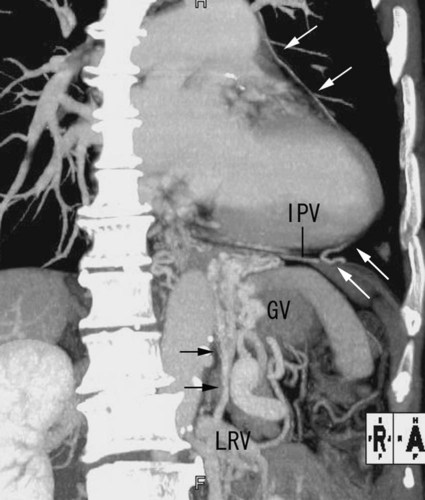
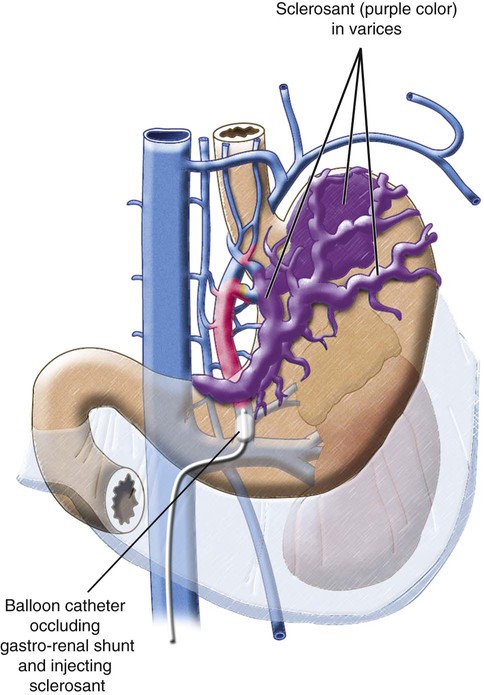
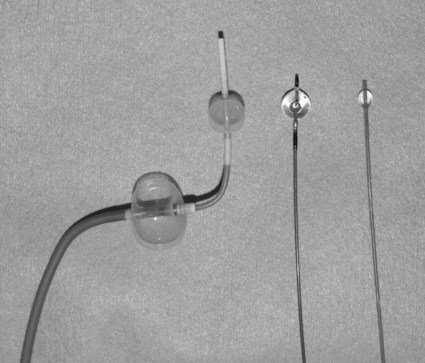
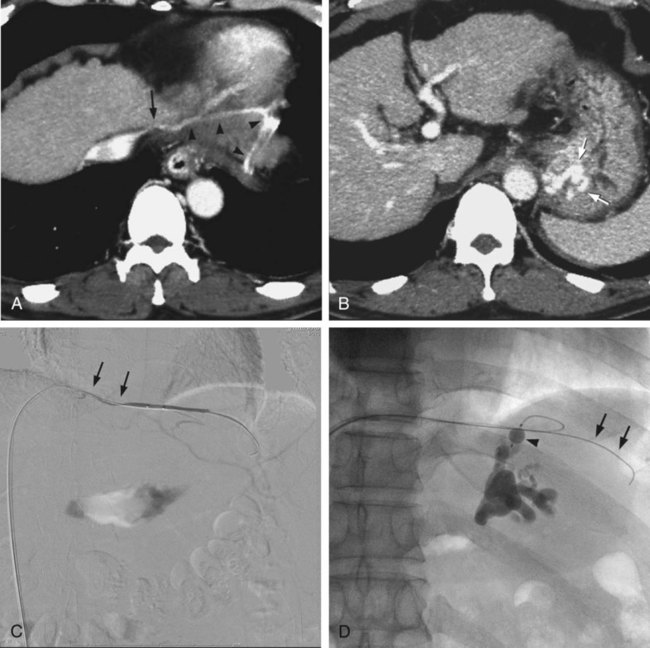
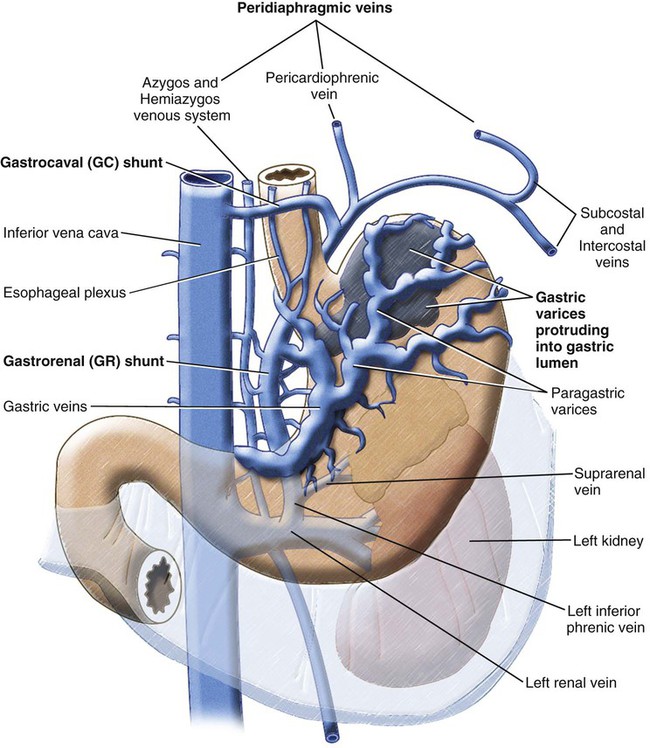
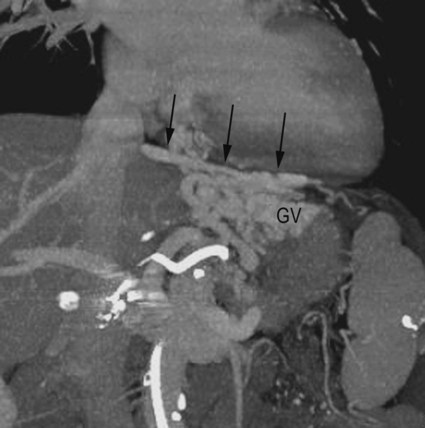
Chapter 113 When compared with esophageal variceal bleeding, bleeding from gastric varices is usually more severe and difficult to control. Gastric varices are classified into two types: gastroesophageal varices and isolated varices.1,2 Gastroesophageal varices located at the cardia are considered part of esophageal varices. Gastroesophageal varices always drain into esophageal varices, and they are usually treated endoscopically (Fig. 113-1). In contrast, isolated varices are usually located at the fundus or at the cardia and fundus and develop independently as part of a large portosystemic shunt that runs through the stomach wall and drains into the left renal vein or inferior vena cava (IVC) (Fig. 113-2).2 Because of their large size and high flow, endoscopic treatment of isolated gastric varices is difficult. With recent developments in interventional techniques, the majority of isolated gastric varices can be treated safely with a balloon-occluded retrograde transvenous obliteration (BRTO) technique.3–5 In BRTO, sclerosant is injected via a balloon catheter positioned at the outlet of the vein draining the gastric varices (gastrorenal or gastrocaval shunt), and the sclerosant fills and stagnates in the varices under balloon occlusion of the shunt (Fig. 113-3). When the sclerosant sufficiently stagnates in the varices, complete thrombosis of the varices can be ensured. Reported success rates of the BRTO technique have ranged from 90% to 100%. Recurrent gastric varices or rebleeding from gastric varices after BRTO occurs rarely. Isolated gastric varices at high risk for rupture or those that have already ruptured are an indication for BRTO. High-risk varices include large varices, those with red spots, and rapidly growing varices. Some authors have performed BRTO for the treatment of portosystemic encephalopathy and ectopic varices such as duodenal varices.6 However, the long-term efficacy of BRTO for portosystemic encephalopathy has not been confirmed. Portal venous pressure will be elevated after BRTO because a large portosystemic shunt is often obliterated concurrently with obliteration of the gastric varices. Therefore, portal venous occlusion or refractory ascites is generally thought to be a contraindication to BRTO. Although a selective infusion technique with a microcatheter may selectively obliterate gastric varices while preserving the portosystemic shunt, it cannot be predicted before treatment whether the shunt will be occluded.7 Aggravation of esophageal varices is also frequently observed after BRTO8; therefore, performance of BRTO for high-risk esophageal varices would increase the risk for bleeding from esophageal varices. In the treatment of patients with both unruptured gastric varices and high-risk esophageal varices, the esophageal varices should be treated by endoscopic techniques before BRTO. Ethanolamine oleate, commonly used as a sclerosing agent, may induce acute renal failure because of its hemolytic effect.9 Renal insufficiency (serum creatinine > 1.5 mg/dL) is also a contraindication or should be carefully treated. A 6F to 7F Simmons-shaped balloon catheter has generally been used for occlusion of gastrorenal shunts (Fig. 113-4). The balloon catheter should have a wide lumen through which a microcatheter can be inserted and should also have a large-diameter balloon (>15 mm) to occlude a large shunt completely. A 5F or 6F C-shaped catheter with a balloon has been used for occlusion of gastrocaval shunts. For the technique of selective BRTO, a 9F/5F coaxial balloon catheter that can easily be advanced proximally to the varices (Fig. 113-5) is used.10 A microcatheter can be inserted through the 5F coaxial balloon catheter. The 9F guiding balloon is positioned at the outlet of the gastrorenal shunt, and the 5F balloon catheter is introduced coaxially into the proximal portion of the shunt over a microcatheter advanced into the varices. The sclerosing agent is then infused via the microcatheter under balloon occlusion of the shunt at the outlet and proximal portion. Microballoon catheters are recently available, which is useful for selective BRTO in cases with a small and tortuous access route (Fig. 113-6). These catheters come in 3.3F to 3.5F sizes with a 6- to 10-mm balloon (see Fig. 113-5), and they can be introduced through a 6F guiding catheter or 4F sheath over a microguidewire of 0.014 inch. For BRTO, 5% ethanolamine oleate iopamidol (EOI), which consists of a mixture of 10% ethanolamine oleate (Oldamin) and the same dose of a contrast agent (iopamidol 300), is commonly used. Because some types of contrast material cannot be mixed with ethanolamine oleate, we used iopamidol 300. Ethanolamine oleate induces hemolysis in blood vessels, and free hemoglobin is released, which may result in renal tubular disturbances and acute renal failure. To prevent renal insufficiency, intravenous administration of 4000 units of haptoglobin, which combines with free hemoglobin, is performed during the procedure. Polidocanol in the form of foam has been recently used as a sclerosing agent alternative to ethanolamine olerate.11 Foam sclerotherapy using polidocanol may reduce the drug amount and maximize the effect by increasing the contact surface area with the venous wall. However, one should be aware of the potential risks of air embolism. Some authors used 50% glucose solution, which is infused before injection of EOI to occluded collateral veins or to replace the blood. This technique can reduce the amount of EOI.12 Isolated gastric varices are usually located at the fundus or at the cardia and fundus and develop independently as part of a large portosystemic shunt that runs through the stomach wall and drains into the left renal vein or IVC.2 The portosystemic shunt consists of afferent gastric veins and the left inferior phrenic vein, which drains into the left renal vein (gastrorenal shunt; 80%-85%) or directly into the IVC (gastrocaval shunt; 10%-15%) or into both the renal vein and the IVC. The left inferior phrenic vein often communicates with other peridiaphragmatic veins, including the left pericardiophrenic vein, intercostal vein, and azygos vein. These peridiaphragmatic veins, along with the main portosystemic shunt, act as collateral veins draining the gastric varices and would be an obstacle to sufficient filling of sclerosant in the gastric varices during BRTO. Knowledge of potential communications between the gastric varices and peridiaphragmatic veins is very important for successful treatment of gastric varices by BRTO.4,5,13 The left inferior phrenic vein often ends in the left renal vein together with the left adrenal vein or passes in front of the esophageal hiatus in the diaphragm and ends in the IVC or left hepatic vein. The proximal portion of the left inferior phrenic vein runs inferior to the diaphragm, and its peripheral branches run superior to the diaphragm. The left inferior phrenic vein potentially communicates with other peridiaphragmatic veins, including the left pericardiophrenic vein, intercostal vein, and anastomotic veins to the right inferior phrenic vein or azygos venous system14; consequently, fundic varices can also drain through these potential communications (Fig. 113-7; also see Fig. 113-2). In our experience with portography, balloon-occluded venography, or both in 85 patients with isolated gastric varices, the main drainage routes from the gastric varices were gastrorenal shunts in 52 cases (61.2%), gastrocaval shunts in 3 cases (3.5%), both gastrorenal and gastrocaval shunts in 26 cases (30.6%), and other peridiaphragmatic veins in 4 cases (4.7%). In a portographic study of 20 patients by Chikamori et al., isolated gastric varices drained into a gastrorenal shunt in 85%, a gastrocaval shunt in 10%, and the pericardiophrenic vein in 5%.2 A gastrorenal shunt ends in the left renal vein together with or separately from the left adrenal vein. It often has small retroperitoneal veins communicating with the azygos venous system, and the left adrenal vein and is sometimes associated with other large collaterals through the gastrocaval shunt or left pericardiophrenic vein (see Fig. 113-2). A gastrocaval shunt ends in the IVC or left hepatic vein (Fig. 113-8). The left inferior phrenic vein runs above the diaphragm peripherally, penetrates the diaphragm near the cardiac apex, and then travels on the inferior surface of the diaphragm. The peripheral portion of the left inferior phrenic vein has many collateral veins, so the majority of gastrocaval shunts are always associated with additional collateral drainage, including the left pericardial vein, veins of the thoracic wall, and an anastomotic vein to the right inferior phrenic vein (see Fig. 113-7). BRTO for this type of gastric variceal drainage is often more difficult than that for varices draining only into the gastrorenal shunt. The diaphragmatic branches of the left pericardiophrenic vein anastomose with the supradiaphragmatic portion of the inferior phrenic vein, which ascends parallel to the left cardiac border and drains into the left brachiocephalic vein, the superior intercostal vein, or the internal mammary vein. The vein can function as a collateral pathway in patients with occlusion of the IVC or superior vena cava (SVC) and portal hypertension. Pericardiophrenic venous drainage from varices is usually associated with a gastrocaval or gastrorenal shunt (Fig. 113-9), but it can exist alone. Performance of BRTO through the left pericardiophrenic vein has a potential risk for serious arrhythmia secondary to stimulation by catheter manipulation or sclerosant.
Retrograde Balloon Occlusion Variceal Ablation
Indications
Contraindications
Equipment
Balloon Catheter
Sclerosing Agent
Technique
Anatomy and Approach
Gastrorenal Shunt
Gastrocaval Shunt
Pericardiophrenic Vein
Retrograde Balloon Occlusion Variceal Ablation