Scrotal Emergencies
Paul R. Sierzenski
Stephen J. Leech
INTRODUCTION
The patient presenting to the emergency department (ED) with acute scrotal pain represents a high-risk, time-urgent complaint. The differential diagnosis includes testicular torsion (with potential organ loss and loss of fertility) epididymitis, orchitis, trauma, hemorrhage, and tumor. The signs, symptoms, and physical findings of these conditions are nonspecific and do not discriminate between disease states. One series demonstrated that in up to 50% of cases of acute scrotal pain, the diagnosis could not be made on the basis of history, physical exam, and lab work alone (1). Diagnostic imaging is often necessary. Testicular ultrasound with power and spectral Doppler has become the imaging modality of choice in patients with acute scrotal pain or swelling (2, 3, 4, 5, 6, 7, 8, 9). Emergency physicians can utilize the increased availability of bedside ultrasound in the ED to expedite patient care and prompt referral to specialists. Studies have shown that emergency physicians with expertise in ultrasound can accurately identify and discriminate causes of the acute scrotum compared to radiology-based studies and surgical findings (10, 11, 12).
CLINICAL APPLICATIONS
Testicular ultrasound is useful for the evaluation of:
Acute scrotal pain
Scrotal mass
Scrotal trauma
Ultrasound can facilitate the recognition and diagnosis of:
Testicular torsion
Epididymitis and orchitis
Testicular fracture
Scrotal masses (including hydroceles, solid tumors, and hernias)
Testicular Torsion
Testicular torsion represents a true surgical emergency, and any patient with acute scrotal pain or swelling should be suspected to have torsion until proven otherwise. Patients with a bell-clapper deformity lack the normal posterior fixation of the testicle to the scrotal wall, and thus twisting and torsion are more likely. Testicular torsion results from the twisting of redundant spermatic cord on its pedunculated blood supply, causing testicular ischemia. Venous thrombosis then occurs, followed by arterial thrombosis. The degree of twisting of the testicle about its axis affects how rapidly testicular infarction can occur. In an animal model, 90 degrees of torsion caused no testicular necrosis at 7 days, 360 degrees of torsion resulted in necrosis in 12 to 24 hours, and 1440 degrees of torsion caused necrosis in 2 hours (13). It is generally thought that rotation of at least 450 degrees is needed to cause complete testicular torsion (14). In addition, spontaneous torsion-detorsion and incomplete torsion can occur. Torsion occurs at two age peaks, the first during infancy, and the second during
puberty. However, the emergency physician must still consider the diagnosis of torsion after puberty, as up to 20% of cases occur postpubescently (15).
puberty. However, the emergency physician must still consider the diagnosis of torsion after puberty, as up to 20% of cases occur postpubescently (15).
Prompt diagnosis and treatment lead to higher salvage rates. Reported salvage rates range from 80% to 100% for patients treated within 6 hours of symptom onset, 70% to 83% between 6 and 12 hours, and 20% to 80% after 12 hours (16, 17, 18, 19). No successful testicular salvage has been reported after 48 hours of torsion (19).
Epididymitis and Orchitis
Epididymitis is the most common cause of acute scrotal pain in adults and also represents the most common misdiagnosis in cases of missed testicular torsion (20). This misdiagnosis usually occurs in men under age 35, in whom testicular torsion and epididymitis are both common. Epididymitis occurs in patients of all ages, from infants to the elderly. It can result from either viral or bacterial infection with inflammation.
In most cases, epididymitis is caused by extension of infection from the lower urinary tract. In men under 35 years, epididymitis is most often a sexually transmitted disease, with Chlamydia trachomatis or Neisseria gonorrhoeae as common etiologic agents. In older males, epididymitis is usually caused by gram-negative pathogens as a result of a urinary tract infection or recent urinary instrumentation (20). Occasionally, epididymitis results from trauma, and some cases are idiopathic with no definite cause. Severe cases of epididymitis can result in abscess formation.
Orchitis is an acute infection of the testis and usually follows an initial episode of epididymitis. The infectious agents implicated in orchitis are similar to those that cause epididymitis. In some cases, an isolated orchitis occurs in the setting of viral infection. Several etiologic agents have been implicated, with mumps being the most common cause.
Scrotal Trauma
Direct trauma to the scrotum can result in contusion, hematoma formation, testicular fracture, torsion, and testicular dislocation. Ultrasound is helpful in defining the location and extent of injury and helps to guide management. When the tunica albuginea is ruptured, surgical intervention is required to repair the tunica, and to prevent an autoimmune reaction against the testicle and resultant sterility (21).
Scrotal Masses
Ultrasound is very sensitive for the identification of scrotal masses, and can help differentiate intratesticular masses from extratesticular masses. The majority of extratesticular masses are benign, while intratesticular masses must be presumed to be neoplastic until proven otherwise. Testicular cancer accounts for 1% to 2% of all malignant tumors in men and is the fifth leading cause of death in men aged 15 to 34 years (22). The majority of testicular tumors are of germ cell origin; seminoma is the most common cell type. If ultrasound demonstrates an intratesticular mass, urgent urologic consultation is required. Common extratesticular scrotal masses include hydroceles, spermatoceles, varicoceles, and inguinal hernias.
IMAGE ACQUISITION
Ultrasound Technique
The patient should be placed in a supine position and made as comfortable as possible. The scrotum is elevated and immobilized by a towel rolled and placed between the patient’s thighs behind the scrotum (Fig. 19.1). The penis should be folded back onto the patient’s abdomen and covered with a towel. Ample amounts of warm gel should be used. A high-frequency linear array transducer provides the greatest detail and resolution (Fig. 19.2). Frequencies used range from 5 to 10 MHz, with lower frequencies being reserved for settings where increased tissue penetration and depth of field are needed. In some circumstances a standard curved transducer is required due to scrotal swelling and the need to image to a greater depth ( VIDEO 19.1).
VIDEO 19.1).
 VIDEO 19.1).
VIDEO 19.1). FIGURE 19.1. Patient Preparation for Testicular Ultrasound. Note the scrotum is supported for patient comfort and to facilitate testicular scanning. |
Scanning Protocol
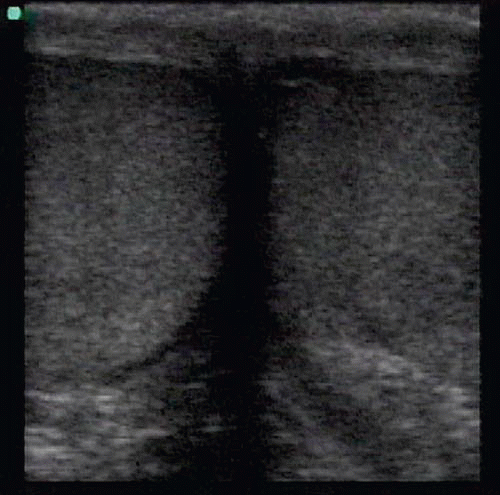
When scanning the scrotum it is important to start with the unaffected testicle. This will allow for comparison of size, texture, and echogenicity between the testicles, as well as allowing for the Doppler settings to be oriented toward the unaffected side. A standard protocol should be followed to completely visualize the scrotal contents. Both testicles should be scanned in their entirety in the sagittal and transverse planes. In addition, a transverse view across the median raphe should be included to compare the gray scale anatomy and blood flow patterns between testicles (Fig. 19.3).
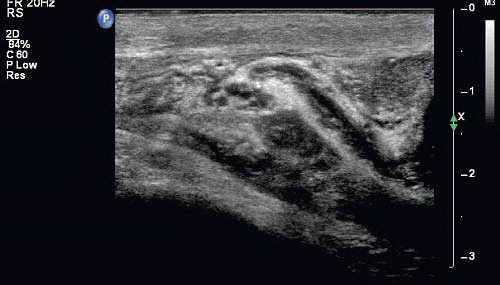
The normal sonographic appearance of the testicle has been described as similar to the liver, with a homogeneous, uniform echogenic pattern (Fig. 19.4). The mediastinum testis appears as a bright echogenic band running in the long axis of the testicle (Fig. 19.5). Attention should also be focused in the epididymis as it courses superiorly and posterior to the testicle (Fig. 19.6). Sonographically, the epididymis is usually isoechoic when compared to the testicle. The head is the most prominent portion, and the body and tail may be difficult to clearly visualize in its normal state.
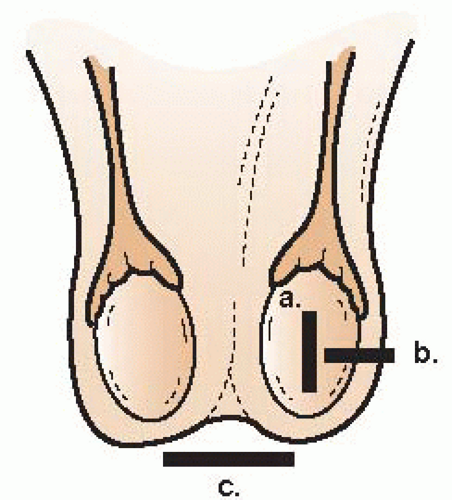 FIGURE 19.3. Transducer Placement for Ultrasound of the Testicle. a, sagittal orientation; b, transverse view; c, transverse comparative view of both testicles. |
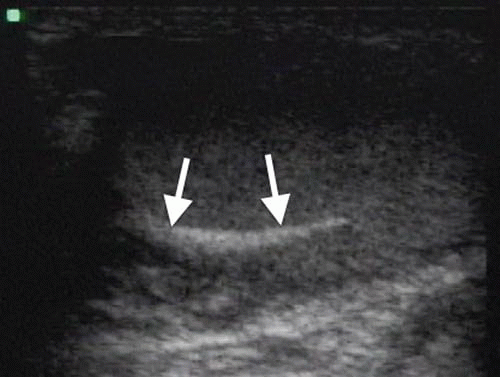 FIGURE 19.5. Sagittal Image of Normal Testis Showing Mediastinum Testis as an Echogenic Band (Arrows). |
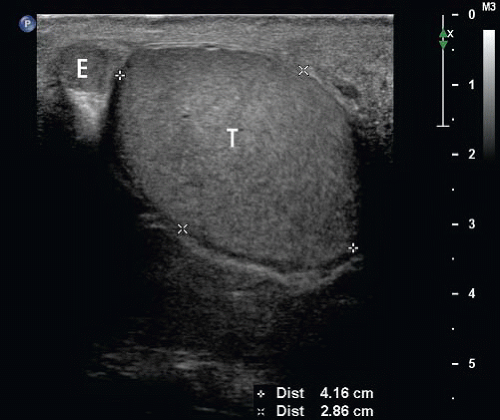 FIGURE 19.6. Normal Testis. Sagittal B-mode image of a normal testis showing testicle (T) and epididymis (E). |
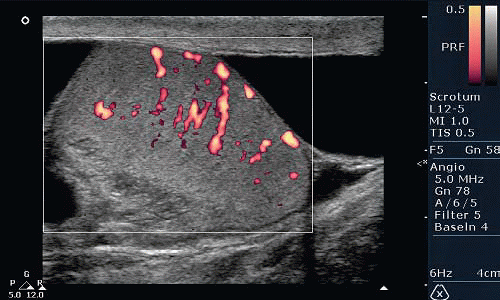
After a thorough survey of the testicle in B-mode imaging, color or power Doppler should be used to identify intratesticular vessels (Fig. 19.7). This is best achieved in the transverse plane near the mediastinum testis. Spectral Doppler interrogation should then be used to identify both arterial and venous waveforms. It is important to demonstrate both arterial and venous flow to exclude testicular torsion with a high degree of certainty. Side-by-side comparisons should be performed to assess for symmetric flow, and any difference noted should raise the clinician’s suspicion for an incomplete torsion or torsion-detorsion.
The spermatic cord is located superior to the testicle. Arterial waveforms obtained in this area will have a high resistive pattern consistent with peripheral vessels. The spermatic cord should be surveyed for evidence of a varicocele if clinical suspicion exists (Fig. 19.8).
Doppler
An understanding of Doppler ultrasound is crucial to evaluating the patient with suspected testicular torsion or scrotal pain. The ultrasound transducer emits and receives ultrasound frequencies; the central processing unit in turn converts the signal into ultrasound images. When an ultrasound wave strikes a moving object, such as a blood cell inside a vessel, shifting of the original ultrasound frequency occurs. The difference between the original and returned frequency is known as Doppler shift. The magnitude of the frequency shift is dependent on the angle at which sound strikes the moving object, as well as the direction and speed of the object. The usual frequency range of Doppler frequency shifts that occurs in normal circumstances in situations involving blood flow is measured in kilohertz. These shifts can provide important diagnostic information regarding flow in the testicle.
Two main types of Doppler are used in scanning the testicles, color Doppler imaging (CDI) and spectral Doppler. CDI displays Doppler shift overlaid on a gray scale B-mode image, which provides information regarding flow velocity and flow direction. Colors are assigned to velocities either toward or away from the transducer, with the intensity of color increasing with increased velocity. Shift toward the transducer is color coded in one color, and shift away from the transducer is coded in another. Power color Doppler displays only the intensity of the Doppler shift, without information regarding the direction of shift (Fig. 19.7). In testicular ultrasound, the detection of flow is the most important use of Doppler, and the increased sensitivity in detecting lower-flow states makes power Doppler imaging preferable to color Doppler for the evaluation of the testicles and scrotum.
Color and power Doppler are both helpful in identifying flow and excluding complete testicular torsion from arterial compromise. It is important to note that partial torsion, or early torsion where venous occlusion is the principal finding, is best excluded using spectral Doppler with the identification of venous flow by the presence of a spectral venous waveform. Spectral Doppler allows quantification of velocities and differentiates between arterial and venous blood flow (Figs. 19.9 and 19.10). The centripetal testicular arteries have a characteristic low-resistive pattern, with a low systolic peak and a wide diastolic peak. The testicular veins display a low-flow, phasic pattern (Fig. 19.10). It is important to document both arterial and venous waveforms during an exam for possible torsion. During torsion, the venous flow pattern is lost first, followed by dampening of the arterial waveform, and then all flow to the testicle is lost. By seeing both arterial and venous spectral waveforms, torsion and incomplete torsion can be essentially ruled out.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree