Septic Emboli
Aqeel A. Chowdhry, MD
Tan-Lucien H. Mohammed, MD, FCCP
Key Facts
Terminology
Septic embolism occurs when infected purulent material is dislodged and embolizes to lung
Imaging Findings
Nodules or wedge-shaped opacities
Usually small (< 3 cm diameter) and few in number
Basilar and peripheral
Cavitation (50%)
Cavitation more common in nodules than wedge-shaped opacities
Rapid cavitation, typically over 24-48 hours
Nodules often in various stages of cavitation: No wall to thin wall
Visible embolus extremely uncommon
Pleural effusions (70%)
CT may be abnormal before blood cultures positive
Top Differential Diagnoses
Pulmonary Emboli
Lung Abscess
Metastases
Pathology
Source of septic emboli
Indwelling venous catheters
Periodontal disease
Skin infections
Clinical Issues
Median duration of symptoms before diagnosis: 18 days
Diagnostic Checklist
Septic embolism in patient with multiple pulmonary nodules and extrapulmonary focus of infection
TERMINOLOGY
Definitions
Septic embolism occurs when infected purulent material is dislodged and embolizes to lung
IMAGING FINDINGS
General Features
Best diagnostic clue: Multiple nodular opacities rapidly evolving into cavitary nodules
Patient position/location: Basilar and peripheral
Size: Usually small (< 3 cm diameter)
Morphology: Nodules more common than wedge-shaped opacities
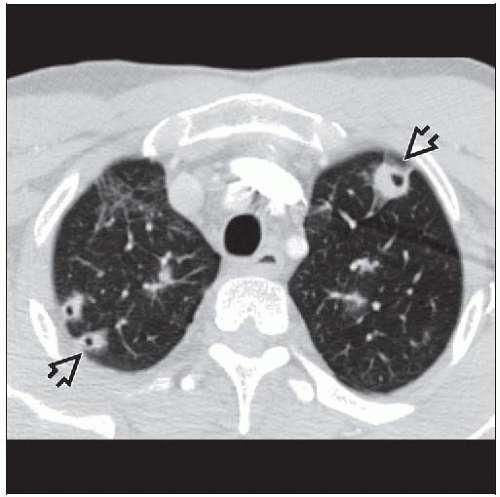
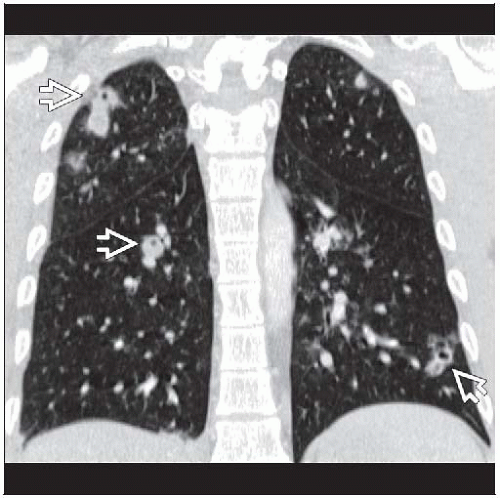
CT Findings
Morphology
Nodules
Majority < 3 cm diameter although they can grow much larger
Edges indistinct, may have halo sign
Air bronchograms seen in 25%
Average number 15 per patient
Wedge-shaped opacities
Peripheral heterogeneous density
Edge may enhance with intravenous contrast
Average number 6 per patient
Cavitation (50%)
More common in nodules than wedge-shaped opacities
Thickness of cavity wall varies from thick to thin (reflects stages of evolution)
Usually no air-fluid level
Distribution
More common in bases (reflects gravity-dependent blood flow)
Bilateral, right lung more nodules than left
Peripheral (within 2 cm of pleura) (90%)
Feeding vessel sign
Vessel leading directly to edge of nodule, found in up to 60-70% of patients
MDCT with reconstructions shows that vessel sign usually represents pulmonary veins coursing next to nodule
Evolution
Rapid cavitation, typically over 24-48 hours
Nodules often in various stages of cavitation: No wall to thin wall
May change in number or appearance (size or degree of cavitation) from day to day
Resolution: May resolve completely with antibiotic therapy, may also result in small residual linear or nodular scars
Pulmonary artery
Visible embolus extremely uncommon
Adenopathy (20%)
Pleural effusions (70%)
May be bilateral or unilateral
Small common; if loculated consider empyema
Heart
May see valve vegetations, especially with gated studies
Indwelling central catheters or pacemaker lead common source
Examine closely for adherent clot (may be source of infection)
May have infection in other organs seen on chest CT (liver abscess, osteomyelitis, renal abscesses)
Radiographic Findings
Radiography: Poorly defined nodular opacities often small and few in number; may be easily missed
Imaging Recommendations
Best imaging tool: CT may be abnormal before blood cultures are positive
Protocol advice: ECG-gated MDCT may be useful to look for valve vegetations
Echocardiographic Findings
Transesophageal echocardiography is procedure of choice to examine valves for vegetations
DIFFERENTIAL DIAGNOSIS
Pulmonary Emboli
Visible emboli in pulmonary artery, uncommon with septic emboli
With infarcts
Infarcts uncommon, usually require some underlying cardiopulmonary disease
Pulmonary infarctions rarely cavitate, cavitation common with septic emboli
Pleural effusions nearly always present with infarction, also common with septic emboli
Lung Abscess
Typically have air-fluid level, less common in septic emboli
Evolves more slowly over days and weeks
Fewer in number
Etiology varies
Periodontal disease
Gravity-dependent segments: Posterior segments of upper lobe or superior segments of lower lobes
Polymicrobial, especially anaerobic organisms like Peptostreptococcus or Fusobacterium
Metastases
Cavitation seen with
Squamous cell carcinoma, sarcomas, most common cell types
Do not rapidly evolve and do not respond to antibiotic therapy
Usually more numerous in number
Usually variable in size
Also have feeding vessel sign
Wegener Granulomatosis
Nodules with varying degrees of cavitation
Do not rapidly evolve
May have subglottic tracheal stenosis
Respond to steroid therapy but not to antimicrobial treatment
Rheumatoid Nodules
Foreign Body Embolus
Source: Catheter fragments, vertebroplasty cement, radioactive prostatic seeds
Rarely causes nodules or infraction
Tumor Embolism
Seen with hepatocellular carcinoma, renal cell carcinoma, or any tumor with extension into venous system
Rarely causes infarcts
Smaller tumors may grow and expand vessel, mass maintains shape of vessel
Intraluminal clot similar to venous embolism
PATHOLOGY
General Features
Etiology
Infective endocarditis
Occurs as result of nonbacterial thrombotic endocarditis, with injury to endothelial surface of heart
Transient bacteremia leads to seeding of lesions with adherent bacteria
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree