Case presentation
A 10-day-old infant presents to the emergency department with 1 day of fussiness, decreased oral intake, decreased urine output, and three grossly bloody stools. There has been no fever, cough, congestion, vomiting, or rash. The child is breastfed exclusively and the mother denies she has had cracked nipples or bleeding from the breast. She has noted the child is feeding less vigorously today.
The child was born vaginally at 34 weeks and spent 4 days in the hospital to observe feeding and required blow by oxygenation for 24 hours. The mother had excellent prenatal care. Prior to hospital discharge, the patient had normal feeding and stooling.
The child is afebrile with a heart rate of 170 beats per minute, a respiratory rate of 30 breaths per minute, and a pulse oxygenation saturation of 98% on room air. While not in obvious distress, the child is fussy during the examination but otherwise remains quiet, which the parents state is not typical. The physical examination is unremarkable, except for mild abdominal distention without obvious tenderness; rectal examination shows a patent anus and is guaiac positive. Right after the rectal examination, she passes a loose, grossly bloody stool.
Imaging considerations
Pneumatosis discovered on radiography is a sign, rather than a specific diagnosis, which can be associated with either benign or potentially life-threatening conditions.
Plain radiography
Plain radiography is the first-line imaging modality employed in many instances when bowel pathology is a concern. Pneumatosis, portal venous gas and free intraperitoneal air can be detected on abdominal radiographs. Initial imaging should include a supine and cross-table, horizontal view. Although a left lateral decubitus view is preferred, the cross-table view is often obtained in the supine position in ill-appearing infants to minimize movement. Attention should be paid to intraluminal, intramural, portal venous, and free intraperitoneal gas visualized with abdominal radiography. In infants with a clinical history and examination compatible with necrotizing enterocolitis (NEC), the finding of pneumatosis intestinalis with or without portal venous gas should prompt concern for this entity. Pneumoperitoneum can be demonstrated by plain radiography, appearing as an unusual and at times oblong central lucency on the anteroposterior view and can often be more easily seen on a left lateral decubitus view. While abdominal radiography may not be sensitive enough to detect pneumatosis early in its course, , it does remain the initial imaging modality of choice. ,
Computed tomography (CT)
CT is not a first-line imaging study but has been shown to be more sensitive at detecting pneumatosis intestinalis and portal venous gas compared to plain radiography. , , CT may also demonstrate bowel wall thickening, free fluid, and peri-intestinal soft-tissue stranding, which are associated with a serious underlying process. This imaging test may be useful if the diagnosis is uncertain or there is suspicion for complex disease or deteriorating clinical status. ,
Both plain abdominal radiography and CT are useful to help distinguish so-called pseudo-pneumatosis intestinalis (which is gas trapped in feces or against the mucosal surface) from true pneumatosis based on the location, pattern, and distribution of the observed gas. Features suggestive of true pneumatosis include portal or mesenteric venous gas, intramural gas superior to a gas-fluid level, continuous gas outlining the bowel wall, and dissecting gas in the bowel wall edge.
Ultrasound (US)
US has become an imaging modality of interest for use in patients with pneumatosis and suspected NEC. Among infants with NEC, US is a useful adjunct to plain radiography of the abdomen. , , In addition to identifying free air, pneumatosis, and portal venous gas, US can detect ascites and bowel wall thickening, and Doppler examination can detect bowel wall ischemia, helping assess for bowel viability. , , Highly concerning sonographic findings in infants with NEC include free air, absent bowel peristalsis, absent bowel wall perfusion, and complex ascites. US of the bowel in infants is personnel dependent, requiring experienced sonographers and experienced pediatric imagers to obtain and interpret these studies.
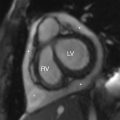
Imaging findings
An abdominal radiograph was obtained and demonstrates a nonobstructive bowel gas pattern, with a mottled appearance of gas over the lateral left lower quadrant suggestive of pneumatosis, and a small lucency over the right upper abdomen concerning for possible free air ( Fig. 10.1 ). A lateral decubitus film was then obtained, demonstrating an irregular lucency over the nondependent abdomen adjacent to the distended bowel suggesting free air ( Fig. 10.2 ).


Case conclusion
The child was placed on intravenous antibiotics and bowel rest and admitted to the hospital for treatment and observation. Serial examinations and close radiographic follow-up were ensured. The patient’s examination improved and follow-up imaging demonstrated resolution of the previously identified findings. She did not require surgical intervention.
Pneumatosis intestinalis is gas in the bowel wall. , , This may be an incidental finding on plain abdominal radiography but may also be associated with more serious processes, such as infection or trauma. The exact mechanism that produces pneumatosis is not clear, but there are multiple theories addressing this formation process. Clinical presentation may include abdominal pain, fever, vomiting, diarrhea, abdominal distention, and signs of sepsis, but pneumatosis may be asymptomatic. , ,
Pneumatosis intestinalis can be associated with ischemic and nonischemic processes, and both have been well described in the literature. Nonischemic processes include bacterial overgrowth (for example, in immunocompromised or immunosuppressed patients undergoing treatment with steroids or chemotherapy) and inflammatory bowel disease. In the former case, there is bacterial penetration of the bowel mucosa and production of intramural gas; in the latter, there is mucosal ulceration, allowing gas to penetrate the bowel wall. , , , , Ischemic processes can be present during infection, such as with NEC or enteritis, in which intramural gas is produced by necrosis of the bowel wall due to bacterial fermentation activity. , , , Pneumatosis has been associated with trauma, , intussusception, and volvulus, , and rarely after laparoscopic surgery including appendectomy. A broad differential should be considered when pneumatosis intestinalis is encountered.
Pediatric pneumatosis intestinalis outside of the neonatal period has been reported in the literature and has been described as benign in many cases. , , , , Several theories have been postulated as to the underlying pathology leading to pneumatosis in the older age group. Pneumatosis has been described in patients with underlying medical conditions, including pulmonary disease, immunocompromise, congenital heart disease, and short gut syndrome, with some cases being recurrent. Another study examining patients outside of the neonatal period (age greater than 30 days) found pneumatosis not only in patients with chronic illness but also in healthy children. In this series, pneumatosis was caused by noninfectious colitis (32%), acute enteric infection or toxin (27%), bowel ischemia (20%), and gastrointestinal dysmotility (17%). The majority (78%) of cases resolved with medical management; however, portal venous gas and low serum bicarbonate were associated with poor outcomes. A case report of a child with corticosteroid dependence due to chronic medical illness was reported to have pneumatosis intestinalis without portal venous gas; he was managed medically, with a good outcome.
Pneumatosis intestinalis from blunt abdominal trauma, while rare, can occur. , Mucosal tearing produced from sudden bowel compression allows gas to enter the intramural space; this causes a disruption in the blood supply of the bowel, producing dissection of gas into the bowel wall. The presence of portal venous gas may also be associated with abdominal trauma; due to an acute change in pressure, gas penetrates submucosal veins and travels to the portal venous system. , , It is important to note that while the presence of gas in the bowel wall implies mucosal injury, it does not necessarily mean necrosis in this setting. , If pneumatosis intestinalis, with or without portal venous gas, is present on radiography, the clinician should consider traumatic causes, particularly if there is no history, physical examination findings, or laboratory values to suggest another source, such as an infectious process. Bowel necrosis as a result of blunt abdominal trauma and subsequent clinical deterioration in a premature infant with pneumatosis intestinalis and extensive portal venous gas, eventually leading to death, has been reported in the literature. Blunt abdominal injury is a leading cause of death due to nonaccidental trauma in the pediatric population and can present as an isolated finding; the lack of apparent signs of physical abuse (bruising, swelling, pain) or intra-abdominal injuries (solid organ lacerations or intestinal hematomas) should not dissuade the clinician from considering nonaccidental trauma as a potential etiology when pneumatosis is discovered on radiography.
In the neonatal period, pneumatosis intestinalis with or without portal venous gas is seen as a sign of NEC, an extremely grave condition with a mortality rate of up to 30%. , , NEC is commonly seen in premature infants, with the risk decreasing with increasing age and weight, , , but can be seen in full-term infants. NEC is thought to be due to intestinal immaturity, leading to a predisposition for endothelial disruption and special properties of the newborn intestinal response to stressful physiologic situations. , Low birth weight is the most commonly reported risk factor for NEC, but small for gestational age, assisted ventilation, sepsis, hypotension, and prolonged rupture of membranes have also been reported risk factors. , Infants affected with NEC have been shown to have an increased incidence of adverse neurodevelopmental outcomes, intestinal strictures, short gut syndrome, and growth delay. , Clinical signs of NEC include temperature instability, poor feeding, lethargy, apnea, hypotension, abdominal distention, bloody stools, and signs of sepsis. Bacterial species found in association with NEC include Escherichia coli , Klebsiella pneumoniae , Proteus mirabilis , Enterobacter cloacae , Clostridium perfringens , and Pseudomonas aeruginosa .
Management of pneumatosis depends on history, physical examination, and the suspected underlying etiology. The management of NEC in the neonatal period consists of broad-spectrum antibiotics, bowel rest, intravenous fluids, and ionotropic support. , , Surgical intervention is usually indicated if there is suspicion of necrosis, regardless of etiology. , , This is often the case with NEC that is failing medical management, as up to 50% of infants with NEC require surgery and the need for surgery is linked to a higher mortality rate. , Pneumatosis thought not to require surgical intervention can be managed medically with close observation, including bowel rest, bowel decompression, and antimicrobial therapy as clinically indicated. , , , , Since it can be difficult to distinguish the two radiographically, history and clinical examination are paramount when interpreting radiographic findings and planning a course of management.