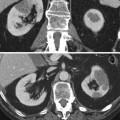
Patient in prone position
Insufflation of a small quantity of oxygen in the retroperitoneal space
Radiographic identification of the right kidney
Skin tracing on the back and right flank of the kidney position
Local anesthesia with novocaine 2 % in the tissues surrounding the inferior pole of the right kidney
Measurement of perirenal pressure induced by the retroperitoneal air
Radiographic control of the anesthesia needle location
Insertion of the biopsy needle sleeve
Biopsy of the renal tissue
Tissue fixation with formaldehyde 3 %
In case of bleeding injection of small quantities of hemostatic gel
Electron microscopy for diagnostic purposes was first applied also by Dr. Fiaschi’s group between 1955 and 1958, specifically by Naccarato and Andres, in collaboration with Swedish colleagues from the Karolinska Institute of Stockholm (Fogazzi and Cameron 1999). Finally, the same Italian group, in collaboration with investigators at Columbia University in New York, first applied immunofluorescence microscopy to renal biopsy tissue in 1957, the results of which were published by Seegal et al. (1959), a year before Freedman et al. (1960) and collaborators published what is considered by many the first article on the subject.
3 Clinical Indications for Renal Biopsy
In the following paragraphs, we will analyze the principal points of the decision algorithm that lead to renal biopsy. The indications for renal biopsy – with refinements of the histopathological techniques on the one hand and reduction of biopsy complications, thanks to real-time ultrasound guidance and to needle improvements, on the other – are constantly increasing. For practical purposes, we have divided the discussion in two sections – major indications, or those in which the biopsy is considered indispensable for the formulation of the diagnosis and the subsequent therapeutic strategy, and optional uses of the biopsy, the indications for which are still being defined.
3.1 Major Indications
3.1.1 Idiopathic Nephrotic Syndrome
The idiopathic nephrotic syndrome in the adult patient is the clinical situation that classically requires the performance of renal biopsy, which is justified by the fact that several histological entities can give rise to the syndrome in adults, each of which is associated with its own therapeutic protocols, differing from each other in terms of drugs, dosages, and duration of treatment. Richards et al. (1994) documented that renal biopsy, performed in adults with the nephrotic syndrome, significantly influenced the choice of therapeutic protocol in 86 % of the cases. On the other hand, conflicting opinions exist regarding the significance of histological findings for each single glomerular pathology. Regarding the nephrotic syndrome secondary to membranous glomerulopathy, some studies have indicated that the copresence of focal and segmental glomerulosclerosis (FSGS) is a negative prognostic indicator, both in terms of clinical response to standard therapy and of progression to renal failure (Dumoulin et al. 2003). Other studies, in contrast, have not found that FSGS or other histological variants of membranous nephropathy are as useful as clinical data in predicting the disease outcome (Troyanov et al. 2006). Regarding segmental glomerulosclerosis itself, numerous studies have stressed the importance of the histological characteristics of the biopsy obtained at the first signs of the disease. The presence of the cellular form, and its “collapsing” variant, indicates an inadequate response to conventional therapy and a faster progression towards end-stage renal disease (ESRD), in comparison with the classical histological variants including perihilar sclerosis and tip lesion (Stokes et al. 2006; Chun et al. 2004). The cellular variant is also highly predictive of segmental glomerulosclerosis recurrence posttransplant (Newstead 2003). Other, less frequent, diagnostic possibilities of the nephrotic syndrome may surprise the nephrologist as he or she reads the outcome of the biopsy, such as primary amyloidosis, fibrillary glomerulonephritis, membranous nephropathy with characteristics of lupus nephritis without the clinical or serological signs of systemic disease, and finally rare diseases with peculiar histological characteristics such as Fabry’s disease, collagen fibrotic glomerulopathy, and L-CAT (lecithin–cholesterol acyltransferase) deficiency nephropathy. In pediatric patients with the nephrotic syndrome, renal biopsy is not usually indicated since more than 90 % of these patients have minimal change glomerulopathy that usually responds to well-known corticosteroid protocols. Thus, renal biopsy in children is reserved for atypical presentations, such as the persistence of microhematuria, hypertension and low complement levels after 6 weeks of steroid therapy, and therapy failure, or for suspected congenital familial nephrotic syndrome.
3.1.2 Acute Renal Injury
In the absence of data clearly indicating the cause of acute renal failure (thus excluding cases with clear laboratory or radiological evidence of prerenal failure, obstruction, and acute tubular necrosis), renal biopsy becomes a fundamental tool not only for diagnosis but above all for prognosis and for determining the therapeutic protocol. One prospective study has shown that renal biopsy was essential in deciding the treatment and hence the outcome in 71 % of acute renal failure patients; the modification of the therapeutic strategy subsequent to the biopsy resulted in clinical benefits which far outweighed the risk of the biopsy (Kobrin and Madaio 1996).
3.1.3 Renal Allograft Dysfunction
The causes of renal allograft dysfunction correlate with the time from transplantation in which they are found; nevertheless renal biopsy can be essential for determining the diagnosis and the treatment choices.
The failure of the kidney to function immediately following transplantation is termed delayed graft function, which is formally defined as the persistence of oliguria or the need for dialysis in the first week posttransplant. Apart from urinary tract obstruction, caused by ureteral necrosis or obstruction, or from thrombosis of the renal artery or vein which can be diagnosed by Doppler ultrasonography, the cause of delayed graft function, and in particular the differential diagnosis between postischemic acute tubular necrosis (the most common cause of delayed graft function) and acute rejection, can only be determined by biopsy.
Early posttransplant renal dysfunction is characterized by renal insufficiency 1–12 weeks after transplantation in patients with initial normal functioning of the graft. The major causes of early dysfunction include acute rejection, calcineurin inhibitor (cyclosporine or tacrolimus) nephrotoxicity, urinary tract obstruction, or reduced renal perfusion associated with a reduction in effective circulating volume. Other diagnostic possibilities include infections (cytomegalovirus or polyoma virus) and early recurrence of the primary renal disease such as segmental glomerulosclerosis, hemolytic-uremic syndrome and thrombotic thrombocytopenic purpura, Goodpasture’s syndrome (antiglomerular basement membrane antibody disease), and interstitial nephritis (Josephson et al. 1999). If one can exclude calcineurin inhibitor toxicity (by briefly reducing the dose and not seeing an improvement in renal function) and urinary tract obstruction, renal biopsy would be highly indicated.
Late acute graft dysfunction is characterized by abrupt worsening of renal function more than 3 months after transplantation. The causes of this situation are essentially the same as those of early posttransplant renal dysfunction, plus the possibility of noncompliance, especially in the case of adolescent recipients. A negative renal ultrasound, particularly the absence of renal artery stenosis, indicates the performance of the allograft biopsy.
Many patients suffer a gradual deterioration of renal function in the years following transplantation, often with persistent proteinuria and hypertension. In this situation, in cases where there is a suspicion of disease recurrence or de novo glomerulonephritis vs. chronic allograft nephropathy or drug nephrotoxicity, renal biopsy can provide valuable information (Briganti et al. 2002), particularly if one is contemplating the conversion of the immunosuppressive regimen.
3.2 Optional Indications
3.2.1 Persistent Nonnephrotic Proteinuria
Renal biopsy is not currently indicated, at least in common clinical practice, in patients who present with isolated proteinuria less than 500 mg to 1 g per 24 h, normal renal function, absence of hematuria of glomerular origin (see below), and absence of clinical or laboratory signs suggestive of systemic disease associated with glomerular pathology, such as systemic lupus erythematosus, vasculitis, monoclonal gammopathy, etc. In such cases the prognosis is good in terms of renal function, and there is no indication for therapy with steroids or other immunosuppressants. Current nephrological opinion changes, however, for proteinuria consistently and significantly greater than 1 g per day, particularly when there is an insufficient response to angiotensin-converting enzyme inhibitors or angiotensin receptor blockers; in these cases most nephrologists opt for biopsy. The presence of diabetes mellitus, in particular in the absence of other signs of microangiopathy such as retinopathy, does not always justify the clinical diagnosis of diabetic nephropathy. Studies carried out on patients with diabetes mellitus type 2 and proteinuria have shown that between 10 and 30 % of cases result from nephropathy different from classical diabetes (Fioretto et al. 2008), and thus, also in the presence of diabetes and proteinuria, renal biopsy should be considered to optimize the therapeutic approach.
3.2.2 Isolated Glomerular Hematuria
Patients who present with isolated glomerular hematuria (dysmorphic red cells and/or red cell casts in the urinary sediment, dipstick negative for proteinuria, normal renal function, normal blood pressure) usually have a benign prognosis in terms of renal function and do not require drug therapy or particular restrictions in terms of lifestyle. In these cases in which prognostic information is not forthcoming and the nephrologist is not confronted with the necessity of making therapeutic choices, renal biopsy does not appear to be indicated. One series of patients with these clinical characteristics in which renal biopsy was performed demonstrated thin membrane disease in 43 % of cases, IgA nephropathy in 20 %, other glomerular pathology (including Alport’s syndrome) in 19 %, and histologically normal kidneys in 18 % (Hall et al. 2004). In another series renal biopsy modified the therapeutic strategy in only 3 % of cases (Richards et al. 1994). An exception could be made for cases of isolated glomerular hematuria associated with a family history of renal disease and particularly of chronic kidney injury. When the patient in question is young, renal biopsy may have a role in genetic counseling. In cases in which the hematuria is associated with nonnephrotic proteinuria, the probability of significant glomerular pathology is greater than 70 %, and in particular the probability of finding IgA nephropathy is greater than 40 % (Hall et al. 2004); in this situation, performance of renal biopsy should be considered.
3.2.3 Chronic Kidney Injury
Renal biopsy may have an important diagnostic role also when the patient presents with established chronic renal injury. The leading example is when renal cortical thickness, demonstrated by ultrasound, is greater than 8–10 mm (Barbiano Di Belgiojoso et al. 2002), particularly associated with proteinuria but also in the absence of proteinuria. In patients with proteinuria, renal biopsy may identify the glomerular disease responsible for the proteinuria, modify the therapy accordingly, quantify the degree of chronicity of the lesion as a useful prognostic indicator, and demonstrate pathology which may be destined to recur in a possible future kidney transplant (Pasquali 2008; Lupo et al. 2008). In patients with chronic kidney injury without proteinuria, renal biopsy can also play an important diagnostic role with therapeutic implications, as well as in defining the chronicity index and the prognosis. An important example is when the biopsy demonstrates an interstitial nephritis which may be susceptible to corticosteroid treatment (Tomson Charles 2003).
4 Contraindications to Renal Biopsy
Contraindications to the performance of renal biopsy can be absolute or relative. In effect the only absolute contraindication, apart from the refusal of the patient to consent to the procedure after having been completely informed regarding the risks and benefits, is the inability of the patient to cooperate with the operator at the moment of the biopsy (as a consequence, e.g., of respiratory difficulty or of the impossibility to maintain the correct position during the entire period of the procedure). Relative contraindications include a hemorrhagic diathesis, severe uncontrolled hypertension, the presence of a single kidney (congenital or acquired), a renal neoplastic mass or renal cysts, a renal artery aneurysm, a renal or perirenal abscess, or the presence of hydronephrosis.
A detailed medical history, an accurate physical exam, and the timely discontinuation of anticoagulant or antiplatelet drugs, together with a prebiopsy laboratory evaluation of coagulation status, would demonstrate and allow the correction of any bleeding risk before the biopsy procedure. In particular it is necessary to demonstrate before the biopsy that the platelet count is greater than 100,000/mm3, that prothrombin time and activated partial thromboplastin times are in the normal range, and that the bleeding time is in the normal range. Significant anemia can also alter bleeding time, and in these cases any additional anemia induced by the biopsy could per se worsen the clinical conditions of the patient. A hematocrit value greater than 30 % and a hemoglobin concentration greater than 10 g/dL would represent an acceptable safety level. An elevated bleeding time (>8–10 min), together with a carefully obtained history and physical exam, and the hematocrit and hemoglobin values are the major predictors of hemorrhagic risk in patients who undergo renal biopsy (Mattix and Singh 1999). An abnormal bleeding time in the absence of other prohemorrhagic factors does not necessarily prohibit the performance of the biopsy; the procedure can be carried out after premedication with DDAVP (deamino-1-8-d-arginine vasopressin), which is administered at a mean dose of 0.3 μg/kg 1 or 2 h before the biopsy (Mannucci et al. 1983). For patients in therapy with an anticoagulant, the drug should be discontinued for a period sufficient to reduce the International Normalized Ratio (INR) to equal or less than 1.5. If the patient is on heparin, the drug should be stopped at least 12–24 h before the procedure, and low molecular weight heparin should be discontinued at least 24 h before the procedure. Aspirin (and perhaps also ticlopidine) should be discontinued 2–3 weeks before the biopsy and nonsteroidal anti-inflammatory drugs at least 2–5 days before the biopsy. Paracetamol can be administered without worry. One should recall that some herbal medicines containing garlic, ginseng, and ginko, sold in pharmacies and health food stores as “revitalizers,” also have antiaggregant properties.
Uncontrolled hypertension increases bleeding complications following renal biopsy, and since severe and uncontrolled hypertension constitutes a serious disease per se, it also requires a treatment independently of the risk it represents for renal biopsy. Thus, at the moment of the biopsy the blood pressure should have been corrected to the level as close as possible to the norm.
The presence of a single kidney, whether congenital or acquired, is not a contraindication for renal biopsy in the absence of other risk factors; it is the normal situation for renal transplant patients, who are often the subjects for renal biopsy.
Renal tumors are normally an indication for surgical intervention; renal biopsy may provide useful information regarding the copresence of parenchymal renal disease by sampling the tissue which are free of tumor in the nephrectomy specimen (partial or total).
Renal cysts do not constitute a contraindication to renal biopsy, provided that a portion of the parenchyma can be found which would allow the percutaneous procedure. Indications for renal biopsy in a patient with polycystic kidney disease would be extremely rare.
The presence of a renal abscess or hydronephrosis requires urgent treatment, regardless of the copresence of renal parenchymal disease which may be an indication for renal biopsy. Thus, relief of urinary tract obstruction and antibiotic therapy for urinary tract infection, even if asymptomatic, would be considered prerequisites for renal biopsy.
Morbid obesity can cause difficulty in localizing the renal pole to biopsy and above all may not allow the renal parenchyma to be reached with the patient in the normal prone position, even with very long biopsy needles. In this situation, the biopsy may be carried out with success with the patient in the supine anterolateral position or under CT guidance (Gesualdo et al. 2008).
5 The Preparation of the Patient for Renal Biopsy
5.1 The Patient Before the Biopsy
Once there is a clinical indication to perform renal biopsy, absolute contraindications have been excluded, relative contraindications have been remedied, and risks associated with the procedure have been minimized, the biopsy is performed. The patient must be able to cooperate fully, simulating beforehand key moments in the biopsy procedure, such as controlling inspiration and brief moments of apnea. The patient must maintain an immobile posture in the prone position with the upper abdomen resting on a pillow or rigid bedroll, in order to fix the kidney in position.
The day of the procedure the patient must be fasting. In the case of agitation or anxiety, mild sedation is useful, but the patient must remain able to cooperate during the procedure. Venous access with an angiocath must be present, connected by an infusion set to a bottle of normal saline, in case of emergency.
6 The Biopsy Procedure
The biopsy procedure is preceded by selecting the site of the biopsy, which besides anatomic considerations depends on the eventual presence of lesions (e.g., cortical scars or cysts) that were seen in the preliminary renal ultrasound (US) examination and on the choice of biopsy needle. Immediately following the biopsy itself, the tissue is studied under the dissecting microscope to confirm that it is indeed renal parenchyma and is divided according to the various microscopic techniques it must undergo. Thus, a familiarity with the different preservation and fixation methods is required.
6.1 The Choice of the Biopsy Site
The preferred site of renal biopsy is the inferior pole of the left kidney because the renal pelvis and large-caliber vessels are relatively far from this level. The biopsy procedure is usually carried out under local anesthesia, although in children less than 10 years of age, general anesthesia may be preferred. Renal US is the preferred method for localizing the kidney and for monitoring more or less continually the procedure. Renal biopsy and US localization can be performed using more than one protocol, according to how the US is used in the various phases of the biopsy: (a) biopsy after US localization of the kidney (with the actual biopsy performed without visualization); (b) US-assisted biopsy in real time, without a guide on the US probe; and (c) US-guided biopsy in real time, with a guide fixed on the probe through which the needle is inserted. The US-guided biopsy in real time is currently considered the safest and most successful option.
6.2 Biopsy Needle Types
Technological progress has produced biopsy needles which are progressively more efficient and less traumatic. The needles used today can be differentiated on the basis by which the tissue core is obtained. In brief, (a) tweezer-like needles, (b) aspiration needles, and (c) cutting needles are available. Another distinguishing characteristic among needles involves the triggering mechanism of the needle that can be: (a) manual, (b) semiautomatic, or (c) automatic. From the aspiration technique of Iversen and Brun (1951), renal biopsy needle has evolved to the Vim and Silverman needle modified by Franklin, then to the spring mechanism of the Tru-Cut needle, and finally to the automatic needles in use today. These needles also have different sizes, and the choice of the caliber (14-16-18-20 gauge) depends on the necessity to obtain a histologically sufficient sample, the customs of the biopsy team, and the characteristics of the patient (size, age, native renal biopsy vs. transplant biopsy). Currently the needles most in use in adults have a caliber between 14 and 18 gauge (Fig. 1), whereas the biopsy needles for use in children have a caliber between 18 and 20 gauge, or even smaller in renal transplants for cellular aspirates for microhistology. Pathologists tend to prefer the tissue cores from the 14-gauge needle which, because of their greater dimensions, provide sufficient material for all the study preparations (Ferrario and Rastaldi 2003).


Fig. 1
(a) A tru-cut automatic needle with a caliper of 16 gauge, usually employed in diffuse renal diseases; (b) a tru-cut automatic needle with a caliper of 18 gauge, usually employed in focal renal disease; (c, d) the mechanism of action of the automatic tru-cut cutting needle. (c) The hollow core needle progresses in tissues while the outer cutting edge component (d) separates the tissue sample
Thus, the biopsy needles differ according to the characteristics of several variables: the cutting action and whether this action is partially or totally automatic; the needle calibre; the echogenicity to the needle tip; the length of the tissue core; the weight of the handle, etc.
The semiautomatic and automatic models offer some advantages: (a) they can be used single-handedly, and thus, a lone operator can both obtain the biopsy and operate the ultrasound probe, and (b) the velocity with which the sampling occurs, which is considered the most delicate parameter in terms of hemorrhagic complications, is decidedly superior compared to manual methods (shortening the time that the needle stays in the kidney and thus reducing the possibility of complications associated with movements of the organ or of the needle).
In conclusion, given the wide range of needle types currently available, it is evident that each operator who has an experience with renal biopsy will use the method and equipment on the basis of his or her personal experience and preferences.
6.3 Evaluation and Division of the Biopsy Tissue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree