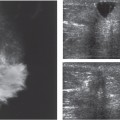
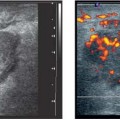
16 Screening Screening involves examining asymptomatic individuals to detect an epidemiologically significant disease. A successful screening program requires a disease of high prevalence where early detection can affect the course of the disease, standardized technique of examination and interpretation, patient compliance, effective treatment, accessibility to the population at risk, and a low-risk cost-effective approach, not to mention the need for suitable equipment and trained personnel. In the United States and western Europe, breast cancer is without question an epidemiologically significant disease. In the United States in the last several years, the number of newly diagnosed female breast cancer patients has ranged from 180 000 to over 200 000 annually. In randomized controlled trials of X-ray mammographic screening over several decades the mortality reduction attributable to mammographic screening is over 20%, and has been reported in László Tabár’s long-term Swedish studies to be as high as 60%. Tabar includes 40–50-year-old women. Postmenopausal women and women over the age of 50 years screened with mammography have also shown mortality reduction, the measure of success in breast cancer screening as opposed to survival, which can be affected by biases such as when detection occurred in the temporal course of the disease. In spite of published data, discussions about the value of screening in premenopausal women continue. Although the incidence of breast cancer rises with increasing age, breast malignancies occur in significant numbers of women under the age of 50 and measurably in women younger than 40 years. Younger women tend to have denser breasts, where mammography is less sensitive than in the fatty breasts of older women. This is only a generalization, however, and many postmenopausal women have dense breast tissue related to fibrous tissue, and some premenopausal women, particularly multiparous women, have fatty breasts that are easy to evaluate mammographically. Although the incidence of breast cancer is lower in women aged 40–50 than in those over 50 years of age, mammography-related mortality reduction in women under 50 supports screening, and the American Cancer Society recommendations in the United States call for annual screening mammography in asymptomatic women from the age of 40 years (Fig. 16.1 a–c). There is no agreed-upon age at which screening should be stopped. The benefits of mammographic screening and the recommendations for its use are based on statistical evaluation of the prevalence of breast cancer in a population at average risk. For women whose risk of developing breast cancer is extremely high—women with a young, first-degree relative (mother, sister, daughter) with premenopausal breast cancer, particularly if bilateral—the advice is for mammography is to commence 5–10 years earlier than the ageat which the affected relative was diagnosed. In discussing screening issues, we must consider that many premenopausal women have clinical symptoms or see their doctor because of cancer fears. In particular, women who are at risk for breast cancer because of a positive family history or previous surgery for atypical proliferative fibrocystic change cannot be placed in the same category as other screening patients. They should be offered a screening program in which negative results will afford these women a reasonable degree of assurance that they do not have breast cancer detectable at the time of the examination. Everyday clinical experience and the results of screening studies teach us that mammography alone cannot accomplish this goal in young women with radiographically dense breasts (Fig. 16.2 a, b). This had led to uncertainty among many women and physicians about the need for screening mammography at all, and adoption for screening of other imaging modalities unproven through randomized controlled trials to reduce breast cancer mortality. Unfortunately, recognition of the limitations of mammography may have tended to reduce patient compliance for this medically necessary screening examination. What is under study, however, are the benefits of supplemental screening with other imaging modalities for women at high risk of breast cancer with mammographically dense breasts. Currently, the two imaging modalities most likely to be used in addition to mammography are ultrasound and MRI. As shown in the preceding chapters, modern high-resolution handheld ultrasound techniques can detect early breast cancer (Fig. 16.3
Clinical Significance
Target Group for Extended Screening
Prerequisites for Extended Screening
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree