Rheumatologic Disease: Imaging with PET-CT and SPECT-CT
Klaus Strobel
Jürg Hodler
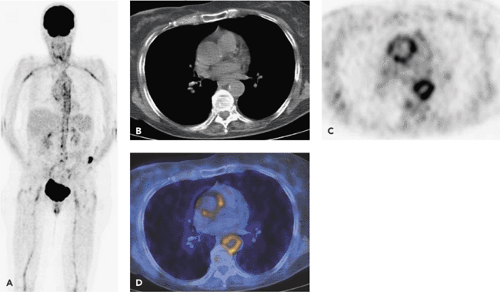
Because fluorodeoxyglucose (FDG) is taken up into activated granulocytes, lymphocytes, and macrophages, positron emission tomography (PET) has the potential to visualize not only infectious but also sterile inflammations that are present in active rheumatologic diseases. So far, the impact of PET on the diagnosis and follow-up of rheumatologic diseases is not yet defined. Promising results have been reported for large-vessel vasculitis. PET demonstrates increased uptake within large artery walls involved in vasculitis in patients with fever of unknown origin (see Fig. 62.1). If vasculitis is clinically suspected, PET may be superior in the evaluation of the extent and grade of activity of the disease compared with other imaging methods, including magnetic resonance imaging (MRI). PET combined with computed tomography (CT) angiography offers a “one-stop shop” approach that demonstrates not only the classical PET signs of vasculitis but also complications that have been classical indications for CT, including stenosis, aneurysm, or dissection. Physiological and atherosclerotic vessel uptake should be considered as differential diagnoses if vasculitis is suspected. Coregistered CT angiography can show atherosclerotic plaques, which helps to solve interpretation problems.
Rheumatoid arthritis is a common, chronic, and progressive disease. It has the highest incidence of all autoimmune diseases. Although some studies dealing with the use of PET in this disease have been done, further studies are needed to evaluate whether metabolic imaging with PET plays a substantial role in the imaging of these patients. PET has been discussed for the initial diagnosis and “staging” of the inflammatory process. Another potential application of PET relates to the monitoring of therapy when expensive new types of medication are being considered.
PET may also occasionally be useful in the differentiation of inflammatory abnormalities potentially mimicking other diseases, such as pulmonary nodules and lymphadenopathy. Experience with PET in systemic lupus erythematosus (SLE), ankylosing spondylitis, and Behçet syndrome is still very limited.
Bone scintigraphy, widely used for imaging patients with various types of arthritis, is very sensitive but unspecific in the diagnosis of inflammatory disease. In comparison with standard bone scintigraphy, single-photon emission computed tomography (SPECT) increases image contrast and improves lesion detection and localization. Evaluation of hot spots with multi-slice CT in the same session increases the specificity and can provide additional important information, such as the extent of bone destruction.
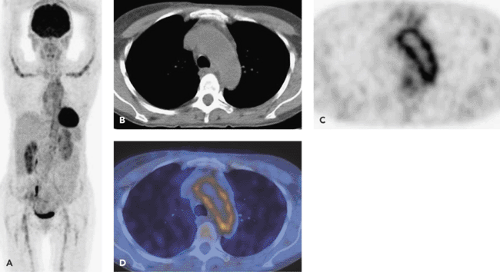
PET in Vasculitis
Vasculitis includes different diseases presenting with inflammation of the arterial wall. The 1992 Chapel-Hill consensus conference defined the vasculitides according to their pathological features and the size of the involved arteries (1). Conventional scintigraphy is not accurate in detecting vessel wall inflammation (2). The most important entities for imaging with PET are the large-vessel arteritides: giant cell arteritis (GCA) and Takayasu arteritis (TA). The diagnosis relies mostly on symptoms, laboratory tests, ultrasound, MRI, invasive pathologic and angiographic investigations, and clinical outcome after treatment. GCA affects patients older than 50 years and presents with new headache and elevation of erythrocyte sedimentation rate. Patients with TA usually present at younger age (younger than 40 years), often with a difference in systolic blood pressure between the arms and bruits over the subclavian arteries or the aorta as a result of stenosis (3,4,5). Polymyalgia rheumatica (PR) is a common illness in elderly persons presenting with proximal muscle pain and stiffness. There is clear evidence that vasculitis of medium-size and large arteries play an important role in PR. Positron emission tomography (PET) studies confirm the suspicion that in many patients PR is associated with subclinical large-vessel vasculitis. Moosig investigated 13 untreated patients with active PR and found increased fluorodeoxyglucose (FDG) activity of the aorta and its major branches in 12 patients (6). Patients with large-cell vasculitis may initially present with untypical and unspecific symptoms, like fever of unknown origin (Fig. 62.1). Diagnosis of vasculitis can be confirmed by typical abnormalities in a temporal artery biopsy, but temporal artery biopsy in vasculitis patients can be falsely negative (Fig. 62.2). An imaging method providing an overview such as PET is important, because the extent of extracranial vessel involvement in GCA is often clinically underestimated and may only be confirmed by autopsy results. Complications of large-vessel inflammation, including stroke, ruptured aneurysm, dissection, and infarction (kidney, heart), are rare but potentially life-threatening (7). Metabolic imaging with FDG-PET has the potential to confirm the diagnosis by visualization of the inflammatory process within the vessel wall. In decreasing order, GCA involves the aorta, the carotid arteries, and the upper and lower limb arteries. TA typically affects the aortic arch and descending aorta, the subclavian arteries, and the pulmonary arteries.
Large-vessel vasculitis has to be differentiated from physiological vessel activity. Mild FDG activity is commonly found within the wall of large vessels, most pronounced in the thoracic aorta of elderly patients (8). Active atherosclerosis is an important differential diagnosis for vasculitis. Atherosclerotic plaques are said to accumulate FDG (9). The pattern and grade of vascular FDG uptake has to be evaluated. FDG accumulation in active atherosclerosis appears to be more focally distributed, to be of mild grade, and to affect the upper and lower legs predominantly. Visualization of calcified plaques in low-dose computed tomography (CT) or soft plaques in CT angiography
in the area of vessel wall FDG activity make the diagnosis more likely. Intense, symmetric FDG uptake involving the large cervical and thoracic vessels is highly suspicious for a vasculitic process.
in the area of vessel wall FDG activity make the diagnosis more likely. Intense, symmetric FDG uptake involving the large cervical and thoracic vessels is highly suspicious for a vasculitic process.
FDG-PET can be used in monitoring of therapy response. Apparently, there is a good correlation between inflammatory blood parameters and FDG activity in the vessel wall (10). Unlike in GCA, the inflammation parameters in TA do not necessarily reflect disease activity (11). In comparison to “standard” imaging modalities such as ultrasound or magnetic resonance imaging (MRI), FDG-PET has a number of advantages, including that it may detect vasculitis earlier than MRI (12). In addition, PET demonstrates the entire extent of vascular involvement during a single imaging session. PET is also investigator independent and therefore more reproducible than ultrasound. If it is combined with CT angiography performed with intravenous iodine contrast media, potential complications of vasculitis, including aneurysm, dissection, and stenosis, can be detected in a “one-stop shop” imaging approach.
The main indication of FDG-PET is an atypical presentation of large-vessel vasculitis, and it is also used to monitor response to anti-inflammatory treatment. It has the potential to reduce the time to diagnosis and to detect clinically and radiologically unsuspected but potentially life-threatening vascular involvement. Especially when it is used in combination with CT angiography, the number of conventional invasive angiograms may be reduced. PET can help to determine the most accurate location for biopsy.
Moderate vascular uptake should be interpreted cautiously, especially in elderly patients with atherosclerosis. All published studies concerning imaging in vasculitis have the limitation of lacking a standard of reference, because biopsy of large vessels and histopathological correlation is not practical in most cases.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree