Dilated cardiomyopathy (DCM) is defined as a disease of the myocardium characterized by left ventricular dilatation and systolic impairment that cannot be exclusively explained by abnormal loading conditions (such as hypertension or valvular heart disease) or coronary artery disease. The true prevalence is debated because of a lack of large contemporary population studies. The original Olmsted County study, performed between 1975 and 1984, estimated the prevalence to be in the region of 1 in 2700 individuals. However, the calculated prevalence of hypertrophic cardiomyopathy in the same study has since been shown to be a gross underestimate, possibly explained by the fact that echocardiography was still a developing technique. Recent reports have estimated the prevalence to be closer to 1 in 400 people in the United States. Nevertheless, DCM is a commonly encountered condition, representing the most frequent indication for cardiac transplantation and a common cause of heart failure and sudden cardiac death (SCD). Despite therapeutic advances, 3-year treated mortality rates are estimated to be 12% to 20%. Definitive early investigation giving a prompt and accurate diagnosis is therefore essential for the expedient introduction of targeted therapy. We will discuss the benefits of cardiovascular magnetic resonance (CMR) in the investigation of DCM after a brief overview of our current understanding of the disease.
Background
DCM represents the final common phenotype of a diverse range of genetic and acquired insults ( Table 31.1 ). In 20% to 35% of cases, at least one first-degree relative is affected; in 20% to 40% of cases, a causative genetic mutation can be demonstrated with modern techniques. Mutations in over 50 genes have now been linked with the disease, the majority of which occur in autosomal genes. In a small proportion of cases the mutations are associated with broader syndromes, most commonly neuromuscular disorders such as Duchenne muscular dystrophy. Inheritance is generally autosomal dominant, although often marked by reduced penetrance and variable expressivity. In contrast to hypertrophic cardiomyopathy, mutations associated with DCM occur in a diverse range of genes responsible for many different cellular functions. The most common mutations occur in genes encoding sarcomeric proteins, with mutations found less commonly in genes responsible for the function of ion channels, the cytoskeleton, and the nuclear envelope (see Table 31.1 ).
| Genetic a | Acquired |
|---|---|
| Sarcomeric | Toxins |
| TTN (25%, titin) MYH6 (4%), MYH7 (4%) (myosin heavy chain) TNNC1 (<1%), TNNT2 (3%), TNNI3 (<1%) (troponin) MYPN (3%–4%, myopalladin) Nuclear Envelope LMNA (6%, lamin A/C) Cytoskeleton DMD (N/A, dystrophin) DES (<1%, desmin) Ion Channels SCN5A (2%–3%, sodium channel protein type 5 subunit) Mitochondrial TAZ (NA, tafazzin) b Sarcoplasmic Reticulum PLN (<1%, phospholamban) | Chemotherapy (anthracyclines, monoclonal antibodies) Alcohol Recreational drugs (cocaine, amphetamines, anabolic steroids) Infectious Insults Viral myocarditis (parvovirus, human herpes virus, Coxsackie) HIV Chagas disease (Trypanosoma cruzi) Peripartum Autoimmune Giant cell myocarditis Multisystem disease (systemic lupus, Churg-Strauss) Endocrine Pheochromocytoma Hypo- and hyperthyroidism Iron Overload |
a Gene listed followed by prevalence and protein encoded in brackets.
Truncating variants of the large titin gene, TTN , are the most common mutations causing DCM. Titin is the largest protein in the human body, spanning the length of the sarcomere, and it acts to generate and regulate contractile force. Advances in genetic sequencing have enabled more detailed study of TTN mutations and their role in DCM and other cardiac pathology. Truncating variants of TTN have now been identified in 25% cases of familial DCM, 18% of sporadic cases and <1% of unaffected controls. Mutations in the LMNA gene, which encodes the lamin A/C protein, part of the nuclear envelope, are also associated with DCM. These mutations are characterized by a highly penetrant and malignant form of the disease that requires aggressive treatment at an early stage given high rates of sudden death and advanced heart failure. Aside from variants in LMNA , the identification of DCM disease-associated mutations holds most significance for relatives of the proband, enabling cascade screening and discharge from follow-up if found to be mutation carrier negative. Cascade screening and the identification of mild disease in asymptomatic individuals enables early diagnosis, disease monitoring, and appropriate intervention. There is also huge opportunity for targeted genetic-based interventions with the development of gene editing techniques.
The most common acquired causes of DCM include exposure to toxins such as excess alcohol and cardiotoxic chemotherapies. The toxic effects of these agents appear to be dose-dependent and cardiac dysfunction often resolves after toxin removal. A previous episode of viral myocarditis is another common cause and is thought to evolve into DCM in up to 30% of cases. Less common, noninfective autoimmune inflammatory conditions can also present with a DCM phenotype. Given the heterogeneity of response to these environmental insults, it appears likely that individual susceptibility is linked to genetic factors.
Peripartum cardiomyopathy (PPCM) is a rarer form of the disease characterized by the development of a DCM in the last trimester of pregnancy or in the first 6 months postpartum. Many studies have linked the development of this condition to an abnormally cleaved segment of prolactin which is toxic to cardiomyocytes. A strong genetic component to the condition has, however, also been demonstrated. In one study, women with PPCM were found to have a similar burden of genetic variants, particularly in TTN (15% of the cohort), compared with a population with idiopathic DCM. Similarly, undiagnosed DCM has been found to be more common in first-degree relatives of patients with PPCM. This neatly demonstrates that PPCM and DCM have a common genetic etiology, which may be unmasked in the presence of specific environmental triggers.
In summary, DCM is the result of a complex interplay between genetic abnormalities, such as variants in TTN , and environmental factors including hemodynamic, inflammatory, and toxic insults. The interaction between these factors may help to explain the variable penetrance and reduced expressivity of mutations and the heterogeneous response of different individuals to environmental insults.
Treatment
The current treatment strategies for dilated cardiomyopathy focus on the use of neurohormonal medical therapies and cardiac resynchronization therapy to treat and prevent heart failure, and implantable cardioverter defibrillators (ICDs) to prevent sudden cardiac death from malignant ventricular arrhythmia. Evidence strongly supports the use of neurohormonal therapies such as beta-blockers and angiotensin-converting enzyme inhibitors in patients with reduced left ventricular ejection fraction (LVEF), and cardiac resynchronization therapy in patients with reduced LVEF and prolonged QRS duration. Data on the use of primary prevention ICD therapy in DCM are, however, slightly less convincing. Current guidelines recommend consideration of ICD therapy in patients with severely depressed ejection fraction, although this single-criterion approach lacks sensitivity and specificity. In clinical trials investigating the benefit of ICD therapy in patients with severely reduced LVEF, only 5% of patients received appropriate therapies per year. This demonstrates that the majority of patients currently receiving primary prevention devices on the basis of guidelines do not gain benefit. Conversely, large population studies have shown that 70% to 80% of SCD sufferers do not have a severely reduced LVEF. Additional parameters, which identify patients at risk of SCD, will allow us to improve the selection of patients for ICD therapy. We discuss the potential of CMR techniques in risk stratification.
Cardiovascular Magnetic Resonance Assessment of Dilated Cardiomyopathy
Morphology and Function
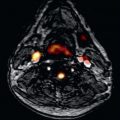
Diagnosis and subsequent management of patients with DCM relies on detailed assessment of left ventricular morphology and function. LVEF is currently the sole arbiter in the selection of patients for device therapy; therefore precise measurement is crucial. CMR allows accurate and reproducible assessment of LV volumes, mass, and ejection fraction without the need for geometrical assumptions and is therefore considered the gold standard noninvasive technique ( Fig. 31.1 ). Analysis of regional function and myocardial strain can also be assessed using myocardial tissue tagging and feature tracking. Analysis of longitudinal strain using myocardial feature tracking has been shown to predict adverse outcomes, independently of other predictors such as LVEF and late gadolinium enhancement (LGE), in patients with DCM. Analysis of wall thickening and end-systolic wall stress and visualization of impaired fiber shortening can also be performed.

Right ventricular (RV) size and function is abnormal in between 30% and 60% of cases of DCM. This is thought to be secondary to intrinsic myocardial dysfunction and increased afterload related to a rise in pulmonary vascular resistance. CMR provides the gold standard noninvasive assessment of both RV size and function because of its three-dimensional capabilities. Accurate assessment can be challenging using other forms of imaging, such as echocardiography, because of its complex and variable shape. Reduced RV ejection fraction on CMR is an independent predictor of all-cause mortality and adverse heart failure outcomes. This supports a role for its use in prognostication of patients with DCM.
CMR also allows accurate quantification of left atrial (LA) volume using the biplane area-length method ( Fig. 31.2 ). This compares favorably against other noninvasive imaging methods because of its excellent endocardial border definition and multiplanar imaging ability, even in the presence of atrial fibrillation. LA size is often increased in cases of DCM secondary to pressure overload from LV diastolic impairment, functional mitral regurgitation, and atrial fibrillation. It has been proposed that the degree of LA enlargement acts as a barometer of diastolic dysfunction and, consequently, there has been interest in the use of LA size to predict heart failure outcomes. Indeed, it has been demonstrated that indexed LA volume calculated using CMR independently predicts cardiac transplant-free survival in DCM. A cutoff value of >72 mL/m 2 has been shown to predict a 3-fold increase in adverse outcomes in patients with DCM.

Functional mitral regurgitation is also a common consequence of DCM secondary to mitral annular dilatation and leaflet tethering secondary to LV impairment. A long-axis cine stack and a short-axis cine image across the valve allows accurate assessment of all parts of the valve apparatus, including individual leaflet scallops, chordae, and papillary muscles. Mitral regurgitant volume can be calculated by estimating the aortic forward flow volume, using phase contrast flow imaging, and subtracting this from the total LV stroke volume. This method has been validated against volumes calculated from echocardiographic indices and catheterization data with good intertechnique agreement. Once again, the accurate assessment of the degree of functional mitral regurgitation provides important prognostic information in DCM.
Given the accuracy in functional assessment, CMR has been proposed as the method of choice for the follow-up of patients with DCM after pharmacologic and surgical intervention. Given the favorable interobserver variability compared with other methods of assessment, the use of CMR in clinical trials can reduce the sample size required, reducing the overall cost and time needed to complete the research. Moreover, it may be possible to avoid repeated studies using less precise methods, which are inconsistent. More precise adjustment of therapy and reduction of admission for repeat studies are likely to overcome the additional costs of a CMR study.
Tissue Characterization
Apart from accurate and reproducible assessment of cardiac morphology and function, the major advantage of CMR in the assessment of DCM is its ability to perform tissue characterization using LGE. This allows the detection and quantification of myocardial fibrosis. We also discuss the potential role of the more recently developed T1 mapping technique, the use of which is currently confined to research.
Fibrosis
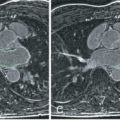
One of the histologic hallmarks of DCM, common to all causes of heart failure, is myocardial fibrosis. There are two main forms of fibrosis detected histologically: interstitial fibrosis and replacement fibrosis ( Fig. 31.3 ). Interstitial fibrosis describes an increase in the collagen volume fraction with expansion of the extracellular matrix, whereas replacement fibrosis describes discrete areas of myocardial scarring resulting from myocyte cell death. Fibrosis is promoted through activation of the renin–angiotensin–aldosterone and the beta-adrenergic axes, both consequences of heart failure. Injurious stimuli and toxins also play an important role by activating inflammatory cascades, leading to the production of reactive oxygen species. These pathways result in activation of myofibroblasts, with upregulation of transforming growth factor beta, altered activity in matrix metalloproteinases, and, ultimately, the production of collagen.

Fibrosis is associated with adverse ventricular remodeling and increased all-cause mortality. It has also been shown to provide an important substrate for the maintenance of re-entry ventricular arrhythmias. An electroanatomical mapping study demonstrated that inducible ventricular arrhythmia and a history of sustained ventricular tachycardia (VT) only occurred in those patients with replacement fibrosis on LGE CMR. Additionally, in each of the cases with inducible arrhythmia, its origin was mapped to the location of the LGE on CMR. Fibrosis has also been associated with fractionated electrograms, slowed conduction, and conduction block during electrophysiology studies. Each of these abnormalities has been associated with an increased risk of sustained VT and ventricular fibrillation. The combination of fibrosis interspersed with areas of surviving myocardium has been correlated with the generation of re-entry wavefronts. Moreover, the targeting of isthmuses of surviving myocardium has been shown to eliminate ventricular arrhythmia. The combination of fibrosis and areas of viable myocardium has therefore been proposed to act as a substrate for re-entry arrhythmia. All of these observations strongly support a role for fibrosis in the generation of ventricular arrhythmia.
Noninvasive detection of fibrosis using CMR therefore provides an opportunity to identify patients with DCM at high risk of sudden arrhythmic death. Treatments targeted at preventing or reversing fibrosis also provide important future therapeutic possibilities.
Late Gadolinium Enhancement Cardiovascular Magnetic Resonance and Midwall Replacement Fibrosis
LGE CMR identifies midwall enhancement in around 30% of patients with DCM, typically occurring in a linear distribution in the septum (see Fig. 31.3 ). Histologic validation has confirmed that this pattern of enhancement represents replacement fibrosis. The mass of fibrosis can be quantified using semiautomated software and validated methods. The most commonly used methods are the full width at half maximum (FWHM) and the >2 standard deviation (>2 SD) approach. The FWHM method quantifies regions of myocardium with a signal intensity >50% of the maximally enhanced region, whereas the >2 SD approach includes regions with a signal intensity >2 SD above the signal intensity of a reference area of normal myocardium.
Given the suboptimal sensitivity and specificity of current LVEF-based criteria for sudden death risk stratification, there has been interest in the incremental value of adding the presence and extent of mid-wall fibrosis, as determined by LGE CMR, to the model. The largest study to date reported all-cause mortality and SCD/aborted SCD rates of 27% and 30%, respectively, in patients with midwall fibrosis, compared with 11% and 7% in patients without fibrosis. Multivariable analysis confirmed that the presence of midwall fibrosis was an independent predictor of all-cause mortality and SCD/aborted SCD. The adjusted hazard ratio (HR) for the SCD composite endpoint was 4.6 in those patients with fibrosis ( P < .001), whereas the adjusted HR for every 1% increment in the mass of fibrosis was 1.1 (95% confidence interval [CI] 1.05–1.16; P < .001). The same study demonstrated that the addition of mid-wall fibrosis to an LVEF-based strategy improved overall risk stratification. This finding has been replicated in similar studies and a large meta-analysis. It has also been demonstrated that LGE quantification by both the FWHM and 2 SD methods provides robust prognostication for the prediction of adverse events. It has been demonstrated that an LGE extent of >6.1% by 2 SD and >4.4% by FWHM predicts adverse events with the greatest sensitivity and specificity.
Altogether, current evidence strongly supports a role for LGE CMR in improving the selection of patients who may benefit from ICD therapy, by identifying those patients at highest risk of adverse arrhythmic outcomes. LGE CMR appears to add robust incremental value to the current LVEF-based approach. The added value of LGE mass quantification appears less convincing, possibly because of interobserver and intraobserver variability. Another explanation may be that, rather than the overall mass of fibrosis, it is the size of the border between areas of fibrosis and surviving myocardium that is most relevant to overall arrhythmic risk. As discussed, isthmuses of surviving myocardium within fibrotic areas appear to play an important role in the generation of re-entry wavefronts. Therefore the size of the area where these two components interact may reflect arrhythmic risk more accurately.
Confirming the Diagnosis
The use of LGE CMR is also key to confirming the diagnosis of DCM in suspected cases. A study investigating the use of LGE CMR in patients with a suspected diagnosis of DCM, based on angiographic and echocardiographic findings, demonstrated that, in fact, 13% of patients had subendocardial enhancement indicating previous myocardial infarction. This demonstrates that coronary angiography misdiagnoses a proportion of patients as having a nonischemic etiology when in fact they have suffered previous asymptomatic infarction. It is recognized that around 25% of patients with myocardial infarction do not present to hospital. A proportion of these patients have unobstructed coronary vasculature on angiography, presumably with infarction secondary to embolic phenomenon or plaque rupture with subsequent re-canalization (see Fig. 31.4E ). This leads to the subsequent incorrect diagnosis of a nonischemic etiology. The correct diagnosis of this subgroup of patients, mislabeled by coronary angiography, is crucial given the different clinical courses and management strategies with regards to ischemic and dilated cardiomyopathies. Subsequent to this, LGE CMR has been shown to be at least as sensitive and specific as invasive angiography in diagnosing the cause of LV impairment in patients presenting with heart failure. This demonstrated a 97% diagnostic accuracy for LGE CMR compared with a 95% diagnostic accuracy for coronary angiography. This supports the role of LGE CMR as the initial diagnostic test in patients presenting with heart failure and LV systolic impairment of uncertain etiology. Fig. 31.4 correlates the findings of LGE CMR and coronary angiography from the study, demonstrating the different possible combinations of findings from CMR and angiography and the subsequent diagnoses. LGE and T2* sequences also allow the diagnosis of other pathologies, such as sarcoidosis and myocardial iron overload, which can occasionally present with a DCM phenotype, requiring different management strategies, and which are not easily diagnosed using other imaging modalities. Sarcoidosis is discussed in further detail later.

Research Techniques
T1 Mapping and Interstitial Fibrosis
Recent advances in T1 mapping techniques now allow the direct quantification of T1 relaxation times of each myocardial voxel, enabling the construction of T1 maps. T1 mapping can be performed preadministration and postadministration of gadolinium contrast. Using precontrast and postcontrast T1 values and hematocrit measurement, the extracellular volume (ECV) fraction can subsequently be calculated. The extent of interstitial fibrosis has been shown to correlate well with ECV fraction and native T1 times. This has led to the possibility of quantifying the degree of interstitial fibrosis in DCM using a noninvasive technique. It has potential advances over the qualitative LGE technique, which relies on subjective interpretation. Moreover, given the fact that the LGE technique relies on regional differences, there is the potential to miss diffuse myocardial fibrosis, which can appear as “nulled” normal myocardium. T1 mapping also offers opportunities for monitoring the response to therapies with potential antifibrotic properties. Studies have reported elevated native T1 values and ECV fractions in DCM, compared with controls. Elevation of ECV in even mild phenotypes of DCM, compared with controls, has been demonstrated. This raises the possibility of using T1 mapping for the diagnosis of borderline cases.
A large study on patients with DCM has demonstrated that native T1 values independently predicted all-cause mortality and a composite of adverse heart failure outcomes. However, despite the association between outcome and native T1 values, it did not demonstrate an independent association between ECV and outcomes. This may be explained by heterogeneities in the methods of ECV calculation, including the timing at which postcontrast images were taken and also the timing of hematocrit measurement relative to the study. This demonstrates the need for standardized precise protocols for T1 mapping for future research and clinical practice.
Perfusion Imaging
Studies have demonstrated a reduction in myocardial blood flow in patients with DCM. Many theories have been proposed to explain this phenomenon despite visually normal epicardial coronary arteries. These mainly focus on dysfunction of the microvessels or increased oxygen diffusion distance because of interstitial fibrosis. The degree of myocardial blood flow impairment has been strongly correlated with prognosis. However, what has been less clear is whether abnormal perfusion is responsible for the adverse prognosis because of myocardial oxygen deprivation or is merely a marker of disease severity. A study using blood oxygen level-dependent CMR, however, has improved our current understanding of the pathophysiologic relevance. This study assessed myocardial oxygenation and myocardial perfusion reserve during adenosine stress in patients with DCM compared with controls. Although myocardial perfusion reserve was reduced in patients with DCM, compared with controls, oxygenation during stress was not significantly different. Moreover, resting cardiac energetics in patients with DCM were not affected by oxygen administration. This suggests that the perfusion deficit is not sufficient to cause a reduction in oxygenation during stress and also that the resting impairment in energy metabolism is not secondary to a myocardial oxygen deficit. This also indicates that the reduction in perfusion observed in DCM is merely a marker of disease severity rather than a significant pathophysiologic driver.
Metabolic Imaging
Investigation of myocardial energetics in DCM is largely confined to research. Magnetic resonance (MR) spectroscopy allows the level of myocardial adenosine triphosphate (ATP) and phosphocreatine (PCr) to be determined. Both compounds are involved in high-energy metabolism and a reduced ratio of PCr:ATP indicates a myocardial energy deficit. The use of MR spectroscopy therefore enables myocardial energetics to be assessed. In patients with DCM, the PCr:ATP ratio has been shown to strongly correlate with outcomes and therapies such as angiotensin-converting enzyme inhibitors have been linked with an improvement in the ratio. Studies on exercise training have also confirmed that although training improves LV function, there is no adverse effect on energetics with no change in PCr:ATP ratio.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree