Retrocalcaneal and Achilles Bursitis
Anatomic Considerations
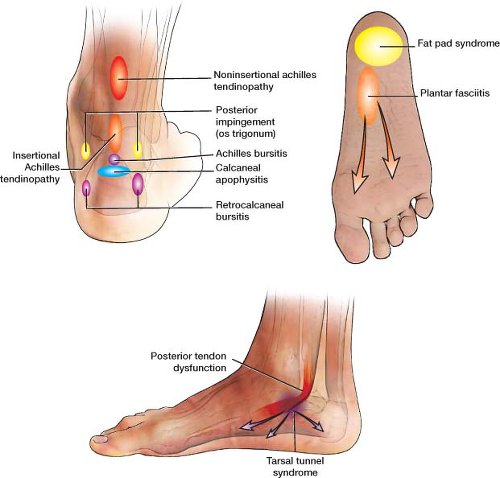
The retrocalcaneal bursa lies between the Achilles tendon and the base of the tibia and the posterior calcaneus (Fig. 15.1). The bursa is subject to the development of inflammation after overuse, misuse, or direct trauma as is the Achilles bursa which lies posterior to the Achilles tendon at its insertion on the calcaneus. The Achilles tendon is the thickest and strongest tendon in the body, yet also very susceptible to rupture. The common tendon of the gastrocnemius muscle, the Achilles tendon, begins at mid-calf and continues downward to attach to the posterior calcaneus, where it may become inflamed. The Achilles tendon narrows during this downward course, becoming most narrow approximately 4 to 5 cm above its calcaneal insertion (Fig. 15.2). It is at this narrowmost point that tendinitis also may occur. Tendinitis, especially at the calcaneal insertion, may mimic retrocalcaneal bursitis and may make diagnosis difficult. The Achilles bursa lies between the skin and the Achilles tendon (Fig 15.1). It is an adventitious bursa which when inflamed is also known as “pump bump” due to its association with the hard back of ill-fitting pump style shoes.
Clinical Correlates
Retrocalcaneal bursitis is a common cause of posterior heel pain (Fig. 15.3). The retrocalcaneal bursa, which is also known as the subtendinous calcaneal bursa, lies between the Achilles tendon and its insertion on the calcaneus (Figs. 15.3 and 15.4). The bursa serves to cushion and facilitate sliding of the Achilles
tendon over the calcaneus. The bursa is subject to inflammation from a variety of causes with acute trauma to the knee and repetitive microtrauma being the most common. Acute injuries to the bursa can occur from direct blunt trauma to the posterior ankle such as kicks while playing sports. The bursa may also become inflammed as a result of overuse injuries, running on uneven or soft surfaces, and jobs that require repeated plantar flexion of the ankle. If the inflammation of the bursa is not treated and the condition becomes chronic, calcification of the bursa with further functional disability may occur. Gout and other crystal arthropathies may also precipitate acute retrocalcaneal bursitis as may bacterial, tubercular, or fungal infections (Fig. 15.5).
tendon over the calcaneus. The bursa is subject to inflammation from a variety of causes with acute trauma to the knee and repetitive microtrauma being the most common. Acute injuries to the bursa can occur from direct blunt trauma to the posterior ankle such as kicks while playing sports. The bursa may also become inflammed as a result of overuse injuries, running on uneven or soft surfaces, and jobs that require repeated plantar flexion of the ankle. If the inflammation of the bursa is not treated and the condition becomes chronic, calcification of the bursa with further functional disability may occur. Gout and other crystal arthropathies may also precipitate acute retrocalcaneal bursitis as may bacterial, tubercular, or fungal infections (Fig. 15.5).
The patient suffering from retrocalcaneal bursitis most frequently present with the complaint of pain in the posterior heel which may radiate into the posterior ankle. The patient may find walking downstairs, standing on tiptoes, and kneeling increasingly difficult. Physical examination of the patient suffering from retrocalcaneal bursitis will reveal point tenderness over the heel, with the medial side affected more commonly
than the lateral. If there is significant inflammation, rubor and color may be present and the entire area may feel boggy or edematous to palpation. At times massive effusion may be present which can be quite distressing to the patient. Active plantar flexion of the affected knee will often reproduce the patient’s pain. Sudden release of resistance to active plantar will markedly increase the pain. If calcification or gouty tophi or xanthomas associated with familial hypercholesterolemia of the bursa and surrounding tendons are present, the examiner may appreciate crepitus with active extension of the knee and the patient may complain of a catching sensation when moving the affected knee, especially on awaking (Fig. 15.6). Often, the patient will not be able to sleep on the affected side. Occasionally, the retrocalcaneal bursa may become infected, with systemic symptoms, including fever and malaise, as well as local symptoms, with rubor, color, and dolor being present.
than the lateral. If there is significant inflammation, rubor and color may be present and the entire area may feel boggy or edematous to palpation. At times massive effusion may be present which can be quite distressing to the patient. Active plantar flexion of the affected knee will often reproduce the patient’s pain. Sudden release of resistance to active plantar will markedly increase the pain. If calcification or gouty tophi or xanthomas associated with familial hypercholesterolemia of the bursa and surrounding tendons are present, the examiner may appreciate crepitus with active extension of the knee and the patient may complain of a catching sensation when moving the affected knee, especially on awaking (Fig. 15.6). Often, the patient will not be able to sleep on the affected side. Occasionally, the retrocalcaneal bursa may become infected, with systemic symptoms, including fever and malaise, as well as local symptoms, with rubor, color, and dolor being present.
Patients with a prominent and upturned calcaneal tuberosity are predisposed to the development of Achilles bursitis or pump bump (Fig. 15.7). When this boney abnormality is associated with Achilles bursitis, Achilles insertional tendinitis, Achilles tendinosis and tearing, and at times, retrocalcaneal bursitis, this constellation of symptoms is known as Haglund disease or deformity (Figs. 15.8 and 15.9).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree