Septic Arthritis
Rick W. Obray
Cathleen F. Magill
Etiology and Epidemiology.
Septic arthritis occurs in all age-groups. In pediatric patients, the hip, knee, and ankle are the most commonly affected joints. In adults, the knee is by far the most commonly affected joint, followed by the hip and shoulder. Patients with a history of intravenous drug abuse (IVDA) often present with involvement of the sternoclavicular and sacroiliac joints, as well as the spine.
Septic arthritis most commonly results from hematogenous seeding of the highly vascular synovial membrane in the context of bacteremia. Much less common etiologies include penetrating trauma, nonpenetrating trauma to a joint, and introduction of bacteria during joint procedure.
Neisseria gonorrhoeae is the most common cause of septic arthritis in the United States, with the highest prevalence among young sexually active adults and homosexual men. Of all nongonococcal cases, Staphylococcus is the most frequent etiologic agent, and is particularly represented in patients with a history of diabetes or rheumatoid arthritis. Other common bacterial agents include Streptococcus species, Pseudomonas aeruginosa, and Escherichia coli. Although Hemophilus influenzae formerly accounted for a large share of cases in children younger than 2 years, the advent of the Hemophilus influenzae type b (Hib) vaccine has reduced the number of cases to near extinction.
Easy hematogenous ingress of bacteria is facilitated by the absence of a limiting basement membrane under the highly vascular synovium. Once inside this space, egress is difficult, and rapid destruction of the joint space occurs. Risk factors for septic arthritis include unprotected sexual intercourse, diabetes, cancer, chronic liver disease, chronic alcoholism, corticosteroid therapy, IVDA, sickle cell disease, previous joint damage, and hypogammaglobulinemia.
Symptoms and Signs.
Most patients present with the acute onset of a warm, erythematous, edematous, painful joint with associated fever and malaise. In 80-90% of patients, septic arthritis is monarticular. When it is polyarticular, usually only two to three joints are involved.
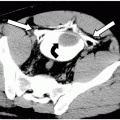
The diagnosis of septic arthritis is usually made clinically. Leukocytosis is often present in children, but not as commonly in adults. Erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) levels are also frequently elevated. The primary tool for analysis of septic arthritis is the joint aspirate (Gram stain, cell count, and culture). Most clinicians perform aspiration of the knee joint at the bedside. Aspiration of the hip and shoulder often requires fluoroscopic guidance by a radiologist.
Differential Diagnosis.
The differential diagnosis should be tailored based on each patient’s risk factors and comorbidities. A general differential includes all of the inflammatory arthritides—rheumatoid arthritis, gout, calcium pyrophosphate dihydrate deposition (CPPD) syndrome, Reiter’s syndrome, arthritis associated with inflammatory bowel disease and psoriatic arthritis. However, in contrast with septic arthritis, these arthritides tend to be polyarticular. Synovial osteochondromatosis and pigmented villonodular synovitis are also in the differential diagnosis. The differential diagnosis in children should be expanded to include trauma (epiphyseal fracture, child abuse), Legg-Calve-Perthes disease, leukemia, slipped capital femoral epiphysis, and transient synovitis.
Indications.
It is reasonable to initiate any evaluation of an acute articular process with radiographs. In children, they are especially important for ruling out trauma.