Presentation and Presenting Images
( ▶ Fig. 86.1, ▶ Fig. 86.2, ▶ Fig. 86.3, ▶ Fig. 86.4, ▶ Fig. 86.5, ▶ Fig. 86.6, ▶ Fig. 86.7, ▶ Fig. 86.8, ▶ Fig. 86.9, ▶ Fig. 86.10, ▶ Fig. 86.11, ▶ Fig. 86.12)
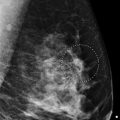
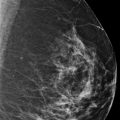
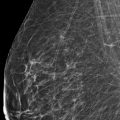
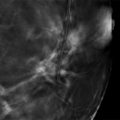
A 56-year-old female presents for evaluation of generalized right breast pain. This is her baseline mammogram.
86.1.1 Breast Tissue Density
There are scattered areas of fibroglandular density.
86.1.2 Imaging Findings
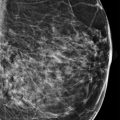
There are no prior studies for comparison. The imaging of the left breast is normal (not shown). The right breast demonstrates oval masses (circles) at the 11 o’clock location in the anterior depth, 2 cm from the nipple, and at the 7 to 8 o’clock location in the middle depth, 5.5 cm from the nipple ( ▶ Fig. 86.7, ▶ Fig. 86.8, ▶ Fig. 86.9). Digital breast tomosynthesis shows the margins of both masses are well circumscribed ( ▶ Fig. 86.10, ▶ Fig. 86.11, and ▶ Fig. 86.12). No other masses are seen.
The patient is premenopausal and not at an increased risk to develop breast cancer (no family history or genetic predisposition). Ultrasound is recommended to further evaluate both masses.
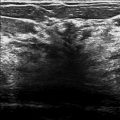
86.2 Diagnostic Images
86.2.1 Imaging Findings
Ultrasound was performed. The mass at the 11 o’clock position (3.3 cm from the nipple) was shown to be a well-circumscribed hypoechoic mass. The mass at the 7 o’clock position (5.8 cm from the nipple) was a well-circumscribed anechoic mass. The cyst is benign (7 o’clock mass); no further work-up is needed. The solid benign-appearing mass (11 o’clock mass) may be followed short-term with repeat sonography in 6 months.
86.3 BI-RADS Classification and Action
Category 3: Probably benign
86.4 Differential Diagnosis
Benign and probably benign masses: Both masses have benign sonographic findings. As this was a baseline exam, it was decided to follow the solid mass with benign features, but it could have been decided to biopsy instead. This decision should involve a discussion with the patient about the level of suspicion of malignancy and about her ability to follow an imaging finding for 2 years to assure it remains stable.
Suspicious masses: There are no suspicious sonographic findings associated with either mass.
Summation artifacts: Both masses persist on conventional mammography and DBT imaging, and again are confirmed on sonography.
86.5 Essential Facts
Benign sonographic characteristics include the following: well-circumscribed margins, wider than tall orientation, less than three gentle lobulations, and the absence of any malignant characteristics.
Malignant sonographic characteristics include the following: spiculated margins, taller than wider orientation, microlobulation, angular margins, and posterior acoustic shadowing.
Conventional mammography plus DBT increases reader performance for identifying masses and architectural distortions over conventional mammography alone.
DBT increases the detection of masses including invasive cancers in breasts of all parenchymal densities and reduces the recall rate while increasing the positive predictive value for both recalls and biopsies.
86.6 Management and Digital Breast Tomosynthesis Principles
DBT is both a screening and diagnostic modality.
DBT acquires several images of the breast at multiple angles. The individual images are reconstructed into a series of thin, high-resolution slices typically 1-mm thick, which can be viewed in the same manner as computed tomography (CT) or magnetic resonance (MR) images, as single slices or dynamically as a movie (cine).
The ability to view images as a single slice or dynamically as a movie eliminates the effects of overlapping breast tissue and allows for better visualization and characterization of masses.
Benign and malignant lesions may have similar appearances on mammography.
Radiologists need to be careful not to dismiss all benign-appearing masses as benign.
86.7 Further Reading
[1] Rafferty EA, Park JM, Philpotts LE, et al. Assessing radiologist performance using combined digital mammography and breast tomosynthesis compared with digital mammography alone: results of a multicenter, multireader trial. Radiology. 2013; 266(1): 104‐113 PubMed
[2] Rose SL, Tidwell AL, Bujnoch LJ, Kushwaha AC, Nordmann AS, Sexton RJr. Implementation of breast tomosynthesis in a routine screening practice: an observational study. AJR Am J Roentgenol. 2013; 200(6): 1401‐1408 PubMed
[3] Stavros AT, Thickman D, Rapp CL, et al. Solid breast nodules: use of sonography to distinguish between benign and malignant lesions. Radiology. 1995;196(1):123-134
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree