absent, leading to abnormal adherence of the placenta to the underlying myometrium. Risk factors for placenta accreta include placenta previa, previous cesarean section, uterine scarring from previous surgery, and multiple previous pregnancies. Abnormalities of placental development may also lead to retained POCs. In approximately 3% to 6% of pregnancies, a succenturiate or accessory lobe is present, which if not suspected at delivery may be retained.
Manifestations of Disease
Clinical Presentation
In the first trimester, after spontaneous abortion or termination, retained POCs are suspected when the patient presents with abnormal bleeding, abdominal pain, or fever. In many cases the cervical canal may be dilated. Serum β-human chorionic gonadotropin (hCG) levels may be checked, but they often contribute little to the diagnosis. Serum β-hCG levels can remain positive for weeks after an uncomplicated miscarriage or pregnancy termination, when no retained products are present. Alternatively an hCG level that is less than the assay threshold may be seen with necrotic retained POCs that are present in the uterus but do not actively secrete the hormone.
In the postpartum period, retained POCs are most commonly seen in the setting of secondary postpartum hemorrhage. This is defined as excessive vaginal blood loss or heavy lochial discharge occurring at least 24 hours after the end of the third stage of labor or during the following 6 weeks postpartum. The bleeding must be of sufficient quantity to prompt a review by an obstetrician. Other symptoms that patients report include pelvic pain, fever, and endometritis.
Imaging Indications and Algorithm
When a patient presents with vaginal bleeding in the first trimester of pregnancy or abnormal bleeding after pregnancy termination, pelvic ultrasound (US) is usually performed to evaluate the uterus for retained POCs. Likewise, US is considered the primary imaging modality for the assessment of patients with secondary postpartum hemorrhage. Magnetic resonance imaging (MRI) is not an appropriate first-line diagnostic procedure for the evaluation of abnormal bleeding in the postabortion or postpartum patient. In one report, however, MRI was found to be helpful in showing anatomic variants that might hinder successful instrumentation of the uterine cavity when retained POCs were present.
Imaging Technique and Findings
Ultrasound
Pelvic US is the primary imaging method used when a patient presents with vaginal bleeding or pain during pregnancy or in the postpartum period. In general, in the first trimester, a transvaginal approach is used to best evaluate the endometrium and intrauterine gestational sac contents, if present. In the postpartum period, a transabdominal approach is usually sufficient, particularly in the immediate postpartum period when the uterus is enlarged. After approximately 6 weeks postpartum, a transvaginal approach may provide a more detailed evaluation of the endometrium. From either approach, one of the main goals in these symptomatic patients is to evaluate the uterus for retained POCs. The sonographic features of retained POCs are variable and will be described.
First Trimester Retained POCs
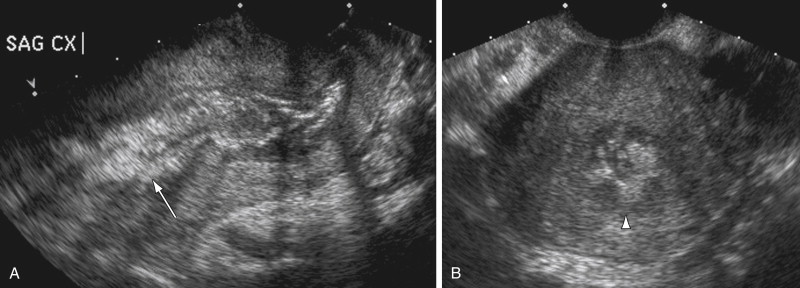
In the setting of a first trimester abortion, the sonographic diagnosis of retained POCs is not difficult to make when an irregular gestational sac with or without a nonviable embryo is identified in the uterus. Similarly, when the gestational sac is seen to migrate into the lower uterine segment over time, a spontaneous abortion in progress is suspected ( Figure 23-1 ). When no gestational sac is seen, the appearance and thickness of the endometrium should be assessed to evaluate for retained products. Findings such as an endometrial mass, an irregular endometrial–myometrial interface, a thick endometrium, and abnormal blood flow are some of the sonographic features that are consistent with retained POCs in the first trimester and will be reviewed.

A focal endometrial mass is one of the reported findings of retained POCs on US, representing the retained trophoblastic tissue ( Figure 23-2 ). On careful inspection of the endometrium, a focal mass is defined as distinct from the rest of the endometrium and measurable in three dimensions. When these criteria are met, the positive predictive value for retained POCs is 80%. The number of false-positive cases is significant, however, because blood clots can appear masslike on US and can be mistaken for retained POCs. Sonohysterography has been reported to be useful to distinguish retained POCs from clots. An echogenic mass that distends the endometrial cavity and is attached to the uterus is considered to be retained POCs, whereas a free-floating mass is presumed to represent a blood clot. Although believed to be a useful diagnostic tool in the setting of an endometrial mass and clinically suspected retained POCs, sonohysterography is not widely used for this purpose in the United States.

An irregular endometrial–myometrial interface is another finding that has also been reported in the setting of retained POCs in the first trimester ( Figure 23-3 ). When associated with a thickened endometrium, heterogeneity of the endometrium, and an intracavitary mass, the sensitivity for retained POCs is up to 100%. The significance of this finding in isolation has not been assessed, however, and therefore its value in the prediction of retained POCs is not clearly known. Additionally the finding is subjective and can be seen in both symptomatic and asymptomatic patients after first trimester abortion. At this time the finding of an irregular endometrial–myometrial interface may be suggestive of retained POCs but only in the setting of other suspicious sonographic findings.
The endometrial thickness, on the other hand, is a reproducible objective measurement that has been evaluated in a number of studies as a predictor of retained POCs in the first trimester. In general, if the endometrium is thin, retained POCs are unlikely ( Figure 23-4 ). If the endometrium is thick, retained POCs are more likely ( Figure 23-5 ). Unfortunately, there are no agreed-on threshold criteria in the literature for endometrial thickness in the detection of retained POCs. Suggestive cutoff values for endometrial thickness have ranged from 2 to 15 mm. Most of these cutoff values were chosen arbitrarily, however, and were not systematically evaluated to determine the best cutoff value.


In one study, retained POCs were unlikely when the endometrial stripe was less than 2 mm, but a thick endometrium greater than 5 mm was always associated with retained POCs. Another study reported a 100% sensitivity and 99.1% specificity for retained POCs using an endometrial thickness cutoff of 8 mm. Other studies have reported less success using endometrial thickness to diagnose retained POCs. Abbasi et al. found that endometrial thickness could not be used to differentiate retained POCs from decidua, as 31 of 36 patients with decidua, not retained POCs, had an endometrial thickness of more than 8 mm.
Problems arise in the diagnosis of retained POCs in patients with an endometrial thickness above a stated cutoff. One study looked at 74 patients after first trimester dilatation and curettage (D&C), none of whom needed further surgical intervention, and found that 50% of patients had an endometrial thickness of 7 to 19 mm and 27% had an endometrial thickness greater than 20 mm or a heterogeneous endometrium measuring at least 14 mm. This study illustrates that the uterine cavity is seldom empty after a first trimester abortion. The authors suggested that the presence of varying amounts of irregular intrauterine material and a thickened endometrium should be considered within the normal range of sonographic appearances and does not necessarily indicate the presence of retained POCs that require intervention. Therefore it is not surprising that the use of only an endometrial thickness above a certain cutoff as an isolated finding to diagnose retained POCs may lead to a false-positive diagnosis on US.
A thin endometrium, however, does have value in practically excluding retained POCs in most cases of first trimester abortion. In two studies the negative predictive value for retained POCs when the endometrial thickness was less than 8 to 10 mm was 100%. Technically, retained POCs can rarely be excluded by an endometrial measurement because retained POCs have been reported even when the endometrium measures less than 5 mm. It may be, however, that these small amounts of retained POCs are not clinically significant. In one study, patients presenting with a spontaneous first trimester abortion and an endometrial thickness less than 8 mm were managed conservatively with success. Some of these patients might have had a small amount of retained POCs, but none required subsequent uterine curettage or subsequently passed a tissue mass after discharge from the hospital.
Color Doppler US has also been reported to add value in the diagnosis of retained POCs in the first trimester. The presence of blood flow within an endometrial mass or thickened endometrium is more likely with retained POCs (see Figure 23-2 , C ), whereas absence of blood flow suggests blood clots ( Figure 23-6 ). The reliability of Doppler US for retained POCs is somewhat variable in the literature, however. Studies have assessed blood flow within the myometrium or just beneath the endometrial–myometrial interface and blood flow within the myometrial arteries.











