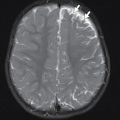
Most pediatric imaging procedures do not require sedation. There are patients, though, who will require some level of sedation in order to obtain a meaningful imaging study. The reasons for sedation are many but include anxiety, painful condition (such as fracture), age of the child (younger children tend to be less cooperative), or study length. Lengthy studies (e.g., extensive magnetic resonance imaging of the brain or spine), studies with painful procedures, children with complex medical conditions in which sedation may be problematic (such as those with cardiac or pulmonary issues), children with tenuous airways or impending airway compromise, or children with medical conditions that the clinician is not familiar or comfortable with should prompt consultation with a pediatric anesthesiologist (or an anesthesiologist who is comfortable and qualified to treat children, including those with complex medical conditions). If such consultation is not available, then consideration should be given to transferring the child to the nearest pediatric facility for the study and further care.
An excellent adjunctive resource to encourage patient cooperation, improve patient comfort, and complete a required imaging study is a child life specialist. Child life specialists use distraction and coping techniques at an age-appropriate level and have been shown to be beneficial in relieving anxiety and increasing cooperation in pediatric patients and to increase family satisfaction with care.
The Guidelines for Monitoring and Management of Pediatric Patients Before, During, and After Sedation for Diagnostic and Therapeutic Procedures state that the goals of sedation are as follows :
- 1.
To guard the patient’s safety and welfare.
- 2.
To minimize physical discomfort and pain.
- 3.
To control anxiety, minimize psychological trauma, and maximize the potential for amnesia.
- 4.
To modify behavior and/or movement so as to allow the safe completion of the procedure.
- 5.
To return the patient to a state in which discharge from medical/dental supervision is safe, as determined by recognized criteria.
Training and credentialing for pediatric sedation should be held by all personnel involved in the sedation procedure. Appropriate equipment for pediatric patients should be available, keeping in mind that requirements vary from child to child, with age, weight, and underlying medical conditions and usage during the sedation process being given consideration. The American Academy of Pediatrics (AAP), the American Academy of Dentistry, the American College of Emergency Medicine, and the Society of Anesthesiologists have all issued guidelines and recommendations addressing best practices for pediatric sedation outside of the operating room by nonanesthesiologists. Continuous monitoring before, during, and after the sedation is indicated; monitoring during sedation should, preferably, be performed by personnel not directly involved in the sedation itself. Studies have noted that despite improvement in pediatric sedation practices, there is a persistent rate (although low) of life-threatening events, including apnea, airway obstruction, and laryngospasm.
Patient safety should always be a priority before, during, and after the sedation process. Sedation outside of the operating theater in an emergency department setting is safe and practical, but there are associated risks. Children younger than 6 years of age are particularly at high risk for sedation-related adverse events due to effects on respiratory drive and protective airway reflexes. , Clinicians should have the clinical skills necessary to rescue patients from an unintended deeper level of sedation, which can occur in the course of the sedation process. A study looking at sedation and general anesthesia for pediatric patients undergoing computed tomography or magnetic resonance imaging found the rate of hypoxemia to be 2.9% and that respiratory events were more likely to occur in children with an American Society of Anesthesiologists (ASA) class of III or IV. Prompt recognition of an event and intervention occurred, and no children had sequelae as a result of their respiratory event, highlighting the importance of proper training of sedation personnel and the availability of appropriate equipment. Interestingly, this study also highlighted the problem of inadequate sedation in their study population. The quality of the scans obtained was deemed not optimal in nearly one-third (29%) of patients, the time of sedation to the initiation of the scanning procedure was significantly longer, and some imaging procedures had to be rescheduled, contributing to increased cost and inconvenience to the patients’ families due to inadequate patient sedation. The authors proposed the identification of children who are at risk for sedation failure prior to the initiation of sedation and, in these cases, considering general anesthesia for their imaging procedure.
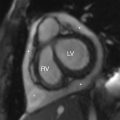
Risk factors for inadequate sedation or failure of sedation include older children, children with higher ASA class, and use of a single agent (benzodiazepines), highlighting that some populations may require general anesthesia. General anesthesia should also be considered in patients with more complex medical conditions (such as congenital heart disease) and in those where the provider is concerned that the patient may be more likely to experience complications from sedation or have inadequate sedation.
Several factors are associated with adverse events and complications from sedation, including inconsistent physiologic monitoring, inadequate presedation evaluation, lack of an independent sedation observer, medication errors, and inadequate recovery procedures. All personnel involved in sedation should have skills in pediatric resuscitation and airway management, specialty-dependent guidelines should be adopted for sedation procedures, and appropriate medications and age-specific equipment should be readily available.
The guidelines promulgated by the AAP and the American College of Emergency Medicine provide general recommendations to help ensure patient safety :
- 1.
Appropriate patient selection
- 2.
A responsible guardian (preferably two adults) to accompany the child
- 3.
Appropriate sedation facility, including personnel and equipment to rescue the decompensating child
- 4.
Back-up emergency services, if the sedation is taking place outside of the hospital setting
- 5.
Personnel, medications, and equipment available onsite that is immediately accessible
- 6.
Appropriate documentation, including informed consent outlining the indications, benefits, risks, and alternative options of the sedation procedure
- 7.
Documentation before, during, and after sedation. Weight should be recorded in kilograms and any known drug allergies should be noted.
Proper patient selection for sedation is an important step in ensuring safety and a successful sedation experience. While there is no screening test that has the ability to predict sedation complications, there are resources available to the clinician to help guide the sedation process. The ASA classification can be useful to help select which patients are candidates for sedation.
| Class I | A normally healthy patient |
| Class II | A patient with mild systemic disease (e.g., controlled reactive airway disease) |
| Class III | A patient with severe systemic disease (e.g., a child who is actively wheezing) |
| Class IV | A patient with severe systemic disease that is a constant threat to life (e.g., a child with status asthmaticus) |
| Class V | A moribund patient who is not expected to survive without the operation (e.g., a patient with severe cardiomyopathy requiring heart transplantation) |
This classification system is not intended to predict risk per se, but increasing ASA classification has been associated with increased perioperative mortality. , In the pediatric emergency department setting, an ASA classification of II or higher was associated with a higher incidence of hypoxia. Children who have an ASA classification of III or greater, an anatomy that could potentially complicate sedation (such as Pierre Robin sequence, Prader Willi syndrome, or other craniofacial developmental abnormalities), or any other anatomical or developmental issues should have anesthesiology or subspecialty consultation before sedation. , ,
It is important that the clinician has a validated, clinically useful method for assessing the quality and depth of sedation for patients undergoing sedation. The AAP, American College of Radiology, and the ASA have adopted four levels of procedural sedation. , The Pediatric Sedation State Scale is a widely used measure of the effectiveness and quality of sedation. Parameters such as control of pain, anxiety, movement, and adverse effects were taken into account in the development of this proposed scale. Another useful scale that is simple to apply clinically and has been validated in pediatric patients is the University of Michigan Sedation Scale. , Other sedation scales used to assess the depth of sedation include the Observer’s Assessment of Alertness/Sedation scale, which has been validated in children but has limited ability to differentiate between deeper levels of sedation. , The Vancouver Sedative Recovery Scale is able to differentiate deeper levels of sedation but is one of the more complex scales available, potentially making clinical application difficult. ,
| SEDATION LEVEL | PATIENT RESPONSE |
| Minimal | Normal response to verbal commands |
| Moderate | Purposeful response to verbal commands or light touch |
| Deep | Difficult to arouse; purposeful response to painful or repeated stimulation |
| General anesthesia | No response |
| VALUE | PATIENT STATE |
| 0 | Awake and alert |
| 1 | Minimally sedated: tired/sleepy; appropriate response to verbal conversation and/or sound |
| 2 | Moderately sedated: somnolent/sleeping; easily aroused with light tactile stimulation or a simple verbal command |
| 3 | Deeply sedated: deep sleep; aroused only with significant physical stimulation |
| 4 | Unarousable |
| STATE | BEHAVIOR |
| 5 | Patient is moving (purposefully or nonpurposefully) in a manner that impedes the proceduralist and requires forceful immobilization. This includes crying or shouting during the procedure, but vocalization is not required. Score is based on movement. |
| 4 | Moving during the procedure (awake or sedated) that requires gentle immobilization for positioning. May verbalize some discomfort or stress, but there is no crying or shouting that expresses stress or objection. |
| 3 | Expression of pain or anxiety on face (may verbalize discomfort), but not moving or impeding completion of the procedure. May require help positioning (as with a lumbar puncture) but does not require restraint to stop movement during the procedure. |
| 2 | Quiet (asleep or awake), not moving during procedure, and no frown (or brow furrow) indicating pain or anxiety. No verbalization of any complaint. |
| 1 | Deeply asleep with normal vital signs, but requiring airway intervention and/or assistance (e.g., central or obstructive apnea, etc.). |
| 0 | Sedation associated with abnormal physiologic parameters that require acute intervention (i.e., oxygen saturation <90%, blood pressure 30% lower than baseline, bradycardia receiving therapy) |
Much debate has been made on the necessity of nil per os (NPO) status and the ability to engage in sedation. There are NPO guidelines that are used to determine when it is considered safe to administer various levels of sedation and anesthesia in patients undergoing elective procedures. , The concern is whether the risk for aspiration or other adverse event is increased when administering sedation for radiologic or other procedures when a patient has not been NPO for a given length of time. There has been differing guidance among professional societies addressing NPO status and sedation in a setting that is considered more urgent or emergent. , A very large study of nearly 140,000 children, conducted by the Pediatric Sedation Research Consortium, examined the relationship of NPO status and aspiration events (defined as an episode of emesis accompanied by a change in respiratory status of the patient or a new radiographic finding). NPO status was known for 107,947 patients, where 25,401 (23.5%) were non—NPO patients. NPO status was defined as no solid food intake for 8 hours, no nonclear fluid intake for at least 6 hours, and no intake of clear liquids for at least 2 hours. Aspiration occurred in 8 of 82,546 NPO patients compared to 2 of 25,401 non—NPO patients. Major complications occurred in 46 of 82,546 NPO patients compared to 15 of 25,401 non—NPO patients. In summary, aspiration was uncommon (<1 event per 10,000 patients) and NPO status for liquids and solids was not an independent predictor of major complications or aspiration. While debate continues regarding sedation and NPO status in the pediatric population and the incidence of aspiration or adverse effects is low, the clinician should consider the indications, urgency, risks, and benefits of sedation for imaging studies.
If the decision is made to utilize sedation in the emergency department or urgent care setting, there are a variety of agents available. Clinicians should be familiar with the indications, benefits, risks, side effects, and pharmacokinetics of whatever agent (or agents) they choose to utilize for sedation and/or anxiolysis. When considering agents, the lowest dose needed with the highest therapeutic index to accomplish imaging should be selected. Long-acting agents are rarely indicated for imaging studies and should generally be avoided. If an imaging study is particularly lengthy, such as magnetic resonance imaging of the brain and complete spine, then anesthesiology should be consulted. Options include analgesic agents, sedative-hypnotic (anxiolytic) agents, and agents in their own categories, such as ketamine, propofol, and nitrous oxide.
Once sedation is completed, patients should be monitored (heart rate, respiratory rate, pulse oximetry, and blood pressure) for return to baseline status. Once patients have returned to their baseline mental and ambulatory status, they may be discharged. Discharge instruction appropriate to the agent and level of sedation used should also be provided to the patient’s caregiver.
Analgesic agents
These agents are not commonly used for imaging sedation, but adequate pain control is important to maximize the chances of obtaining a meaningful imaging study. Pain control with appropriate agents is important for fracture imaging. An excellent example of this is imaging supracondylar fractures; a true lateral image is desired to assess the type/degree of the injury (for example, type I, II, or III fractures), which is important for planning appropriate treatment.
Morphine
This agent has been found to be as efficacious as fentanyl in the control of pain in pediatric patients. However, like all opioids, morphine can cause respiratory depression and decrease blood pressure through peripheral vasodilation. Morphine is generally not the preferred agent for sedation. This agent should be used cautiously in patients with either airway or cardiovascular compromise. A usual dose is 0.1 mg/kg intravenously.
Fentanyl
Fentanyl is a synthetic opioid with a potency of approximately 100 times that of morphine. This agent has a rapid onset (5 minutes) but a short duration of action (less than 1 hour). Initial intravenous dosing is 1 µg/kg. While these properties make fentanyl a good analgesic option, there are several potential effects associated with its use. These effects are primarily respiratory (hypoxemia, respiratory depression, and apnea), are more likely when fentanyl is combined with another sedative agent, and occur early after administration (5–15 minutes). ,
Chest muscle rigidity (sometimes known colloquially as rigid chest syndrome) is a well-described and feared complication of fentanyl usage but is not common. , The result of this phenomenon is an inability to ventilate and is a life-threatening complication. While large doses have been associated with this condition (>4 µg/kg), chest wall rigidity has been reported in patients with appropriate intravenous doses, particularly with rapid administration (i.e., a “push” dose). ,
Intranasal fentanyl is being increasingly utilized. This method of delivery is quite advantageous, being effective, easy, painless, and rapid. , A typical dose is 2 µg/kg, with a maximum of 100 µg per dose, which can be repeated once within 5 minutes if clinically indicated.
Sedative-hypnotic agents
Etomidate
Etomidate has a rapid onset of action (less than 30 seconds) and brief duration (usually less than 15 minutes); the usual dose is 0.1–0.3 mg/kg intravenously with 0.05 mg/kg bolus given as clinically indicated. , This agent has several advantages in addition to its rapid onset, including reducing intracranial pressure and maintaining hemodynamic status. Adverse effects include respiratory depression, vomiting, and nonepileptiform myoclonus. , Since etomidate inhibits endogenous steroid production, it should not be used in patients with known adrenal insufficiency and should be used with caution in patients with septic shock, since adrenal suppression may be present in patients with this condition. For this reason, etomidate infusions are not recommended.
Propofol
A nonopioid agent that has been used extensively in operative and intensive care settings, propofol has been increasingly used for procedural sedation in emergency departments. , There are several properties of this agent that make it attractive for sedation use. This agent has a rapid onset of action and recovery (seconds) and lowers intracranial pressure, making its use especially appropriate for neuroimaging of patients with head injury. Propofol may be given as a bolus or as an infusion. A usual starting dose is 100 to 150 µg/kg per minute, with gradual titration of the dose to achieve effect, with a maximum of 200 µg/kg per minute. , , If propofol is being used as a bolus, the initial dose is 1 to 2 mg/kg, with additional boluses of 0.5 mg/kg, every 3 to 5 minutes as clinically indicated to maintain sedation. , However, there are several potentially adverse effects associated with the use of propofol. This agent does not possess analgesic properties, and when analgesia is desired, propofol may be used in combination with other agents that provide analgesia, such as morphine, fentanyl, or ketamine. These combinations may increase the chance for respiratory depression, bradycardia, and hypotension and may also exceed the intended level of sedation. , One study found that in patients undergoing fracture reduction with propofol and fentanyl, 31% of patients experienced oxygen desaturation and 25% of patients required maneuvers to address respiratory decompensation. Propofol should be used with caution in hypovolemic patients or patients with reduced cardiac function/output; these patients should receive an intravenous fluid bolus prior to being given propofol. , , Propofol also causes pain during administration, which may be reduced with the administration of lidocaine (0.5 mg/kg) prior to propofol administration or in combination with another analgesic agent. Adverse effects from propofol use include respiratory depression, apnea, and hypotension (up to 5% of patients) , ; respiratory arrest and cardiac arrest have been reported but are rare. ,
An allergy to eggs has traditionally been a contraindication to propofol use, but studies have shown that propofol has been safely used in patients with a history of egg allergy. , Propofol infusion syndrome has been described in pediatric patients being cared for in an intensive care setting. This is a constellation of refractory bradycardia in combination with metabolic acidosis, rhabdomyolysis, and hyperlipidemia that progresses to asystole. This syndrome is associated with prolonged propofol infusion or high doses of propofol (>4000 µg/kg/24 hours); it is usually fatal and its exact etiology is unknown. ,
Dexmedetomidine
This agent is a selective alpha-2-adrenergic receptor agonist. Dexmedetomidine has primarily sedative properties but has some analgesic properties. The main advantage of this agent is excellent sedation with minimal respiratory depression, and dexmedetomidine has been found to be safe in pediatric procedures requiring sedation but not necessarily analgesia. For pediatric patients, doses higher than those used in adult patients are used: 2 to 3 µg/kg intravenous bolus, followed by a 1 to 2 µg/kg/hour infusion. , Dexmedetomidine has also been found to be effective when given intranasally at doses of 2.5 to 3 µg/kg/dose. , , Another advantage of this agent is its use in patients with autism. , Serious adverse effects, such as laryngospasm, are not common, although 4% of patients receiving this medication had cardiovascular effects (heart rate and blood pressure increases or hypotension); hypertension has been reported in 5% of patients given dexmedetomidine and is associated with younger age, higher doses, and multiple boluses.
Midazolam
Midazolam is a rapid-acting, short-duration agent that when given intravenously has anxiolytic, amnestic, and muscle relaxant actions. It can be combined with fentanyl to provide moderate sedation; a usual dose is 0.1 mg/kg. , , A distinct advantage of midazolam is that there are other routes in which this medication can be given, including oral, sublingual, and intranasal. The preferred method of delivering this medication intranasally is with an atomizer, which produces better absorption and provides better patient comfort when compared to directly instilling the medication. The intranasal dose is higher than the intravenous dose, using 0.2 mg/kg with a maximum of 10 mg per dose. , , Adverse effects include respiratory depression and apnea; this risk is increased with coadministration of opioid medications. Paradoxical reactions, such as irritability and aggressive behavior, have been reported. Paradoxical reactions and respiratory depression can be reversed with flumazenil. Flumazenil should be used with caution in patients with a known seizure disorder, as this medication can lower a seizure threshold and precipitate a seizure.
Other agents
Ketamine
One of the most commonly used agents for pediatric sedation, this agent produces a dissociative state while at the same time providing both analgesic and sedative effects. Ketamine is a derivative of phencyclidine, more commonly known as PCP, and produces its effects by binding to N -methyl-d-aspartate (NMDA) receptors. This agent is rapidly acting and has a short duration of action. Ketamine is most often utilized for completion of brief, painful procedures, such as fracture reduction. In addition to excellent and effective sedation and analgesia, ketamine also provides amnesia and immobilization while preserving airway protective reflexes and spontaneous breathing. , The usual initial intravenous dose of ketamine is 1 to 1.5 mg/kg as a bolus, followed by repeated doses of 0.5 to 1 mg/kg as clinically indicated. Notably, providing initial pain management with an opioid is not a contraindication for procedural sedation with ketamine. Although this does increase the incidence of vomiting and the need for oxygen use, it does not increase the incidence of adverse effects.
Ketamine can be combined with propofol. When ketamine is used in this manner, the dose is reduced to 0.5 mg/kg. A suggested dosing regimen is 0.5 mg/kg of ketamine, followed by 0.5 mg/kg of propofol, with an additional dose of 0.5 mg/kg of propofol given as clinically indicated. ,
Intramuscular (IM) dosing of ketamine is also an option. If ketamine is given through this route, the dose must be increased to achieve effect. A typical IM dose is 4 to 5 mg/kg; if clinically indicated, a second dose of 2 to 4 mg/kg can be given 10 minutes later.
Adverse effects from ketamine typically are vomiting and recovery reactions (irritability, hallucinations, and agitation). , Although they are the most serious potential complications, laryngospasm and apnea are not commonly seen, , are usually brief, and can be effectively managed the majority of the time with positive pressure bag-mask ventilation. , Several large studies have documented adverse effects from ketamine (apnea [<1%], laryngospasm [<1%], and oxygen desaturation [3%]), which are independently associated with young age (<2 years old), intravenous doses greater than an initial dose of 2.5 mg/kg or total dose >5 mg/kg, or coadministration of a benzodiazepine or atropine; vomiting (8%) was associated with older age and high intravenous dosing. , The IM route of administration is more commonly associated with vomiting and prolonged recovery times. This route does not appear to be associated with increased incidence of laryngospasm, as once thought. , While ketamine has been shown to cause hypersalivation, routine administration of atropine or glycopyrrolate is not recommended, as the risk of laryngospasm due to hypersalivation is not decreased with these agents in large studies. Routine administration of midazolam is also not recommended as a means to mitigate vomiting and/or the emergence reaction sometimes seen with ketamine use. , Vomiting is the most commonly seen adverse effect from ketamine administration, and some authors recommend routine administration of odansetron for patients undergoing sedation with ketamine. , ,
Ketamine is contraindicated in patients who are less than 3 months of age or those patients who have had severe emergence reactions in the past. Ketamine is relatively contraindicated in patients who have increased intraocular pressure (the evidence for this is debated), increased intracranial pressure (this is a matter of ongoing debate as well), hypertension, and thyroid disease. ,
Intranasal ketamine delivery has recently been investigated and has been found to be effective with few adverse effects, the most common of which was vomiting. As with the intravenous delivery route, routine coadministration of a benzodiazepine was not supported, as has been reported in previous studies with ketamine in the pediatric population. , Patients did appear to have a higher incidence of emergence reactions with the intranasal route, but there was no consistent definition of what constituted an emergence reaction. , , The perceived satisfaction of the level of sedation with intranasal ketamine for sedation has not been consistent in the literature, and doses have ranged from 2 mg/kg to 9 mg/kg. , Analgesia has been reported to be satisfactory. , The superiority of intranasal ketamine versus other agents for sedation has not been proven, however, and studies using intranasal ketamine for fracture reduction are lacking. The lack of rigorous trials on intranasal ketamine use in the pediatric population makes its routine for use for sedation difficult at this time, but there does appear to be promise for use in sedation for brief procedures, such as obtaining an imaging study.
Summary
While sedation or anxiolysis for pediatric radiologic procedures is not always clinically needed, appropriate use of agents for these purposes will allow for patient comfort and minimize motion, resulting in a meaningful radiologic study for management purposes. Clinicians should be familiar with the indications, dosages, and potential adverse effects of whatever agent is chosen, as well as airway rescue techniques should a patient progress to unintended levels of sedation. Properly trained staff familiar with sedation practice and principles will maximize sedation success and minimize complications. The choice of sedation/anxiolytic agent should consider the lowest, most effective dose required to achieve the desired imaging study.
References
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree