3]. A physical simulator should have at least as good, or better, accuracy in positioning as the treatment unit and its mechanical tolerance must be excellent (e.g. an isocentre accuracy of 1 mm diameter sphere should be possible). The simulator geometry should permit all the required beam directions and field definitions that are achievable on a linear accelerator. Modern physical simulators (e.g. Varian Acuity™) do not have the limitations of the image intensifier systems that have been used for decades. The availability of an amorphous silicon panel to provide a digital imaging device has resulted in simulators that are almost identical to the therapy unit and have few movement constraints.
The simulator couch again needs to be identical to that used on the therapy unit and should have the same range of lateral, longitudinal, vertical and rotational movements. Coordinate scales between the simulator and linear accelerator must be identical. The ability to accommodate all treatment accessories and ensure precise emulation of the patient’s position is essential.
The size of image that can be obtained during physical simulation is limited by a number of factors: the physical size of the image detector, the focus–axis distance, the focus–detector distance and the ability to stitch images together using a merge function. Dual and Quad merge techniques allow the acquisition of an image larger than the size of the imager (which is typically 30 × 40 cm2). The enlarged image is created by moving the detector plate and acquiring multiple images all of which contain the beam central axis. Software enables these images to be referenced to this common central axis point and aligned accurately to provide extended images in both the horizontal and vertical directions. This facility is particularly useful for large pelvic fields or extended spine fields. Automatic merging of multiple images is less successful when there are significant differences in absorption within the images, e.g. a pelvis where large air gaps cause high contrast gradients.
During the localization procedure, the simulator is used much like a diagnostic x-ray unit where the patient is positioned on the couch in the treatment position and moved while imaging the anatomy. The desired location for field placement requires x-ray visualization in real-time until the required position is reached. In order to minimize radiation exposure to the patient during this procedure, a utility called ‘motion control’ is available. This function allows the control of field placement, e.g. x/y blades, collimator or field centre by adjusting these parameters on the captured (frozen/stored) image. Subsequent live activation of the imaging system initiated an automatic change to the parameter values and patient position on the physical simulator. The advantage of this function is that clinical decision and minor adjustments can be made on the captured image with a final check made with an x-ray exposure.
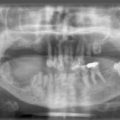
A typical head and neck physical simulation procedure is described below (although where a CT based facility is available, this offers a superior method of anatomical localization and contouring).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree