Right Upper Quadrant: Liver, Gallbladder, and Biliary Tree
Karen S. Cosby
John L. Kendall
INTRODUCTION
Abdominal pain is a leading cause for visits to the emergency department (ED). The evaluation of the abdomen frequently utilizes many resources, not the least of which is the time often invested in serial exams, use of consultants, and imaging procedures. Focused bedside ultrasound offers a valuable adjunct for the assessment of abdominal pain. With even a moderate amount of training and limited experience, emergency physicians can obtain sufficient skill to incorporate right upper quadrant (RUQ) ultrasound into their bedside exams and clinical decisions (1, 2, 3, 4, 5, 6). Most studies can be completed in <10 minutes (5). The current literature verifies that emergency ultrasound of the RUQ is accurate, improves time to diagnosis and treatment, decreases ED length of stay, and improves patient satisfaction (7, 8, 9). Ultrasound of the RUQ is included in the list of recommended applications for emergency ultrasound and is part of the model ultrasound curriculum of emergency medicine residency training programs (10).
CLINICAL APPLICATIONS
RUQ ultrasound is useful in assessing three common problems:
Right upper quadrant and epigastric pain
Jaundice
Ascites
There are four common practical applications for bedside ultrasound of the RUQ, including the detection of:
Gallstones
Cholecystitis
Dilated bile ducts and biliary obstruction
Ascites
Ultrasound can also potentially help in the search for a focal source of infection in patients who are septic, those with altered mental status and unreliable exams, and in the elderly or immunocompromised who may be less likely to have focal findings (11).
The liver is the major acoustic window to the abdomen. Familiarity with the liver and its surrounding structures will open up a variety of applications for abdominal scanning beyond those listed here. As clinicians become proficient in RUQ scans, they will likely become more confident in the Focused Assessment by Sonography for Trauma (FAST) exam (to assess for free fluid in Morison’s pouch) and in the scan of the proximal abdominal aorta (to detect aneurysms and dissections). Although RUQ ultrasound is primarily focused on the liver, gallbladder, and biliary tree, it may incidentally reveal pathology in adjacent areas in the right kidney, pleural space, pancreas, and aorta.
GUIDE TO IMAGE ACQUISITION
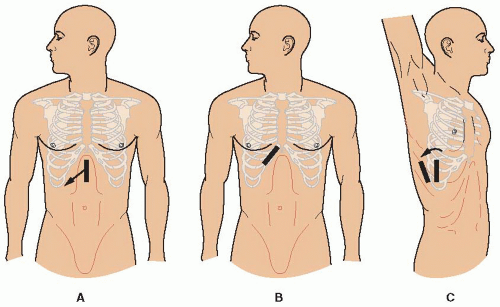
The liver, gallbladder, and biliary tree can be imaged from a number of approaches (subcostal, intercostal, and flank) with the patient in a variety of positions (supine, semirecumbent, erect, left lateral decubitus, and prone). The optimal technique will vary based on differences in anatomy, body habitus, and bowel gas patterns. Ideally, the sonographer should begin with a few standard approaches, modified and guided by both external and internal landmarks (Fig. 9.1).
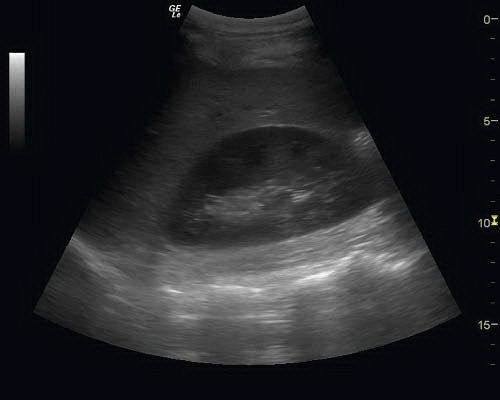
The subcostal approach is the most commonly used initial approach to imaging the gallbladder. Begin with the patient supine, and place the transducer in the midline at the epigastrium with the transducer oriented in the sagittal plane (Fig. 9.1A). If there is a large left hepatic lobe, the liver may be easily seen in this position. Leaving the transducer in the midline, tilt the transducer to project the sound wave toward the patient’s right side. In some cases, this will be sufficient to localize the gallbladder. If it is not seen, move the transducer down the costal margin while projecting it cephalad under the rib margin to scan through the dome of the liver. In many patients, the liver is mostly intrathoracic. In these patients, an improved image can be obtained by placing the transducer between the ribs (intercostal approach) (Fig. 9.1B). Alternatively, the patient can be positioned to bring the liver down below the costal margin. Have patients sit erect or semirecumbent, and instruct them to breathe deeply with their “belly out.” As the liver descends, the liver and gallbladder may be more easily imaged. If these maneuvers fail, move the patient to a left lateral decubitus position. This position brings the liver and gallbladder more toward the midline and closer to the transducer. Scan again from the subcostal approach, then continue to move the transducer along the costal margin toward the right flank. If the anterior subcostal approach is unsuccessful, leave the patient in a left lateral decubitus position, and scan through the right flank to identify the right kidney and Morison’s pouch (Fig. 9.1C). Once the right kidney is in view, the transducer should be angled slightly cephalad and anterior. The fundus of the gallbladder lies in close proximity to the right kidney and will often pop into view with this maneuver. Occasionally, it is useful to roll the patient from a left lateral decubitus position into a nearly prone position and scan from a subcostal approach. This position brings the gallbladder anterior. If heavy shadowing is seen from the gallbladder fossa, moving the patient prone may help the stones fall forward and make the echogenic stones more visible themselves, helping distinguish the shadows of a gallbladder packed with stones from artifact created by bowel gas (12).
If these external landmarks do not produce a good image, focus on obtaining the best possible acoustic window of the liver and follow internal landmarks. The portal triad and main lobar fissure (MLF) are useful landmarks that can be used to locate the gallbladder fossa. If the portal triad is used to define the center of a clock face, the gallbladder is usually found around 2 o’clock. The MLF can be seen as an
echogenic line joining the portal triad to the gallbladder. (See section on Anatomy.)
echogenic line joining the portal triad to the gallbladder. (See section on Anatomy.)
Regardless of how the image is obtained, once the gallbladder is identified, the entire organ should be scanned to fully visualize it. Gently rocking the transducer right and left, then rotating it 90 degrees to view both the long and short axis will produce a three-dimensional perspective. It is often necessary to manipulate the transducer to fully define the anatomy and pick up stones that may be obscured by the twists and turns common to many gallbladders.
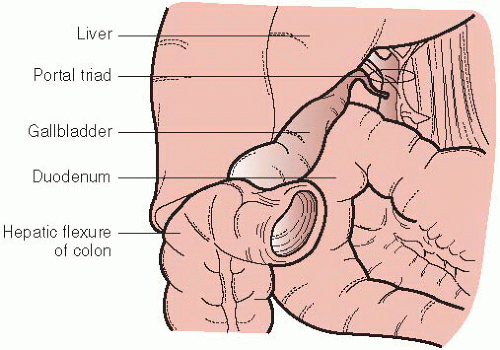
In general, the best ultrasound images are obtained when sound waves are directed perpendicular to the organ of interest in as direct a path as possible. Unfortunately, this approach may not always work for the gallbladder. From patient-to-patient there is considerable variation in the location and orientation of the gallbladder, and there are a number of acoustic barriers. For example, the transverse colon often rests immediately adjacent to the gallbladder, and the duodenum sweeps along its medial margin (Fig. 9.2). If the sound waves encounter bowel gas from either, shadowing will obscure the image. Most of the maneuvers described here are simply attempts to direct the ultrasound beam around these obstacles.
There are no consistent external landmarks or transducer positions that can adequately guide the emergency sonographer to reliably visualize the gallbladder in all patients. These guides are a starting point. Ideally, sonographers should use a systematic approach for scanning and modify their approach based on their experience and success.
NORMAL ANATOMY
The primary indication for a bedside RUQ ultrasound is to detect gallbladder disease as a potential source of pain. The novice may be tempted to focus solely on identifying the gallbladder and then be satisfied once its visualized. However, the RUQ is an anatomically complex area traversed by a number of vascular and ductal structures, most of which are well visualized by ultrasound. Even if the sonographer does not initially desire to identify this anatomy, the busy network of vessels and structures in the area will likely be distracting, if not confusing. Some sonographers have found that this region is more difficult than many applications of ED bedside ultrasound, but once mastered, their ability to explore the abdomen and their confidence in their results are greatly enhanced. A thorough and methodical review of this anatomy will improve the diagnostic utility of RUQ ultrasound.
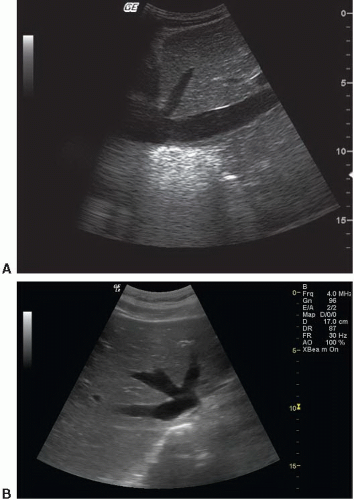
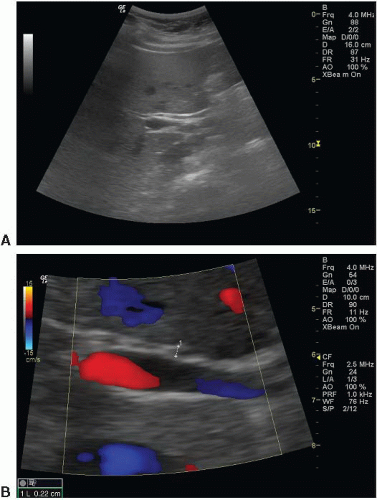
The Liver
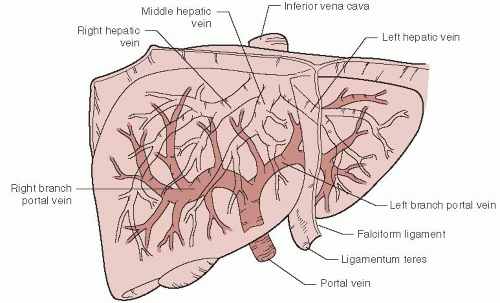
The liver is a major solid organ that serves as a good acoustic window to image most of the upper abdominal structures. A cross section of the liver reveals organized hepatocytes punctuated by branches of the bile ducts, hepatic artery, and hepatic and portal veins. The liver has a gray echotexture typical of solid viscera; the numerous vessels coursing through the organ give it a “salt-and-pepper” appearance, with areas of increased and decreased echogenicity scattered uniformly throughout (Fig. 9.3). The capsule of the liver appears brightly echogenic, especially in its border with the diaphragm. The major structures that are identifiable by ultrasound include the hepatic and portal veins, the hepatic arteries, and bile ducts (13). Figure 9.4 demonstrates a general outline of the major branches of the hepatic and portal venous structures.
Hepatic Veins
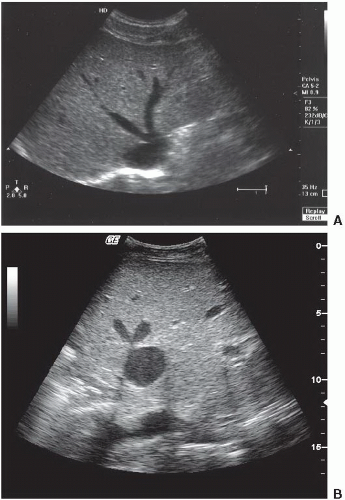
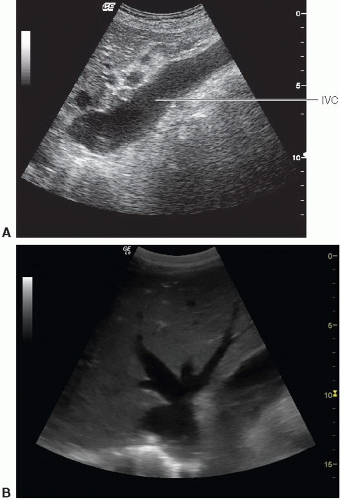
The liver is divided into anatomical lobes and segments by the hepatic veins (Fig. 9.4) (13). Three branches of hepatic veins arise from the inferior vena cava (IVC) just after it enters the abdominal cavity near the diaphragm (Figs. 9.4 and 9.5; eFig. 9.1). The middle hepatic vein divides the liver into anatomical right and left lobes and courses through the MLF. The right hepatic vein divides the right lobe of the liver into anterior and posterior segments; the left hepatic vein divides the left lobe of the liver into medial and lateral segments. The hepatic veins are thin, smooth-walled structures; the walls themselves are almost invisible to ultrasound. As the veins converge toward the vena cava, they sometimes look like rabbit ears; some have colorfully described their appearance as the “Playboy bunny sign” (Fig. 9.6). For the purposes of ED
ultrasound, the middle hepatic vein serves as a landmark for the MLF, a valuable guide to the gallbladder. The appearance of the hepatic veins and IVC can give indirect evidence of fluid status and cardiac performance. The vessels may be engorged and especially prominent in the face of fluid overload and/or elevated right heart pressures (Fig. 9.7). For experienced sonographers, the hepatic veins can help localize pathology to specific lobes or segments.
ultrasound, the middle hepatic vein serves as a landmark for the MLF, a valuable guide to the gallbladder. The appearance of the hepatic veins and IVC can give indirect evidence of fluid status and cardiac performance. The vessels may be engorged and especially prominent in the face of fluid overload and/or elevated right heart pressures (Fig. 9.7). For experienced sonographers, the hepatic veins can help localize pathology to specific lobes or segments.
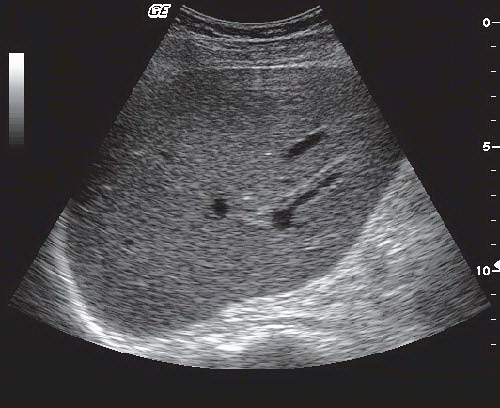 FIGURE 9.3. Sonographic Appearance of the Normal Liver. The liver has a uniform salt-and-pepper appearance created by the numerous vessels coursing through the parenchyma. |
Portal Veins
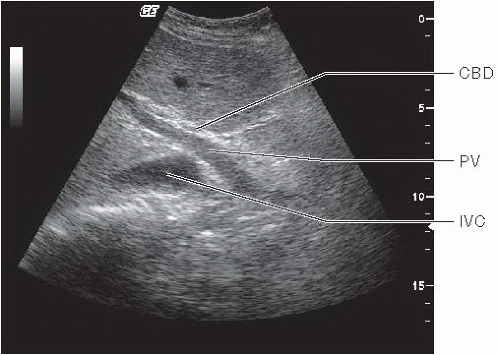
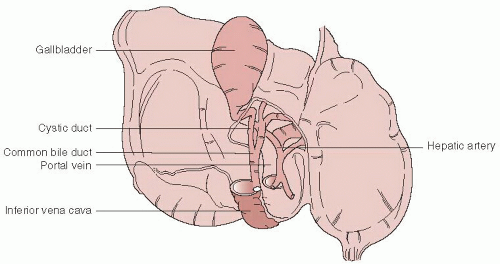
The portal vein forms the most recognizable part of the portal triad and is usually an easy landmark to identify in the liver. For the emergency sonographer, it helps to identify the common bile duct and gallbladder. The portal venous system returns blood from the intestines to the liver. The main portal vein is formed by the union of the splenic, inferior, and superior mesenteric veins. The splenic vein can be seen in a transverse section of the midline abdominal vasculature, where it courses just anterior to the superior mesenteric artery (Fig. 9.8; eFig. 9.2). In a plane transverse to the body, the long axis of the splenic vein is seen as a regular tubular structure that suddenly balloons out at the portosplenic convergence, formed when the inferior mesenteric vein joins it (14). The portosplenic convergence defines the origin of the portal vein. As the portal vein enters the liver, it lies just anterior to the IVC; this point defines the hilum of the liver (Fig. 9.9) (13). When the long axis of the main portal vein is viewed, the common bile duct can be seen to accompany it toward the porta hepatis (Figs. 9.9 and 9.10; eFigs. 9.3 and 9.4;  VIDEO 9.1). The normal common bile duct is barely visible as an irregular structure just anterior to the portal vein. The portal vein rapidly gives rise to two main branches, the right and left portal veins (Figs. 9.4 and 9.11). The right portal vein is the major landmark of the portal triad in the porta hepatis. The portal veins are characterized by bright echogenic walls that help distinguish them from other vessels in the liver. This peculiar echogenicity gives the appearance of a halo surrounding the portal venous vessels.
VIDEO 9.1). The normal common bile duct is barely visible as an irregular structure just anterior to the portal vein. The portal vein rapidly gives rise to two main branches, the right and left portal veins (Figs. 9.4 and 9.11). The right portal vein is the major landmark of the portal triad in the porta hepatis. The portal veins are characterized by bright echogenic walls that help distinguish them from other vessels in the liver. This peculiar echogenicity gives the appearance of a halo surrounding the portal venous vessels.
 VIDEO 9.1). The normal common bile duct is barely visible as an irregular structure just anterior to the portal vein. The portal vein rapidly gives rise to two main branches, the right and left portal veins (Figs. 9.4 and 9.11). The right portal vein is the major landmark of the portal triad in the porta hepatis. The portal veins are characterized by bright echogenic walls that help distinguish them from other vessels in the liver. This peculiar echogenicity gives the appearance of a halo surrounding the portal venous vessels.
VIDEO 9.1). The normal common bile duct is barely visible as an irregular structure just anterior to the portal vein. The portal vein rapidly gives rise to two main branches, the right and left portal veins (Figs. 9.4 and 9.11). The right portal vein is the major landmark of the portal triad in the porta hepatis. The portal veins are characterized by bright echogenic walls that help distinguish them from other vessels in the liver. This peculiar echogenicity gives the appearance of a halo surrounding the portal venous vessels.Hepatic Artery
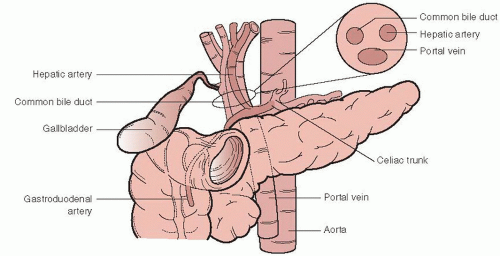
The hepatic artery (usually) originates as a branch off the celiac trunk. The main hepatic artery branches into the gastroduodenal artery and the proper hepatic artery. The gastroduodenal artery follows the course of the C-loop of the duodenum and defines the head of the pancreas. The proper hepatic artery ascends toward the porta hepatis to join the portal vein in the portal triad (Fig. 9.12). Its value in ED ultrasound is limited. For experienced sonographers it can be used to localize the pancreas (15).
Bile Ducts
The hepatocytes are drained by tiny biliary radicles that converge toward the porta hepatis. Eventually, they drain into the common hepatic duct. Just before the portal triad, the common hepatic and cystic ducts join to form the common bile duct. Common bile duct stones and pancreatic head tumors can obstruct outflow from the common bile duct, resulting in an enlarged duct. A dilated common bile duct is the hallmark of obstructive jaundice.
Bile ducts follow the path of the portal venous system throughout the liver. In routine scans of the liver the peripheral biliary radicles are typically not visualized unless they are enlarged. The larger common bile duct can be identified at the portal triad. If a transverse section is obtained through the portal triad, the common bile duct is seen just anterior to and to the right of the portal vein (Fig. 9.12). The diameter of the common bile duct is much smaller than the main portal vein, and is often almost imperceptible. When the portal vein is viewed in its long axis, the common duct can be seen to accompany it in its course toward the duodenum. It may be difficult to see if it is not enlarged, but it can be appreciated by the irregular beaded appearance it gives just anterior to the main portal vein (Fig. 9.10; eFigs. 9.3 and 9.4;  VIDEO 9.1).
VIDEO 9.1).
 VIDEO 9.1).
VIDEO 9.1).Gallbladder
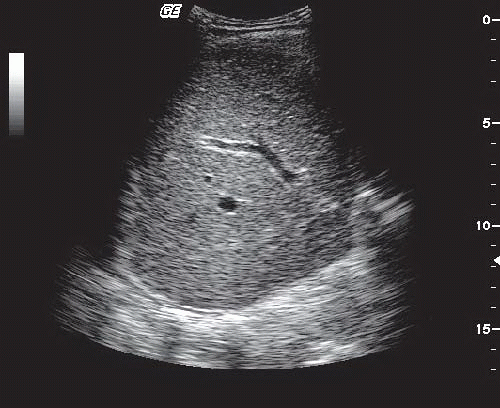
The gallbladder is a pear-shaped cystic structure that occupies the region between the right and the left lobes of the liver and typically lies on the inferior surface of the liver (Fig. 9.13). The normal gallbladder has the typical sonographic features of a cyst:
The lumen is an echo-free space, bounded by
Smooth regular walls, with
Posterior wall enhancement (more echogenic than surrounding tissue), and
Increased “through-transmission.” (The region immediately behind a simple cyst appears more echogenic than surrounding tissue. This artifact is created as the sound waves hit the interface between liquid and solid media.)
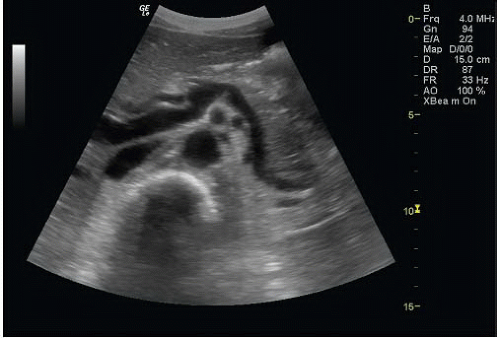
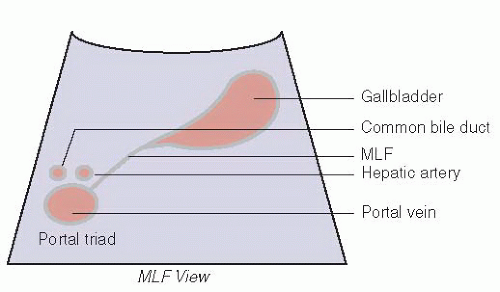
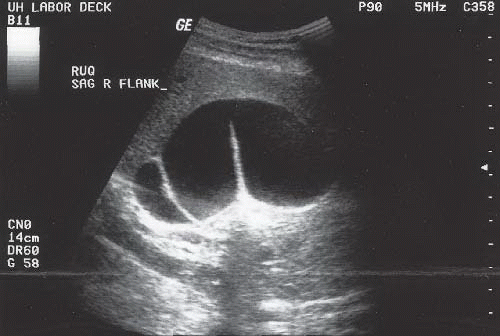
When a longitudinal or long axis view of the gallbladder is obtained, it appears to be connected to the portal triad by a visible echogenic line, the MLF. The MLF runs between the gallbladder and the IVC. The MLF View is a convenient view that defines much of the relevant anatomy for examinations of the gallbladder (Figs. 9.14 and 9.15; eFigs. 9.5-9.7). In that one view, abnormalities of the gallbladder and common bile duct can be seen.
There are a number of congenital variants in gallbladders. Gallbladders may have folds, internal septums, and duplications. It is important to explore the full dimensions of the gallbladder and cystic duct to avoid missing stones. Folds, twists, turns, and septums complicate imaging of the gallbladder by creating shadows and artifacts that can mimic
stones. Small stones can hide in these regions as well. The sonographer will need to view each turn of the gallbladder in two dimensions to distinguish between shadows created by anatomical structures from those caused by stones (Figs. 9.16 and 9.17; VIDEO 9.2).
VIDEO 9.2).
stones. Small stones can hide in these regions as well. The sonographer will need to view each turn of the gallbladder in two dimensions to distinguish between shadows created by anatomical structures from those caused by stones (Figs. 9.16 and 9.17;
 VIDEO 9.2).
VIDEO 9.2).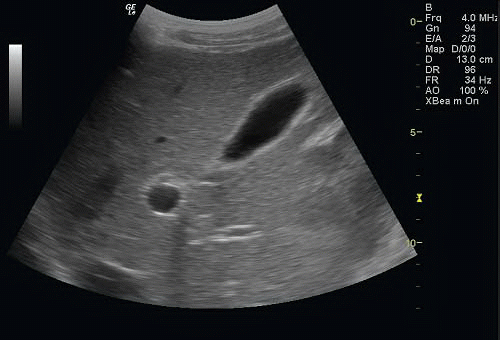 FIGURE 9.14. Normal Gallbladder. The gallbladder, main lobar fissure (MLF), and portal vein (PV) are seen. A tear-shaped gallbladder points toward the MLF and portal triad. |
Occasionally, the gallbladder may not be visualized. Agenesis of the gallbladder has been described, but is rare. Most likely, the scan is simply inadequate. Formal ultrasound protocols request a fasting state to minimize bowel gas and optimize gallbladder distention. The sonographer should recognize the limitations of bedside scans in the unprepped patient and be willing to declare the exam “indeterminate.”
Morison’s Pouch
The interface between the liver and the right kidney can be visualized from a flank approach. This potential space, Morison’s pouch, is an area where free fluid may accumulate. A view of Morison’s pouch is useful when looking for free intra-abdominal fluid, either from ascites or intra-abdominal hemorrhage (Fig. 9.18).
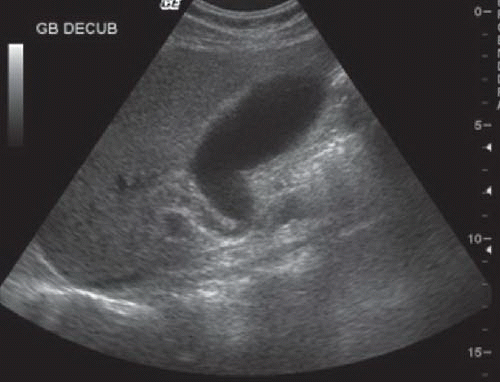 FIGURE 9.16. This Normal Gallbladder Takes a Sharp Turn as it Empties into the Cystic Duct. Such curves and twists can create shadows, as well as serve as sites where stones can become lodged. |
Standard Views of the Right Upper Quadrant
A few specific views define most of the anatomy relevant for the focused bedside exam of the RUQ. A longitudinal cut through the long axis of the gallbladder should include a view of the MLF and portal triad (Figs. 9.14 and 9.15). A second view through the short axis of the gallbladder should be obtained. The emergency sonographer should acquire a minimum of two views perpendicular to each other for any organ of interest, then scan from side to side. This creates a three-dimensional view of the object in the mind’s eye.
Before completing the examination of the gallbladder, the portal triad should be examined. The portal vein, hepatic artery, and common bile duct are all viewed in their transverse orientation in the portal triad, as shown in Figure 9.15. The normal portal triad looks something like Mickey Mouse, with the portal vein making up Mickey’s face, his ears formed anteriorly by the hepatic artery on the left and the common bile duct on the right (Fig. 9.12 inset). In the normal portal triad, the “ears” are symmetrical. If they are not symmetrical, a more detailed exam should be done to measure the common bile duct and trace its path back toward the duodenum looking for a source and site of obstruction. In order to better visualize the common bile duct, the sonographer first identifies the portal vein in transverse orientation, then twists the probe to obtain a longitudinal view. When the portal vein is viewed in its long axis, the common bile duct should be seen just anterior to it. The normal common duct will be barely visible as it travels alongside the portal vein and sometimes has a beaded irregular appearance (Fig. 9.10). The normal common bile duct measures <6 mm in cross-sectional diameter. Although the hepatic artery occupies the portal triad, it ascends in a different plane than the portal vein and bile duct and tends to disappear when the long axis of the portal vein is viewed. Sometimes, the common duct can be seen to loop over the hepatic artery in its course toward the duodenum.
Although it is helpful to recognize the major structures of the liver described above, it is not necessary to identify each of them in every exam. The ability to recognize the normal hepatic architecture can help to improve the quality of the
study. Sonographers who are familiar with the anatomy of the liver, biliary tract, and abdominal vasculature will likely be less distracted or confused by anatomical details, able to recognize subtle variations from normal, and better able to complete definitive exams in a timely manner.
study. Sonographers who are familiar with the anatomy of the liver, biliary tract, and abdominal vasculature will likely be less distracted or confused by anatomical details, able to recognize subtle variations from normal, and better able to complete definitive exams in a timely manner.
PATHOLOGY
Cholelithiasis
The most common ED application for a scan of the RUQ is for detection of gallstones in patients suspected of having biliary colic or cholecystitis. Gallstones have four sonographic features (11,16).
They are echogenic structures within the usual echo-free gallbladder lumen. Most are round, curvilinear, or multifaceted in shape. They range in shape from just a few millimeters to over a centimeter in size.
They create acoustic shadows. The typical gallstone shadow is described as “clean,” meaning black with well-defined, discrete margins. Since the usual space behind the gallbladder has enhanced echogenicity, the shadow created by a stone is pronounced. In contrast, shadows created by artifact and bowel gas are described as “dirty,” meaning they are grayish and poorly delineated. Bowel gas, in particular, scatters the ultrasound beam, creating a snowstorm of grayish artifact with poorly defined margins. Classically, stones were believed to create shadows because they contain calcium. In fact, the shadow created by a stone is more dependent upon the size of the stone than on its mineral content. Very small (1 to 3 mm) stones may not create shadows and are one source of false-negative scans (17).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree