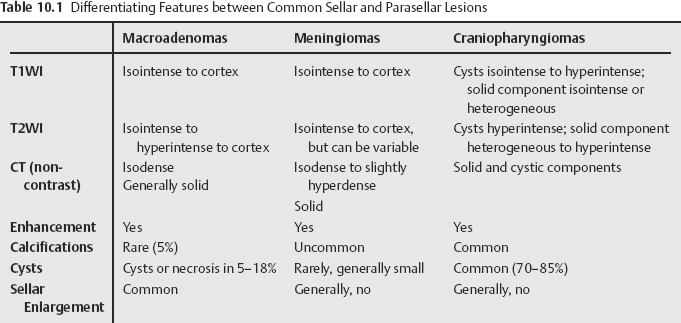
10 The normal pituitary gland generally measures between 4 to 7 mm in height, depending on age, sex, and pregnancy status, and generally does not exceed 10 mm. The posterior lobe is hyperintense on T1-weighted magnetic resonance [MR] images (T1WI) due to vasopressin and should always be seen in normal children and infants, although the incidence of this finding decreases with age. Sellar and parasellar lesions most commonly arise from the pituitary gland or adjacent structures such as vessels, dura, or developmental remnants. Adenomas, meningiomas, craniopharyngiomas, and vascular lesions account for ~75% of sellar and parasellar lesions. These lesions comprise 10 to 15% of all intracranial neoplasms and one third to one half of sellar and parasellar masses. They are divided into macroadenomas and microadenomas based on size. Macroadenomas are greater than 10 mm and commonly grow into the suprasellar region, but may extend into the sphenoid sinus or bone and be more invasive, and may invade the cavernous sinus. Imaging features are detailed in Table 10.1. Pituitary apoplexy refers to hemorrhage and necrosis of an adenoma due to tenuous blood supply from the hypophyseal portal system. Imaging demonstrates blood products, commonly high signal on T1WI and T2WI (T2-weighted MR images). Apoplexy is differentiated from Sheehan’s syndrome, which is postpartum or peripartum pituitary hemorrhage and necrosis. Microadenomas are less than 10 mm in size. Their appearance is There may be associated sellar erosion, focal elevation of the superior margin of the pituitary, and infundibular deviation. Dynamic images may show relatively less enhancement of an adenoma with respect to a normal gland. On delayed images taken 30 to 40 minutes following injection, adenomas may have delayed enhancement with respect to a normal pituitary gland. They may have hemorrhage resulting in high signal on T1WIs. Meningiomas are the second most common sellar/parasellar lesion; in this location, they represent 5 to 11% of all meningiomas. They are more common in women. They are generally homogeneously solid tumors; however, they may occasionally contain necrosis, scarring, cystic degeneration, and calcifications. Imaging features are detailed in Table 10.1. Craniopharyngiomas arise within squamous epithelial remnants or remnant ectoblastic cells of Rathke’s pouch and the craniopharyngeal duct and account for 3 to 5% of all intracranial masses. There is a bimodal age distribution, occurring from 5 to 14 years of age, with a second peak at 65 to 74 years of age. They tend to recur and invade local structures and adhere to surrounding structures, including vessels. They are typically suprasellar and may extend into the sella. They can have cystic and solid components. Rim or nodular calcification is present in 80 to 87%. Calcification is more common in children (90%) than in adults (50 to 70%) The imaging features are outlined in Table 10.1.
Sellar and Parasellar Lesions
Pituitary Adenomas
Meningiomas
Craniopharyngiomas
Rathke’s Cleft Cysts
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree