11 Scars—The Treated Breast Scars can challenge the goal of accurate imaging interpretation. Scars and malignancies share many of the breast findings on which diagnosis hinges: architectural distortion, focal asymmetries, calcifications, and at times, masses (Table 11.1) Additional signs of advanced cancer—skin thickening and breast edema—are also hallmarks of the irradiated breast. Application of clinical history, review of imaging findings correlated with the chronology of surgical alteration and trauma, and knowledge of the specifics of the procedure will help to minimize the false-positive diagnosis of benign lesions and reduce the number of unnecessary biopsies, while at the same time avoiding a false-negative diagnosis of breast cancer. Without having reviewed a sequence of previous examinations including preoperative studies, if available, the use of mammography alone can pose problems in differentiating spiculated scars from tumor. In using ultrasound, to distinguish scar from tumor—new or locally recurrent—considerable experience is often needed (Fig. 11.1 a, b). The greatest difficulties are encountered in women who have undergone breast-conserving cancer surgery. An adequate local excision of a carcinoma usually leaves a relatively large surgical cavity with a correspondingly extensive scar. The tumor bed fills with fluid, ordinarily not drained as the slow resorption is thought to promote cosmesis. The picture is further complicated by breast edema and skin thickening caused by postoperative irradiation of the breast and a boost dose to the tumor bed. Contrasted with the near-complete resolution of findings related to benign surgical excisions, for many women in a year or 18 months, radiation therapy prolongs the resolution time of post-treatment changes to 2 years or more, and for some findings, there is never a return to the pretreatment appearance (Fig. 11.2). Initially the radiation mastitis obscures the scar, which then becomes increasingly conspicuous as the edema recedes in the same 3-year time frame that a local recurrence might be found at or near the lumpectomy site (Fig. 11.3 a–e). Unfortunately, this can start a chain reaction of unnecessary diagnostic procedures, including core needle or surgical biopsy, that causes a great deal of anguish that is frequently avoidable.
Clinical Significance, Diagnostic Problems
– Pain – Sensory disturbance – Cosmetic disfigurement – Breast lumps
– Inspection: skin retraction – Palpation: indeterminate mass – Mammography: spiculated density – Ultrasound: indeterminate hypoechoic lesion
|
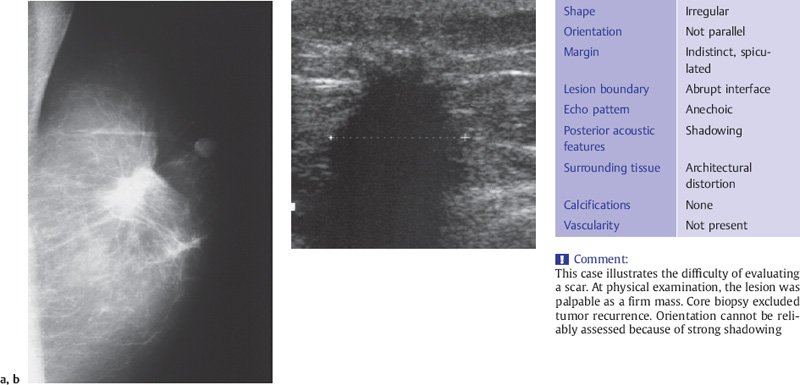
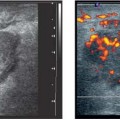
Fig. 11.1 a, b Typical findings 2 years after breast-conserving surgery.
a The mediolateral mammogram shows a spiculated density in the original tumor bed.
b The ultrasound appearance of the lesion is also suspicious.
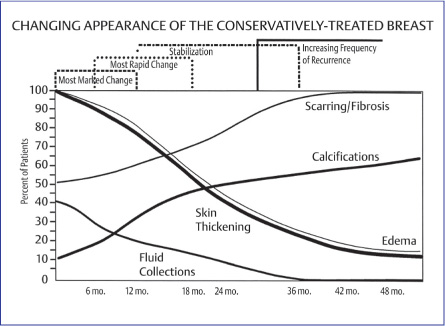
Fig. 11.2 Changing appearance of the conservatively treated breast. With permission from Elsevier, 1992.
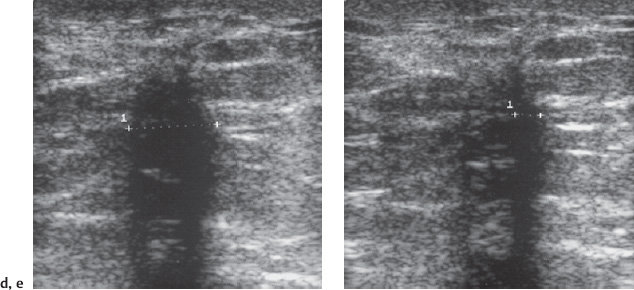
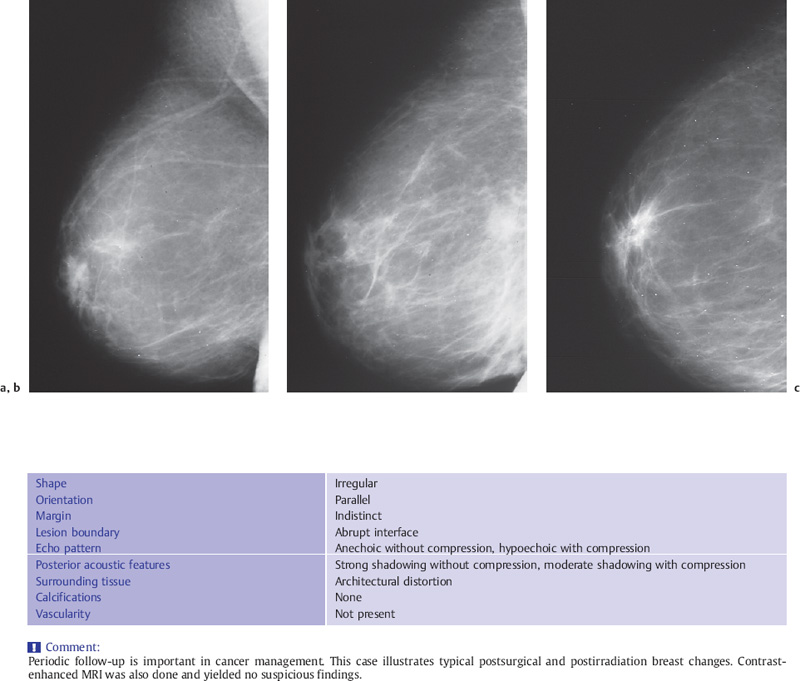
Fig. 11.3 a–e Follow-up of a scar after breast-conserving surgery and radiotherapy.
a Preoperative mammogram shows a typical carcinoma.
b 1 year after breast-conserving surgery and postoperative radiotherapy, increased density is seen throughout the whole breast.
c 2 years after surgery and irradiation, the breast appears less dense but the scar is more conspicuous and resembles a local recurrence.
d Ultrasound without compression at 2 years appears suspicious.
e Scanning with breast compression shows increased structural details, resulting in a lower index of suspicion.
Mammographic follow-up is essential, particularly in identifying and analyzing calcifications. Special views and careful sequential review of these mammograms, sonograms, and, when they are done, MRI scans can help to overcome some of the limitations imposed by conservative cancer treatment. Ultrasound can be a very valuable adjunct in differentiating postsurgical and postirradiation changes from malignancy. In difficult cases, when the lumpectomy scar is mature after approximately 2 years, contrast-enhanced MRI may be able to resolve the ambiguity between benign post-treatment changes and recurrence.
Diagnostic Criteria, Postoperative Follow-Up
A mammographic view tangential to the scar, best with spot compression and magnification, with a thin wire taped to the skin along the length of the scar, can separate the thickened skin at the entry site from the tumor bed itself, eliminating the extra density projected on to the lumpectomy site by the skin scar that at times suggests possibility of recurrence. But by the nature of the imaging modality, intramammary post-treatment changes can be visualized clearly and directly with ultrasound. One advantage of ultrasound is that it is tomographic, each image representing a thin slice of tissue, thus eliminating superimposed structures. Ultrasound also presents an opportunity to evaluate the compressibility of lesions during real-time scanning. Experience is needed, however, to correctly interpret the variety of changes that may be found.
Typical Findings
Intramammary scars often appear hypoechoic on ultrasound due to the refractive effects caused by the diffuse, regenerative proliferation of connective tissue (Table 11.2). The lesion has indistinct margins and often casts an acoustic shadow. The connective tissue fibers in scars are compressible, however. Pressure from the transducer flattens the fibers, frequently causing the hypoechoic lesion and posterior acoustic shadow to disappear (Figs. 11.4 a, b, 11.5), as may also happen in areas of native fibrotic tissue with no antecedent trauma or surgery. This alteration in sonographic appearance is helpful in the differential diagnosis, especially in attempting to distinguish a scar from recurrent tumor following breast-conserving surgery.
Shape | Irregular |
Orientation | Not parallel |
Margin | Indistinct |
Lesion boundary | Abrupt interface |
Echo pattern | Anechoic without compression* |
 Subjective complaints
Subjective complaints Interference with follow-up
Interference with follow-up Consequences: morbidity and costs due to repeat surgery, or costly additional diagnostic procedures
Consequences: morbidity and costs due to repeat surgery, or costly additional diagnostic procedures