Silicosis, Complex
Kimberly E. Sanchez, MD
Aqeel A. Chowdhry, MD
Tan-Lucien H. Mohammed, MD, FCCP
Key Facts
Terminology
Complicated pneumoconiosis: Aggregation of nodules into large masses > 1 cm in diameter, evolves from simple pneumoconiosis
Imaging Findings
Progressive massive fibrosis
Usually bilateral in upper lobes and superior segments of lower lobes
Typically more common in dorsal aspect of lung
Right hemithorax earlier and PMF larger than left hemithorax
PMF > 4 cm nearly all contain areas of low attenuation due to central necrosis
If necrosis or cavitation is seen, mycobacterial infection should be considered
As PMF progresses, micronodules decrease in profusion
Initially develop in lung periphery and with time migrate towards hilum
PET can be markedly positive in PMF, likely due to inflammatory cell activity
Top Differential Diagnoses
Talcosis
Tuberculosis (TB)
Sarcoidosis
Pathology
Risk of lung disease related to both dose (intensity) and time (length) of exposure
Diagnostic Checklist
Rapid change in radiographic findings concerning for tuberculosis or carcinoma
TERMINOLOGY
Abbreviations and Synonyms
Complicated pneumoconiosis, progressive massive fibrosis (PMF), anthracosilicosis
Definitions
Lung disease due to inhalation of inorganic mineral dusts containing crystalline silicone dioxide (cement construction products, roof tiles, etc.)
Complicated pneumoconiosis: Aggregation of nodules into large masses > 1 cm in diameter, evolves from simple pneumoconiosis
Advanced coalescence is known as progressive massive fibrosis
IMAGING FINDINGS
General Features
Best diagnostic clue: Micronodular interstitial thickening in upper lung zones with posterior (dorsal) predominance
Patient position/location
Rounded dusts predominately affect upper lung zones
Coal dust accumulates around respiratory bronchioles (coal dust macule)
Silica accumulates along lymphatics in centriacinar lobule and lobule periphery
Size
Micronodules < 10 mm in diameter
PMF aggregation > 1 cm
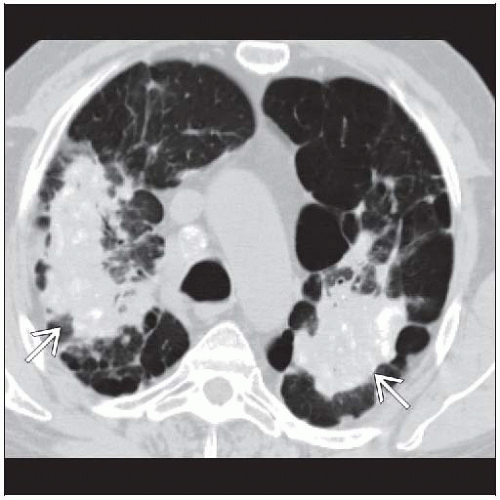
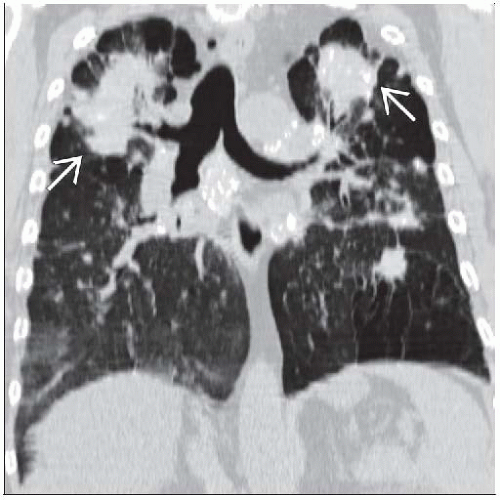
CT Findings
More sensitive in detection of nodules and confluence of small opacities
Micronodules
< 10 mm in centrilobular and subpleural distribution, follow lymphatic pathways
Distribution: More profuse in dorsal aspect of upper lobes, right side > left side
Nodules may calcify
Lymph nodes
Typically hilar and mediastinal lymph nodes enlarged
May calcify (“eggshell” classic pattern), though may be diffuse or punctate
Hilar adenopathy may develop before parenchymal disease
Progressive massive fibrosis
Aggregation into nodular clusters > 1 cm in diameter
Usually surrounded by background of small micronodules
As PMF progresses, micronodules decrease in profusion
Location
Usually bilateral in upper lobes and superior segments of lower lobes
Typically more common in dorsal aspect of lung
Right hemithorax affected 1st and size of PMF usually larger than left hemithorax
Shape
Irregular shape, often elliptical
Outer edge usually sharply defined from coexisting emphysema
Density
PMF > 4 cm, nearly all contain areas of low attenuation due to central necrosis
If necrosis or cavitation is seen, mycobacterial infection should be considered
May contain air bronchograms
May calcify diffusely
Evolution
Growth of PMF slow, typically over many years
Initially develops in lung periphery and with time migrates toward hilum
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree