Shoulder
Anatomy and Techniques
Standard Position 1: Biceps Tendon
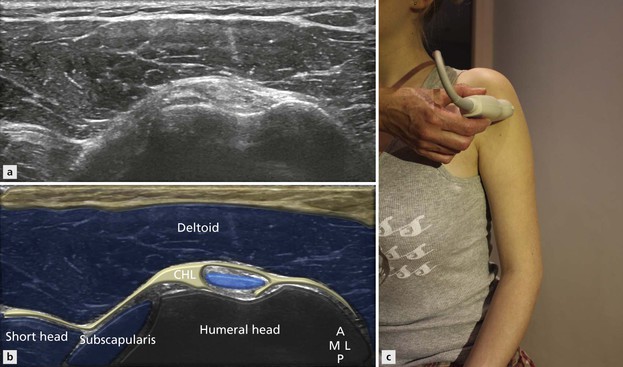
Standard Position 2: Rotator Interval
Standard Position 3: Subscapularis Tendon
Standard Position 4: Supraspinatus Tendon
Standard Position 5: Infraspinatus and Teres Minor Tendon
Standard Position 6: Supraspinatus Muscle and Acromioclavicular Joint
DYNAMIC ASSESSMENT OF BURSAL IMPINGEMENT
Overview
The important bony landmarks in the evaluation of the supraspinatus tendon are the humeral head, the coracoid, the clavicle and acromium, joined at the acromioclavicular joint. The glenohumeral joint is an inherently unstable joint and depends on the surrounding soft tissues for stabilization. Soft tissue stabilizers are divided into intrinsic and extrinsic. The most important extrinsic soft tissues are the supraspinatus tendon superiorly, infraspinatus posteriorly and subscapularis anteriorly (Fig. 1.1). The important intrinsic soft tissue stabilizers are the glenohumeral joint and capsule.

Figure 1.1 The glenohumeral joint is stabilized by a combination of the joint capsule with its condensations, the glenohumeral ligaments and the rotator cuff tendons. The coracoacromial arch overlies the supraspinatus comprising the coracoid, acromial and CAL.
Patient Position
It is important to take a history directly from the patient before the examination begins as this can often provide useful diagnostic information. The examination itself begins with a brief inspection of the shoulder, useful to detect muscle wasting. As with most ultrasound examinations the probe should be held lightly with sufficient, but not excessive, contact with the skin. Holding the probe between the thumb and adjacent fingers while resting the little finger on the patient’s skin is an ideal way of obtaining excellent contact with minimal pressure.
The cuff is examined from biceps anteriorly to teres minor posteriorly and from the acromioclavicular joint superiorly to deltoid insertion inferiorly. The examination is concentrated on the four major tendons, but it is important to have a routine to ensure that none of the other important structures is overlooked. My preference is to begin with the biceps tendon and rotator interval anteriorly, then move sequentially through subscapularis, supraspinatus and infraspinatus and teres in that order (Fig. 1.2). The examination concludes with an assessment of the posterior glenohumeral joint, infraglenoid notch, supraspinatus muscle and the acromioclavicular joint, before sweeping down to the deltoid insertion.
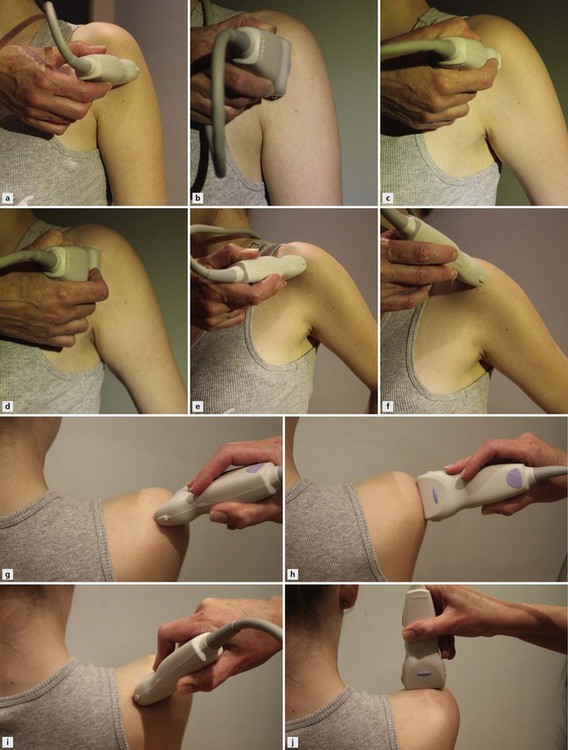
Figure 1.2 Standard ultrasound examination positions. (A, B) Dorsum of hand on patient’s knee with some shoulder extension: used to visualise biceps tendon in short and long axis. (C, D) Shoulder extended, hand by side position for subscapularis (external rotation can also be used). (E, F) Hand on back pocket: used for supraspinatus short and long axis. (G, H, I, J) Arm across anterior chest for teres minor long and short axis, supraspinatus muscle belly and acromioclavicular joint.
Standard Position 1: Biceps Tendon
Technique
The patient sits and places their hand on their knee palm upwards. This induces a little external rotation sufficient to bring the bicipital groove to an anterior position (Fig. 1.3). The groove is easily located by placing the probe in an axial plane on the anterior aspect of the humeral head. The probe is then moved superiorly and inferiorly, tracing the biceps tendon from the upper part of the groove to below its upper musculotendinous junction. The normal tendon has a bright speckled appearance in the axial plane, made up of the poorly reflective tendon fibre bundles and the hyperechoic connective tissue matrix. Care must be taken to ensure that the probe is always held at 90° to the tendon to remove the effects of anisotropy. Anisotropy is an artefact whereby areas of reduced reflectivity simulating tendinopathy occur as a result of incident echoes arriving at angles other than perpendicular and being reflected away from the tendon, rather than bouncing back to the probe to help form an image.
The probe is then rotated 90° so that the tendon can be examined in its long axis (Fig. 1.4). Maintaining the tendon in view during this manoeuvre takes a little practice; however, if the probe falls off the tendon it is very easy to move a little medial or lateral to find it again, noting where the reflective humeral shaft drops away as the probe crosses the groove. In most individuals, the tendon travels deeper as it passes distally. This introduces an element of anisotropy, which can be easily corrected by some gentle pressure at the distal end of the probe. This manoeuvre is called ‘heel toeing’ and is used in several locations in musculoskeletal ultrasound. The long-axis image of the tendon is very useful for confirming integrity; however, as with most tendons, the internal structure is best evaluated in the axial plane.
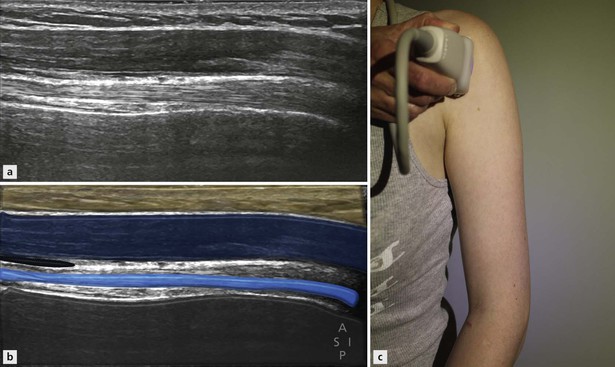
Figure 1.4 Position 2: long axis of biceps with the subacromial subdeltoid bursa just visible anterior to the superior part of the tendon.
When assessment of the long head of biceps is complete, the probe is moved medially to locate the short head of biceps. The bony margin of the coracoid process provides a very useful landmark. The short head arises from its inferior margin superficial to the insertion of the pectoralis minor and coracobrachialis tendons. The tendon of pectoralis major can be identified as a long, thin slip passing over the biceps tendon around the level of the proximal musculotendinous junction. The more detailed anatomy of the arm will be covered in a later section. The probe is then returned to the upper biceps to review the rotator interval.
Standard Position 2: Rotator Interval
Technique
As has already been mentioned, the rotator interval is the name given to the space between the subscapularis and the supraspinatus tendons through which the long head of biceps passes as it exits the glenohumeral joint. Because the tendon undergoes a 90° turn as it enters the bicipital groove, it must be supported to ensure that it does not displace medially. Two ligaments in particular combine to create this support, which is also referred to as the rotator pulley (Fig. 1.5). The two ligaments are the coracohumeral and the superior glenohumeral ligaments. The pulley is also reinforced by fibres of the subscapularis tendon passing superficially to the coracohumeral ligament and inserting on the lateral aspect of the groove. These fibres are sometimes erroneously referred to as the transverse ligament.
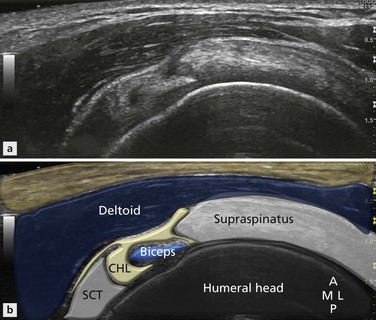
Figure 1.5 Rotator interval image. The coracohumeral ligament reinforced by the superior glenohumeral ligament separates supraspinatus from infraspinatus.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree