2.1 Scenario 1: Early Failure of UAE
Vignette—LK is a 43-year-old woman who works as a college professor. She has a 10-year history of increasing menorrhagia and pressure symptoms. Physical examination and MRI show an 18–20-week uterus almost completely occupied by 2 or 3 large fibroids which show homogeneous global enhancement. Endometrial biopsy is benign.
At UAE both uterine arteries were catheterized and embolized with a total of 12 ml of calibrated hydrogel microspheres (8 ml to the left uterine artery, 4 ml to the right uterine artery), achieving the desired endpoint1. The entire uterus was demonstrated during embolization. Her recovery was uneventful, with return to full activity levels within 1 week.
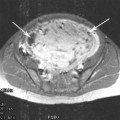
She was seen in the office 4 months after the UAE for follow-up. Her menstrual flow remained very heavy and she continued to have significant pressure symptoms, both essentially unchanged from before the UAE. MRI showed no change in uterine/fibroid size with minimal infarction of fibroids.
A woman who has had no improvement in her fibroid-related symptoms after embolization represents a clinical failure of the procedure. A woman who has an initial response to UAE and recurrence of symptoms within a short term (3–12 months) represents an early failure of the procedure. When evaluating these patients the first question that needs to be answered is whether or not the initial procedure was technically successful. Were both uterine arteries identified and selectively catheterized? Was the desired endpoint reached? Were adequate doses of embolic agent given? Was there a complete “uterogram”—was the entirety of the expected volume of the uterus seen during embolization?
If the answer to any of these questions is “no” then the first procedure should be considered a technical failure. Repeat arteriography and re-embolization to redress the technical problem with the procedure is appropriate. Technical failure of UAE should be a rare event, below 2% (Worthington-Kirsch et al. 2005). Overall, about 90% of patients experience at least short-term relief from symptoms (Spies et al. 2005). The causes of clinical failure in patients who have had technically successful procedures include incorrect diagnosis for the cause of the patient’s symptoms, unrecognized under embolization, sarcoma, and other causes which are yet to be defined.
If the first procedure was apparently technically adequate, then a contrast-enhanced MRI of the uterus is needed to decide on a course of treatment. If the MRI shows that all visible fibroids are globally infarcted, there is no indication for a repeat embolization. This suggests that the fibroid disease is not the cause of the patient’s symptoms and another etiology needs to be considered. These patients should be referred to their gynecologist for further evaluation and management.
If the MRI shows that there has been partial infarction of the fibroids, then the embolization was probably inadequate. The uterine arteries may have been under embolized (due to poor choice of endpoint or spasm), or there may be accessory supply to the fibroids. This is most commonly from the ovarian artery. The pattern of fibroid infarction/preservation of flow may suggest which of these is responsible.
If the patient has had no improvement in symptoms after UAE despite what appears to be a technically adequate embolization and MRI shows no significant fibroid infarction (less than 10% of the overall fibroid burden), a repeat embolization should not be performed. There have been at least two reports of uterine leiomyosarcoma in this setting (Common et al. 2001; Papadia et al. 2007). In these cases it is important to explain to the patient that the risk of her having a malignancy is high enough that she needs to have a surgical procedure, which will most likely be hysterectomy. The author has referred two patients for hysterectomy under these conditions (out of a total of over 2,700 UAE procedures). In both cases no sarcoma was found. The reason for noninfarction of the fibroids in these patients is not clear.
Some would argue that a repeat UAE may be useful in this situation. It is true that many patients in this situation will not have a diagnosis of sarcoma after surgery. However, if the patient has a sarcoma the embolization and follow-up period could be interpreted as a 3-month (or longer) delay in diagnosis. It would be imprudent to delay the diagnosis by another 3–4 months or longer by attempting a repeat UAE.
Two of the three alternatives in this scenario require that the patient be referred back to her gynecologist for further management. It is essential to keep open communications between the IR and the gynecologist so that referrals like this can be managed in an efficient and collegial manner. The author personally makes every effort to speak directly with the gynecologist by telephone in addition to sending the relevant office notes, ideally calling and speaking with the gynecologist while the patient is still in the office and can listen to or participate in the discussion.
Vignette (continued) —After explaining the situation to her, I called Ms K’s gynecologist while she was still in the office and reviewed the case. I explained to both the patient and her primary gynecologist that I did not think that this was a sarcoma, but that the risk of it being one was such that I did not think a nonsurgical procedure was wise. Ms K was referred to a gynecologic oncologist, who performed a TAH. The final pathology report was fibroids with no histologic evidence of sarcoma.
2.2 Scenario 2: Late Failure of Symptom Control
Vignette—FA had UAE in 1998, at age 35. She did well after the UAE, with complete resolution of symptoms. She was seen in follow-up at 3 months and 1 year post-UAE, after which she chose not to come for annual follow-up visits.
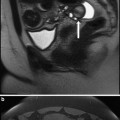
At age 46 she began to have recurrent menorrhagia and some urinary pressure. She came to the office 18 months after her menses became noticeably heavier. MRI revealed a 14–16 week-sized uterus with multiple enhancing fibroids.
The patient who has an initially good response to UAE and then experiences recurrent symptoms (either recurrent menorrhagia or bulk/pressure symptoms) in the medium to long term (arbitrarily more than 12 months) usually does so because of either an inadequate embolization or growth of new fibroids. It is important to recognize that menorrhagia may also develop because of pathology different from fibroids.
Repeating the contrast-enhanced MRI when symptoms recur is essential to making the diagnosis and planning treatment. The MRI is used to determine the extent and location of perfused fibroids and guide arteriography. This can provide information regarding the presence of collateral flow, especially from the ovarian arteries. The ovarian arteries typically will supply the fundal portion of the uterus. MRA can also define the ovarian arteries (Kirby et al. 2011).
Ideally, all patients have had a routine follow-up MRI done at 3–6 months post embolization. This is useful to define the extent of fibroid infarction or lack thereof and to advise the patient regarding the likelihood of symptom recurrence. If the MRI shows global fibroid infarction, it appears that the likelihood of recurrence is lower and that the clinical efficacy should be more durable than in those patients who have some preservation of enhancement in their fibroids.
It is important to note that if the follow-up MRI shows persistent fibroid perfusion the decision to intervene depends on how the patient is doing clinically. The imaging findings of persistent perfusion are not in and of themselves justification for a repeat arteriogram/embolization.
The decision tree for late recurrence is similar to that for early recurrence, with the exception of the patient who shows global fibroid enhancement. If the patient has had a good response to UAE for over a year and now has globally enhancing fibroids, repeat UAE is indicated.
Vignette (continued)—Ms A had a second UAE, receiving 1.5 ml of calibrated hydrogel microspheres to the left uterine artery and 6 ml of microspheres to the right uterine artery. Her recovery was uneventful, with return to full activity levels in 9 days. Since then she has had complete relief from her menorrhagia and pressure symptoms.
3 Technique for Repeat UAE
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree