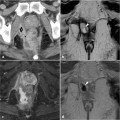
Fig. 25.1
A 40-year-old male HIV-infected patient hospitalized with sepsis. The caudalmost image from a total body CT (a) shows a right perianal abscess collection with fluid content and gas bubbles. Focused MRI better confirms the abscess process, which involves the right ischioanal fossa and levator ani muscle, as seen on the coronal T2-weighted image (b)
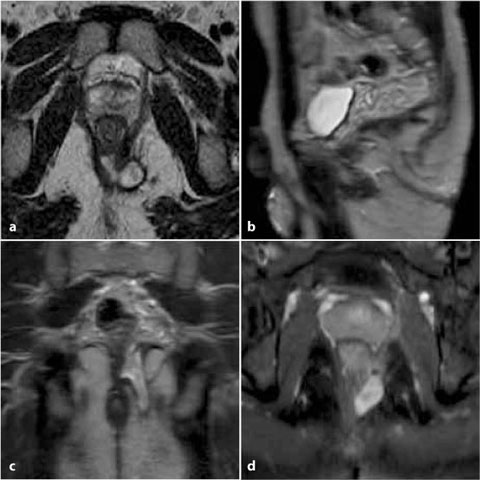
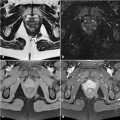
Fig. 25.2
A 37-year-old HIV-infected male homosexual with a clinical diagnosis of anal condylomas. Axial (a), sagittal (b), and coronal (c) T2-weighted images show a posterior perianal fistula and an abscess collection with involvement of the levator ani muscle; there is a secondary tract in the ischioanal space. On contrast-enhanced axial fat-suppressed (d) Tl-weighted MRI, the left perianal abscess markedly enhances. Biopsy disclosed coexistent syphilis infection
Venereal diseases (occurring in 56% of patients) include condylomas, syphilis (Fig. 25.2), gonorrhea, Chlamydia, and amebiasis, along with other peculiar HIV-associated infections such as cytomegalovirus (CMV), herpes simplex virus (HSV), and candidiasis [2, 3]. Globally, the most frequent diseases are condylomas (usually associated with oral and/or genital lesions) and ulcers (related to HSV and CMV infections) [2]. In Western countries, an increase in syphilis, mostly due to homosexual contacts, was recently reported. The variable and unspecific symptoms of syphilis consist of local pain sometimes associated with itching, tenesmus, urgency of defecation, or anal discharge, which may be purulent, mucoid, or blood-stained. Therefore, this uncommon diagnosis should be suspected in a patient who presents with anorectal lesions and particularly in active homosexual males [1, 4, 5].
Opportunistic intestinal infections account for a large proportion of the morbidity in HIV-infected patients and are usually assessed by means of microbiological and parasitic stool cultures coupled with endoscopy [9].
Diagnostic imaging procedures, particularly MRI, may have a role in visualizing abnormalities involving the anorectal tract, inflammatory lesions and their topography, and possible complications such as abscess collections, as well as in differentiating benign lesions from solid neoplastic ones [10].
Although uncommon (about 7% of cases), anal tumors are more prevalent in HIV-infected patients than in the general population. They mainly consist of squamous-cell carcinomas associated with HPV infection, Kaposi’s sarcoma, and, rarely, non-Hodgkin lymphoma [2, 3]. On CT, neoplastic lesions appear as solid soft-tissue thickenings or masses; on MRI, they are solid, T1- hypointense lesions with positive contrast enhancement, and of intermediate-to high signal intensity (usually heterogeneous in larger lesions) on T2-weighted and STIR images. In the imaging of HIV-infected patients, special attention should be paid to the presence of solid, enhancing tissue consistent with tumor as this finding indicates the need for biopsy (Fig. 25.3




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree