Figure 14.1 Impact of rigorous serial imaging on the legal process. A nine-month-old infant undergoing skeletal assessment because of bilateral distal humeral SH injuries and multiple lower extremity CMLs in twin sibling (see Fig. 4.33). The SS was normal. Although abuse was alleged by the child welfare agency at the emergency court hearing, the judge chose to leave the children in the home. A, AP view of the distal right femur from the initial SS shows no apparent abnormality. B, External rotation oblique view of the right knee from the two-week follow-up study reveals findings consistent with a distal femoral CML (arrows). No other injuries were found. Given this additional information, the court ordered foster placement of both children. C, Oblique view of the right femur two weeks later shows evidence of union of the fragment (arrows).
Global skeletal assessment
Background
Caffey advised routine views of the long bones when he drew attention to the skeletal injuries associated with subdural hematomas (SDHs) in 1946 (1). However, there was wide variation in the approach to skeletal imaging for suspected child abuse for most of the twentieth century. Little attention was given to technical factors, the regions encompassed by the survey, and the specific views employed in these assessments. In particular, there were no recommendations for systematic rigorous imaging of the spine, hands, and feet (2–6). At most, authors recommended that the hands and feet be included on full views of the extremities but lateral views of the entire spine were not specified (6).
The babygram, an effort to image the infant and small child on one or two radiographic exposures, was commonplace thorough the latter half of the twentieth century, and stood in stark contrast to customary efforts to improve the technical rigor of radiographic studies performed of specific anatomic regions for indications such as accidental trauma, infection, and neoplasia (Fig. 14.2).
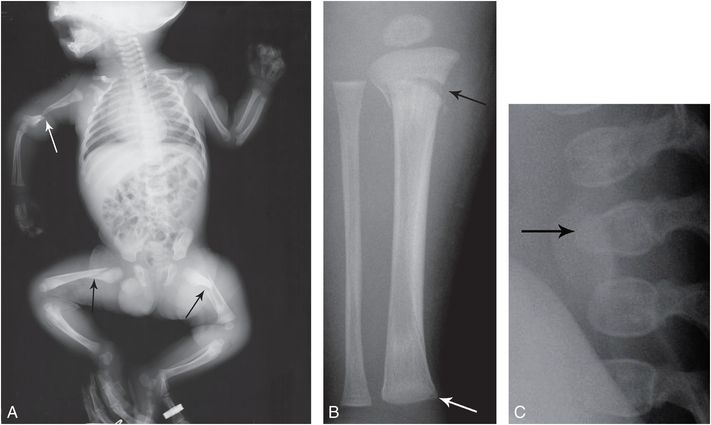
Figure 14.2 “Babygram.” A six-week-old infant not moving right leg. Radiographs done elsewhere revealed a right femur fracture, and a “babygram” was performed. A, This crude assessment reveals several gross shaft fractures (arrows). However, it fails to define a right proximal tibial metaphyseal fracture (black arrow), a distal tibial CML (white arrow) evident on the AP view of the right lower leg (B), and an L2 vertebral body compression fracture (arrow) visible on the lateral view of the lumbar spine (C) from the subsequent SS.
Consequently, delineating the full spectrum of inflicted injuries was hampered by the limited quality of imaging data, and this had a clear impact on the level of radiographic assessment in cases of suspected abuse.
In 1991 the Section on Radiology of the American Academy of Pediatrics (AAP) published a statement detailing the skeletal imaging recommendations for suspected abuse, and in 1997 the American College of Radiology (ACR) published formal standards for skeletal surveys (SSs) (7, 8). The recommendations acknowledged that the SS is “frequently critical to diagnosis and is often presented as evidence in care and protection cases, criminal proceedings and other types of litigation” (7). Compliance with these recommendations in the United States has been variable, but it has become customary to separately image the hands and feet, and to include lateral views of the spine in SSs for suspected abuse (9). A 2003 report by Offiah and Hall found that the compliance with the published standards in England is less encouraging (10). Despite the wide variations in how, when, and in whom these studies are performed, the literature provides strong support for global screening in infants and young children with suspected abuse (10–23).
Scintigraphy has also been employed for many years for global skeletal assessment, and it remains an important tool in this context (16). There has been renewed interest in this modality with the availability of 18F-NaF positron emission tomography (PET) skeletal imaging in some centers (24). Whole-body magnetic resonance imaging (WB-MRI) has gained popularity for global screening for osseous neoplasia, and some centers have explored its utility in the context of child abuse (25). Whole-body computed tomography (CT) has been used in the context of postmortem imaging, but there are few data to justify its use as a screening technique in living children (26).
Modalities
Skeletal survey
Technical principles
The general technical principles governing the radiographic SS include the use of a high-detail imaging system and tightly collimated views of each anatomic region of the entire skeleton (21). A detailed discussion of the technical aspects of the SS is presented in Chapter 30. A principle implicit in general radiographic imaging of the extremities is that frontal and lateral projections are required to achieve optimal detection of subtle injuries. Since the standard survey protocol prescribes only frontal view of each region of the extremities, this approach will miss fractures (Fig. 14.3), and the inclusion of lateral views of the extremities will significantly increase the number of fractures detected on this study (27). This increased yield must be weighed against the addition of at least eight more views to the standard protocol. At a minimum, additional views of the extremities should be obtained on the basis of the clinical findings and any abnormalities identified or suspected on the initial images. Oblique views are particularly useful in the assessment of the classic metaphyseal lesion (CML) (see Fig. 14.1). On occasion, a modest suspicion of fracture on the frontal view, based on an asymmetric appearance with the contralateral side, may require multiple exposures until an optimal view elucidates the finding (Fig. 14.4). Anteroposterior (AP) and lateral views of the thorax are acquired and the sternum should be included on the lateral projection. The addition of right and left posterior oblique views of the thorax increases the yield of rib fractures (see Chapter 5), and they have been incorporated into the current recommended survey protocols (17, 20, 21, 28, 29). It should be noted that when rib fractures are visible on the oblique view, there is usually some evidence of rib fracture on the AP projection (30). Tightly collimated views of particular rib regions may document fractures which are equivocal with the standard field of view.
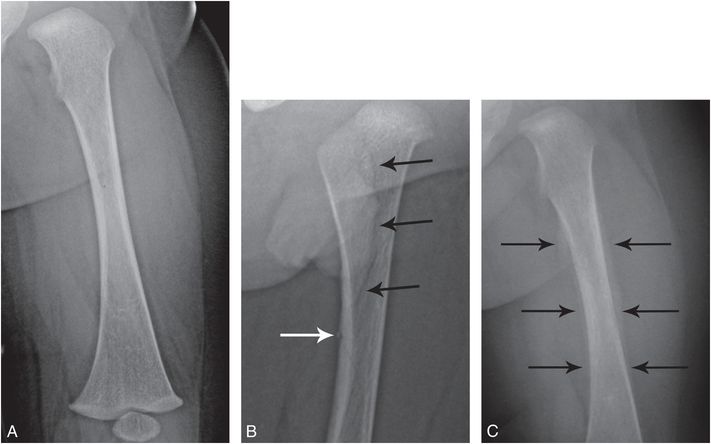
Figure 14.3 Femoral fracture only evident on the lateral projection. A six-month-old infant who reportedly became fussy and stopped using the left lower extremity, with pain on left leg movement. Radiographs done elsewhere reportedly revealed a left femoral shaft fracture. A, AP view of the left femur from the SS shows no abnormality. B, Because of the earlier findings, a lateral view was obtained revealing a subtle nondisplaced oblique femoral shaft fracture (black arrows) with subtle posterior cortical disruption (white arrow). C, AP view two weeks later shows extensive SPNBF, but still no fracture line.
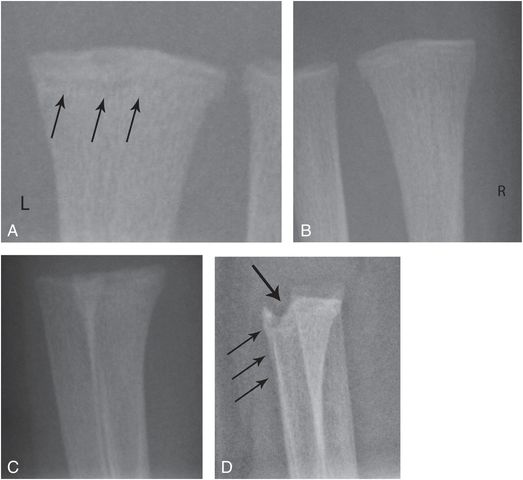
Figure 14.4 Subtle CML, heavily dependent on technique. A 23-day-old infant not moving left leg. Radiographs revealed a CML of the left proximal tibia. SS demonstrated multiple additional CMLs at the knees. A, B, Cropped AP views of the distal forearms show vague sclerosis and lucency in the left distal radial metaphysis (arrows) when compared with the right. C, First attempt at a lateral projection of the left side shows no definite abnormality. D, A second lateral view with slight rotation to project the ulna ventrally shows a healing distal radial CML (thick arrow) with SPNBF (thin arrows).
It is the author’s view that the hands should be viewed in the oblique projection, since subtle buckle fractures may not be evident on the frontal projection (see Chapter 4) (31). Inclusion of the hands on a view of the arm/forearm provides suboptimal detail and may miss these important injuries. Additional views tightly collimated to individual digits are often helpful to characterize findings suspected on the initial images.
Since most spinal injuries are detected on the lateral projection, well-collimated lateral views of the cervical, thoracic, and lumbosacral spine are critical (see Chapter 21) (32). Although these vertebral body compression fractures are usually clinically silent, they carry a significant association with intracranial injuries. They may also be the only unsuspected skeletal injury detected on the survey (32). Several publications have suggested that views of the spine, hands, and feet can be eliminated from the survey protocol (33, 34), but others have reinforced the need to encompass the entire skeleton on the initial survey (30, 32, 35, 36). Although these studies found that the overall prevalence of injuries of the hands and feet or spine is less than 3%, the combined prevalence of fractures in these regions in some studies is as high as 20% when only positive SSs are considered (30).
When a skull fracture is suspected, the customary frontal and the single lateral examination should be supplemented with the opposite lateral projection and a Towne’s view. Experience suggests that three-dimensional (3D) models generated from cranial CT may be able to supplant radiography in some cases (see Chapter 17), but currently views of the skull are still advisable in the standard survey protocol.
Follow-up SS
A follow-up SS is widely accepted when concerning fractures are evident on the initial study, or when the survey is normal and there are persistent suspicions of abuse based on clinical or other imaging grounds. A follow-up SS can: (1) confirm suspected fractures; (2) detect additional fractures; (3) differentiate fractures from normal developmental variants; and (4) date injuries.
Silverman and Kuhn noted the value of repeat radiographs in the detection of metaphyseal injuries in abused children (37). Kleinman and colleagues studied 23 infants and toddlers strongly suspected of being physically abused who underwent a follow-up SS excluding the skull 2 weeks after the initial examination (38). A follow-up study yielded additional information regarding skeletal injury in 61% of cases. The number of fractures detected increased from 70 to 89 (27%) (P = 0.005). Most of these additional injuries were CMLs or rib fractures. In 13 of the 70 fractures previously detected, the follow-up SS provided important additional information about the age of those injuries. Bennett and others studied 57 children less than 2 years of age who had an initial negative SS. Four children had signs of healing bone trauma on a follow-up survey. Three of these children (75%) had healing rib fractures and one child had a healing proximal humeral fracture. The authors concluded that even if the initial SS is normal, a follow-up examination can yield forensically important findings on follow-up SS and may increase the certainty of a diagnosis of abuse. The value of this imaging approach has been confirmed by others (30, 39–45).
Some authors have explored the possibility of an abbreviated follow-up SS (42, 43). Harlan and others studied 101 children ranging in age from 0 to 36 months (42). Eighty-five were less than 1 year of age, 12 (11.9%) were aged 12–24 months, and 3 (3%) were aged 25–36 months. All cases had the initial ACR standardized examination and a similar follow-up study that excluded the skull. A total of 244 fractures were identified in the 101 children on the initial SS. Follow-up surveys demonstrated new information in 38 children (37.6%). The authors found that a follow-up protocol that excluded the lateral views of the spine and the AP view of the pelvis missed no injuries that were unsuspected on the initial study. A multicenter study supports Harlan’s findings, and it is reasonable to conclude that this approach can result in decreased radiation burden without the loss of diagnostic information (46). Such an approach is predicated on the application of rigorous technique and careful radiologist scrutiny for all image acquisitions (see Chapter 30).
There are data that suggest that the follow-up study is underutilized in some centers. Singh et al. studied 1470 children who underwent an initial SS and found that only 11% also had a follow-up exam (44). Of these studies, 14% (24/169) revealed previously unrecognized fractures; all of which were healing. There were 8 children in whom the information obtained from the follow-up SS resulted in a diagnosis of definite physical abuse; all 8 children were younger than 12 months, and in 6 of these cases the initial SS did not demonstrate any fractures. The authors suggested that because of the high morbidity and mortality of unrecognized/missed abuse in infants, a follow-up SS should be a routine part of the evaluation in this age group.
Although the precise optimal interval between the initial and follow-up exams has not been established, based on customary patterns of healing, a repeat study at two weeks is advised. In some situations practical issues may require a slight modification in this timetable. If a young infant is to be discharged from an inpatient setting, and a study at 2 weeks is problematic, a minimum interval of 10 days may be a reasonable compromise. In the infant who has been placed in a cast or harness for a fracture, a three-week interval may be acceptable in order to permit safe removal of the immobilization device.
Skeletal scintigraphy
In the early child abuse literature, the diagnosis of skeletal injury relied entirely on radiography. With advancements in the development of radiopharmaceuticals, in particular the family of bone avid polyphosphate compounds, skeletal scintigraphy has assumed an important role in cases of suspected child abuse. Skeletal scintigraphy in pediatrics, particularly in infants, is technically demanding and requires collimation and other instrumentation suitable for small children (see Chapter 28) (47, 48). In the hands of technologists and radiologists/nuclear medicine physicians with strong training and experience with pediatric patients, scintigraphy is a valuable technique for assessing inflicted skeletal injury (24, 49, 50).
Many examples of skeletal injury demonstrated with bone scans are illustrated in this text. Skeletal scintigraphy can also reveal abnormal extraskeletal accumulations of radionuclide that may provide evidence regarding inflicted soft tissue/visceral injury (see Figs. 22.35, 22.38) (51, 52). The advantages and disadvantages of scintigraphy in the evaluation of suspected abuse, and its complementary role with regard to skeletal radiography, are addressed below.
Radiographic SS versus skeletal scintigraphy
Nearly all the nuclear medicine studies in the literature focus on the use of 99mTc methylene diphosphonate (MDP) or related compounds for imaging suspected abuse. Studies comparing the relative utility of these examinations in cases of suspected abuse are limited and are often hindered by small numbers of patients, variations in imaging protocols, different degrees of technologist and interpreter expertise, and investigator bias. Several studies have assessed the value of radiography vs. scintigraphy as a primary diagnostic tool for suspected child abuse (49, 53–57). Radiologists from the Children’s Hospital of Milwaukee studied 261 infants and children suspected of being abused who underwent radiographic SSs and skeletal scintigraphy (49). The bone scans were performed with meticulous attention to technique and converging collimators in small infants. Sedation was required in uncooperative patients. Complete radiographic SSs were obtained, including frontal and lateral views of the thoracolumbar spine. Details of the precise filming protocol and the spatial resolution of the radiographic imaging systems were not provided. The skull was not evaluated scintigraphically in this study. Of the 261 children examined by both techniques, 120 demonstrated scintigraphic abnormalities at one or more sites and 105 demonstrated one or more radiographic abnormalities. Radiography yielded false-negative results in 32 patients; scintigraphy yielded 2 false-negative studies. Although no “gold standard” could be applied to the cases in which abnormalities were apparent only on scintigraphy, the study suggests a superior sensitivity of scintigraphy over radiography under the conditions described by the authors.
Other studies have shown higher percentages of false-negative bone scans (2, 54, 55). In a multicenter study Merten and colleagues reviewed the radiographic findings in 563 abused infants and children (2). In the limited number of patients undergoing both scintigraphy and SSs, a false-negative rate of 27% with scintigraphy was encountered. The studies of Sty and Starshak (49) and Merten and colleagues (2) prompted a useful exchange of views in the editorial section of the journal Radiology (58–62).
In 1993, Conway and associates described their experience with 61 cases of suspected abuse that underwent both bone scintigraphy and radiographic SS (63). No specific information regarding the technique and imaging systems employed for the radiographic SS was provided. Nearly all patients were under three years of age, and most were infants. Bone scintigraphy detected 26 abnormalities not noted on SS in 11 patients. Fifteen of these additional abnormalities noted scintigraphically were rib fractures. In 7 patients, 13 abnormalities were detected on SS that had been missed on bone scintigraphy; of these, 6 were skull fractures. Inter-reader agreement was 68.6% with scintigraphy and 80% with SS. Most importantly, disagreements between modalities, as well as between readers, were most frequent in children under 18 months of age. The authors concluded that “radionuclide scintigraphy is a complementary rather than competitive imaging modality to x-ray evaluation in the diagnosis and management of physical child abuse” (63).
In 2003 Mandelstam and others reached a similar conclusion. The authors studied 32 children that had undergone both SS and 99mTc medronate bone scintigraphy within a 48-hour period (50); 24 of 32 (75%) were under 12 months old and 30 of 32 (94%) were less than 3 years of age. Both examinations followed rigid departmental protocols that remained identical throughout the study period. The total number of bony injuries identified was 124 in 30 children; 64 were identified on bone scan and 77 on SS. Rib fractures represented 60 of 124 (48%) of the bony injuries and were present in 16 of 30 children (53%); 62.5% had multiple rib fractures. When rib fractures were excluded, there were 64 (52%) bony injuries, of which 33% were seen on both imaging modalities, 44% were seen on SS only, and 25% were seen on bone scans alone. Metaphyseal lesions characteristic of child abuse were present in 20 cases (31%) on SS, and only 35% of these were identified on bone scan. There were 6 children (20%) with normal SSs who had abnormalities on bone scan. There were 3 children (10%) with normal bone scans who had injuries demonstrated radiographically. Because of the demonstrated complementary nature of the two modalities, the authors recommended that both examinations be performed in cases of suspected child abuse.
Drubach et al. explored the use of 18F-NaF PET in the context of suspected child abuse (24). Introduced in 1962, 18F-NaF is a positron-emitting, bone-seeking imaging agent, which was approved as a bone imaging agent by the US Food and Drug Administration in 1972 (64). Until recently, the modest availability of PET imaging infrastructure limited the clinical use of this agent, but the emergence of this technology and the availability of the radionuclide compound have created new applications for 18F-NaF PET imaging. The higher target-to-background ratio, better image contrast, and superior spatial resolution of 18F-NaF PET make this an attractive 3D alternative to planar 99mTc-based imaging.
Drubach et al. reviewed the SS and PET images obtained in 22 patients under 2 years of age (24). A total of 156 fractures were detected at baseline SS, and 200 fractures were detected with PET. When compared with the reference standard (findings in the 14 patients who underwent baseline and follow-up SS), PET had sensitivities of 85% for the detection of all fractures, 92% for the detection of thoracic fractures (ribs, sternum, clavicle, and scapula), 93% for the detection of posterior rib fractures, and 67% for the detection of CMLs. Compared with the reference standard, baseline SS had sensitivities of 72% for the detection of all fractures, 68% for the detection of thoracic fractures, 73% for the detection of posterior rib fractures, and 80% for the detection of CMLs. The authors concluded that 18F-NaF PET had greater sensitivity in the overall detection of fractures related to child abuse than did baseline SS and was superior in the detection of rib fractures in particular.
On the basis of these communications and other relevant sources, the relative merits of these two modalities can be assessed (Table 14.1).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








