SONOGRAM ABBREVIATIONS
Ao Aorta
D Diaphragm
K Kidney
L Liver
S Spine
Sp Spleen
KEY WORDS
Atelectasis (Collapsed Lung). Collapse of part of the lung due to volume loss; atelectasis is caused by either extrinsic compression (pneumothorax or pleural effusion) or intrinsic obstruction of a central bronchus.
Consolidation. An infected segment of the lung filled mainly with fluid instead of air.
Empyema. Pus in the pleural cavity.
Hemothorax. Blood in the pleural cavity.
Paradoxical Motion. Opposite from normal motion of the diaphragm. Specifically, downward motion of the diaphragm with expiration and upward motion on inspiration due to hemidiaphragm paralysis.
Pleura. A thin membrane that lines the thorax and diaphragm and surrounds the lungs. It has two layers:
Parietal (Costal) Pleura. Extends from the inferior aspect of the lungs and covers the sides of the pericardium to the chest wall and backward to the spine. The outer layer of the pleura.
Visceral Pleura. Lines the lungs and the interlobar fissures; it is loose at the borders to allow for lung expansion. The inner layer of the pleura.
Pleural Cavity. The space between the two layers of the pleura, where pleural fluid accumulates.
Pleural Fibrosis. Fibrous tissue thickening the pleura; results from chronic inflammatory diseases of the lungs such as tuberculosis.
Pneumothorax. Air within the pleural cavity outside the lung—a possible complication of thoracentesis. Hydropneumothorax implies both fluid and air within the pleural space.
Subpulmonic. Inferior to the lungs, above the diaphragm.
Thoracentesis. Puncture of the chest to obtain pleural fluid.
The Clinical Problem
Because of the air in the lungs, chest sonography is limited to assessing pathology adjacent to the pleura. Fluid accumulates in the pleural space as a reaction to underlying pulmonary or upper abdominal disease, or as a consequence of systemic disease such as heart failure. Effusions are usually detected by chest radiography. Fluid that is free follows gravity and falls to the base of the chest; however, loculated fluid, which is the result of adhesions or malignancy, does not layer on chest radiograph. The distinction is easily made using ultrasound, providing the pocket lies adjacent to the ribs.
Obtaining a fluid sample can be important for diagnostic purposes or may be a palliative measure to alleviate shortness of breath. Clinicians customarily localize for thoracentesis in the patient’s room by percussing the chest (“thumping” with their fingers) and listening for dullness. In obese or muscular patients, clinical localization may fail. In cases like these, ultrasound is helpful in guiding thoracentesis. Ultrasound is also helpful in determining the nature of an opaque hemithorax on the chest radiograph. Such an opacification may indicate tumor, fluid, collapsed lung, or a combination of these entities.
Diaphragmatic movement can be detected by ultrasound. This demonstration is especially helpful in ruling out paradoxical motion due to diaphragmatic paralysis.
Ultrasound is being used more and more, particularly in trauma settings, as a rapid, easily obtained tool to diagnose pneumothorax.
Anatomy
NORMAL CHEST
When no fluid or mass is present, the tissues within the chest do not conduct sound. There are alternating bands of echogenicity due to reverberations from air and the rounded, bright reflectors seen due to the bone. Between the skin and ribs are subcutaneous fat and muscles; the soft tissue between ribs is mostly muscle. Because the intercostal vessels lie under the lower lip of each rib, they are poorly seen; however, remember their location when deciding on needle placement. All thoracentesis needle placements should be just on top of the rib to avoid these vessels.
The pleural space is that potential space between the parietal and the visceral pleura, which normally contains only a few millimeters of a lubricating secretion. The surface of the lung can be seen moving up and down with respiration, and the ventilated lung produces a reverberation artifact in the intercostal spaces (Figs. 21-1 and 21-2).
DIAPHRAGM
The diaphragm is seen as an echogenic, curved line above the liver and spleen. The diaphragm can be difficult to demonstrate, especially on the left, because it lies along virtually the same axis as the ultrasonic beam. The spleen provides less of a window to angle through than does the liver.
Technique
For masses or loculated effusions, position the patient so the pathology site is easily accessible and so he or she is comfortable enough not to move during the procedure.
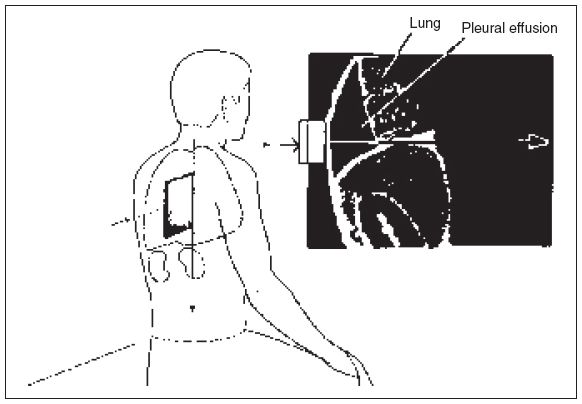
Figure 21-1. ![]() Usual position used when scanning a pleural effusion. The ultrasonic appearance of a pleural effusion and lung (inset). Note the alternating pattern of reverberations from the air and absent transmission from bone in the lung area.
Usual position used when scanning a pleural effusion. The ultrasonic appearance of a pleural effusion and lung (inset). Note the alternating pattern of reverberations from the air and absent transmission from bone in the lung area.
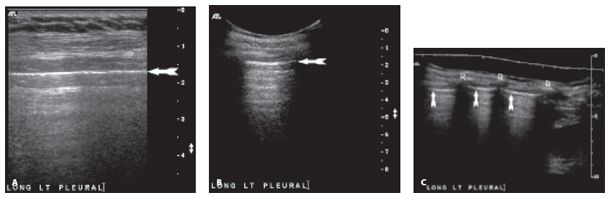
Figure 21-2. ![]() Longitudinal sonogram of the chest wall in a healthy patient without pneumothorax. Note ribs (R) with posterior acoustic shadowing, and reverberation artifact found in normal lung. A. Linear transducer for best resolution. B. Curved linear transducer. C. Extended field-of-view technology with linear transducer showing several interspaces. Pleural margin (arrow).
Longitudinal sonogram of the chest wall in a healthy patient without pneumothorax. Note ribs (R) with posterior acoustic shadowing, and reverberation artifact found in normal lung. A. Linear transducer for best resolution. B. Curved linear transducer. C. Extended field-of-view technology with linear transducer showing several interspaces. Pleural margin (arrow).
Figure 21-3. ![]() Diaphragmatic representation of a pleural effusion above the diaphragm (D) on a supine longitudinal view (A) and supine transverse view (B). Note that the fluid extends to the spine on transverse views. Longitudinal sonogram (C) showing left-sided pleural effusion (E) in a premature neonate who was born with a complex cardiac defect. L, collapsed lung surrounded by the pleural fluid. Transverse sonogram (D) through the base of the right lung showing an anechoic (simple) right pleural effusion (“RT PL”) above the hemidiaphragm and a tiny amount of ascites (arrow) under the hemidiaphragm.
Diaphragmatic representation of a pleural effusion above the diaphragm (D) on a supine longitudinal view (A) and supine transverse view (B). Note that the fluid extends to the spine on transverse views. Longitudinal sonogram (C) showing left-sided pleural effusion (E) in a premature neonate who was born with a complex cardiac defect. L, collapsed lung surrounded by the pleural fluid. Transverse sonogram (D) through the base of the right lung showing an anechoic (simple) right pleural effusion (“RT PL”) above the hemidiaphragm and a tiny amount of ascites (arrow) under the hemidiaphragm.
PLEURAL EFFUSION
Pleural effusions (Figs. 21-1 and 21-3) usually pool above the diaphragm along the posterior chest wall. It is sometimes necessary to scan along the axillary line to check for fluid laterally. Loculated effusions can be found in any location (Fig. 21-4). Plan the search by examining the chest radiograph or computed tomography (CT).
The patient is scanned upright, sitting on a stool without a back, or a stretcher with his or her legs dangling from the sides, thus affording ready access from all sides (Fig. 21-1). For ill patients, it is helpful to have a sturdy table or stand in front of the patient to rest his or her chest on during the procedure. If looking in the posterior chest, one can better visualize the area behind the scapulae by having the patient cross his or her arms, rotating the scapulae outward. Scanning in the supraclavicular fossa will allow access to the superior sulcus to look for loculated effusions or apical tumors. Subpulmonic masses or empyema may be best seen by scanning from the abdomen.
A 3.5- to 5-MHz transducer is usually an appropriate frequency to display the chest wall and the distance to the lung. A curved, linear transducer with a wide footprint is best for the initial search, whereas changing to a smaller sector is helpful in evaluating deeper structures, where the near field is less important. For small collections, scanning with a linear transducer may be helpful in obtaining optimal visualization and localization.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



