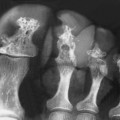
• Normal tendons and ligaments are devoid of signal on all routine pulse sequences • Tendinitis: this leads to tendon enlargement and increased intratendinous signal intensity High-resolution transducers are ideal for assessing tendon, ligament and muscle injuries • Normal tendons appear as hyperechoic parallel lines within the longitudinal plane • Tendinitis: this is seen as an increased tendon thickness with altered echogenicity (focal or diffuse) • Tear: this appears as a hypoechoic gap within the tendon (often fluid is seen within the tendon sheath) • Pathological fracture: this occurs where substantially less force is required to cause a fracture in a weakened bone • Stress fracture (fatigue fracture): this occurs due to chronic repetitive trauma on normal bone • Insufficiency fracture: this is caused by normal activity on abnormal bone (e.g. osteopenic bone in the elderly) • Joint prosthetic loosening: a widened radiolucency at either the bone–cement or prosthesis–bone interface (> 2mm) • Location: e.g. proximal, middle or distal shaft • An open (disruption of the overlying skin, suggested by gas within the adjacent soft tissues) vs a closed fracture (with intact overlying skin) • A complete (a fracture extending across the full width of the bone) vs an incomplete fracture (e.g. a paediatric greenstick fracture) • A transverse vs an oblique vs a spiral (due to significant torsional force) fracture • Distraction (separation) vs impaction vs overriding (overlapping without impaction) of the fracture fragments • Joint dislocation (the articular surfaces are completely separated) vs subluxation (there is partial contact between the articular surfaces) • An avulsion fracture: there is separation of the bone fragment at the ligament or tendinous attachment site (it is usually a transverse fracture) • An osteochondral fracture: there is disruption of the articular cartilage and underlying subchondral bone • Comminuted fracture: > 2 separate bone fragments • Butterfly fragment: a large triangular fragment usually orientated along the long axis of the bone • The proximal fragment is considered the point of reference when describing the displacement of a distal fragment: • Associated soft tissue injuries: • The cervical spine is normally lordotic – this may be absent due to patient positioning, the presence of a hard collar or muscular spasm • All seven cervical vertebrae (including the C7–T1 junction) must be visualized • Four imaginary continuous curves should be present: (1) anterior vertebral body line, (2) posterior vertebral body line, (3) spinolaminar line and (4) posterior spinous process line • A perfectly positioned lateral view: the right and left facet joints are superimposed (otherwise the facet joints partially overlap) • The odontoid process is usually tilted posteriorly on the body of C2 – however this may otherwise indicate an odontoid fracture • The atlantoaxial distance measured at the base of the dens between the anterior cortex of the dens and posterior cortex of the anterior arch of C1: • Assessment of the prevertebral tissues (to exclude a retropharyngeal haematoma): • The cervical spine is divided into 3 columns: • Instability is suggested if there is: abnormal spinous process fanning • Instability is more likely if more than one column is disrupted • Fractures and dislocations are most common within the lower cervical spine (C4–C7) • Paraspinal haematomas (e.g. a retropharyngeal mass) may point to an otherwise obscure fracture or dislocation • The oblique superior articulating surfaces of the lateral masses of the atlas are driven down and laterally – this disrupts the anterior and posterior arches of the atlas (there can be a single disruption of each arch) • Bilateral fractures of the neural arch anterior to the inferior facets (traumatic spondylolysis of the axis) • It is often associated with dislocation of C2 on C3 (there may be an associated avulsion fracture of the anteroinferior C2 margin) • Any neurological deficit is often less severe than anticipated (as the normal cervical cord occupies only up to 50% of the spinal canal AP diameter and bilateral isthmus fractures can produce canal decompression) • This can be mistaken for an os odontoideum (either congenital or post traumatic) • Type 1 (high): an avulsion fracture of the superolateral portion of the tip of the dens by the intact alar ligament – STABLE injury • Type 2 (high): a transverse fracture at the base of the dens (the commonest type) – UNSTABLE injury • Type 3 (low): a fracture of the superior portion of the axis body with extension through one or both of its superior articular facets (it is not technically a dens fracture) – UNSTABLE injury • A fracture of the anteroinferior corner of body of C2 (which is avulsed by an intact anterior longitudinal ligament) • It may occur in isolation or be associated with a hangman’s fracture • Dislocation of the interfacetal joint on the side opposite to the direction of rotation (the dislocated facet comes to rest anterior to the subjacent facet and is thus ‘locked’) • Compression of a vertebral body between adjacent vertebral bodies • Anterior wedged vertebral body deformity and vertebral end-plate depression (which is usually superior) • Decreased anterior vertebral body height (the anterior cortical margin may be disrupted, angulated or impacted) • Lumbar spine: a fracture is usually limited to the superior end plate and subjacent vertebral body • Paraspinous haematoma: a localized lateral bulge of the mediastinal stripe • A non-united vertebral ring epiphysis • This is common at the thoracolumbar junction (resulting from an axial compression force) • Unlike a simple compression fracture the vertebral body posterior cortex is disrupted • STABLE injury (it may become an UNSTABLE injury if there is a neurological deficit or retropulsed fragments) • This most commonly occurs at the T10–L2 level (at the junction of mobile and relatively immobile segments) • Mechanism: it is due to a combination of shearing, rotation and flexion forces Wide separation of the spinous processes • There may be a disrupted intervertebral disc, facet joint or interspinous ligament without an associated fracture • Vertebral body above the injury level: anterior dislocation • Vertebral body below the injury level: an anterior wedge compression fracture with a triangular bony fragment avulsed from its anterosuperior surface • Horizontal splitting of the vertebral body with little compression (a ‘seatbelt’ fracture) • It is commonly associated with intra-abdominal and neurological injuries • Mechanism: anterior hyperflexion over an object (e.g. a seatbelt) that serves as a fulcrum A horizontal fracture involving the spinous processes, laminae, articular masses and vertebral body • The vertebral body is tilted (with a widened interspinous space) at the injury site with little anterior wedging • There may be disruption of the ligaments and intervertebral discs without an associated fracture • Fractures tend to be spiral (they can also be angulated and overriding due to muscular contraction on the individual fragments) • They are most commonly seen in the elderly • Tears affecting the anterosuperior labrum, with biceps tendon involvement • SLAP: Superior Labrum from Anterior to Posterior (in relation to the biceps tendon insertion) • There is a restrictive space between the acromion, coracoacromial arch and acromioclavicular joint (superiorly) and the humeral head and greater tuberosity (inferiorly) • There is potential ‘pinching’ of the distal centimetre of the supraspinatus tendon (representing a vascular watershed region) between the coracoacromial arch and humeral head on abduction and external rotation
Skeletal trauma
INTRODUCTION
GENERAL CONSIDERATIONS
MRI
 sprains and tears increase their water content (T2WI: high SI)
sprains and tears increase their water content (T2WI: high SI)  fat-suppressed sequences increase the conspicuity of any increased signal
fat-suppressed sequences increase the conspicuity of any increased signal
 Partial tear: this may be seen as an irregularity within the tendon shape with associated high SI (T2WI)
Partial tear: this may be seen as an irregularity within the tendon shape with associated high SI (T2WI)
 Complete tear: the tendon is discontinuous, absent or unrecognizable
Complete tear: the tendon is discontinuous, absent or unrecognizable
US
 artefactual areas of hypoechogenicity may result from incorrect transducer placement
artefactual areas of hypoechogenicity may result from incorrect transducer placement
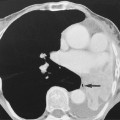
 ‘Banana fracture’: pathological fractures tend to be oriented transversely within long bones
‘Banana fracture’: pathological fractures tend to be oriented transversely within long bones
 Causes: metastatic disease
Causes: metastatic disease  benign tumours (e.g. an enchondroma or a solitary bone cyst)
benign tumours (e.g. an enchondroma or a solitary bone cyst)  Paget’s disease
Paget’s disease  renal osteodystrophy
renal osteodystrophy  osteogenesis imperfecta
osteogenesis imperfecta
 a subtle periosteal reaction or a transverse band of linear sclerosis may develop 1–2 weeks after the onset of symptoms
a subtle periosteal reaction or a transverse band of linear sclerosis may develop 1–2 weeks after the onset of symptoms
 Common sites: metatarsal shafts (‘march fractures’)
Common sites: metatarsal shafts (‘march fractures’)  pubic rami
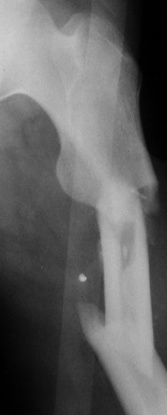
pubic rami  femoral neck
femoral neck  tibial and fibular shafts
tibial and fibular shafts  calcaneal tuberosity
calcaneal tuberosity
 prosthetic migration
prosthetic migration  periosteal reaction
periosteal reaction
FRACTURE DESCRIPTION
 a fracture fragment can become a joint loose body
a fracture fragment can become a joint loose body
 Anterior, posterior, medial or lateral (e.g. one shaft width medial displacement)
Anterior, posterior, medial or lateral (e.g. one shaft width medial displacement)
 Angulation of the long axis of the distal fragment relative to the proximal fragment (varus vs valgus)
Angulation of the long axis of the distal fragment relative to the proximal fragment (varus vs valgus)
ASSESSMENT OF CERVICAL SPINE INJURIES
ASSESSMENT OF CERVICAL SPINE INJURIES
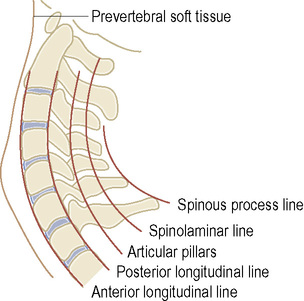
NORMAL RADIOLOGICAL ANATOMY (LATERAL XR)
 this may require a swimmer’s view if they are not demonstrated on the lateral view
this may require a swimmer’s view if they are not demonstrated on the lateral view
 NB: in children, the spinolaminar line may have an offset of 2 to 3mm at the C2–C3 and C3–C4 levels with flexion and extension
NB: in children, the spinolaminar line may have an offset of 2 to 3mm at the C2–C3 and C3–C4 levels with flexion and extension
 any facet joint overlap should be uniform at all levels – an abrupt change in the amount of overlap within adjacent levels indicates abnormal rotation along the longitudinal axis of the spine
any facet joint overlap should be uniform at all levels – an abrupt change in the amount of overlap within adjacent levels indicates abnormal rotation along the longitudinal axis of the spine
 The articular surfaces of each facet must be congruent – this may otherwise indicate a subluxed or dislocated facet
The articular surfaces of each facet must be congruent – this may otherwise indicate a subluxed or dislocated facet
RADIOGRAPHIC SIGNS OF INSTABILITY
 Anterior column: the anterior longitudinal ligament and the anterior ½ of the vertebral body
Anterior column: the anterior longitudinal ligament and the anterior ½ of the vertebral body
 Middle column: the posterior ½ of the vertebral body and the posterior longitudinal ligament
Middle column: the posterior ½ of the vertebral body and the posterior longitudinal ligament
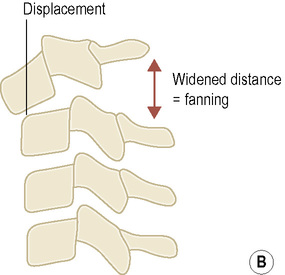
 a widened disc space
a widened disc space  horizontal displacement of one body on another (> 3.5mm)
horizontal displacement of one body on another (> 3.5mm)  angulation > 11º
angulation > 11º  disrupted facets or multiple fractures
disrupted facets or multiple fractures
PEARLS
 Usually the upper vertebral body is displaced anteriorly relative to the lower vertebral body
Usually the upper vertebral body is displaced anteriorly relative to the lower vertebral body
 There is often an anterior wedge compression fracture of the lower vertebral body and fractures involving the laminae, facets, or spinous processes
There is often an anterior wedge compression fracture of the lower vertebral body and fractures involving the laminae, facets, or spinous processes
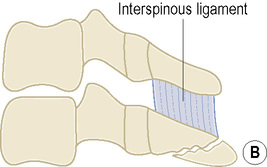
 Alternatively, there may be disruption of the joint capsule of the facet joints and interspinous ligament without associated fractures
Alternatively, there may be disruption of the joint capsule of the facet joints and interspinous ligament without associated fractures
 At times there may be no significant fracture associated with a dislocation, since the injury is limited to the intervertebral disc, facet joint capsules and intervening ligaments
At times there may be no significant fracture associated with a dislocation, since the injury is limited to the intervertebral disc, facet joint capsules and intervening ligaments
SPINAL INJURIES
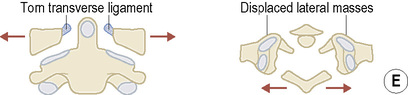
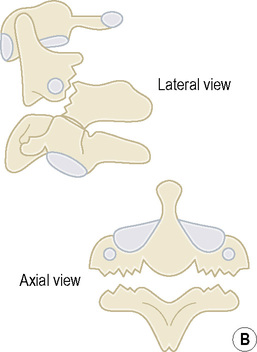
JEFFERSON FRACTURE (C1)
DEFINITION
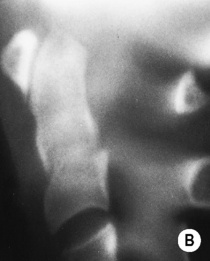
HANGMAN’S FRACTURE (C2)
DEFINITION
 the fracture lines tend to be oblique and symmetrical
the fracture lines tend to be oblique and symmetrical
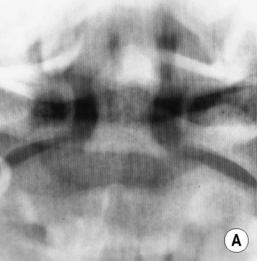
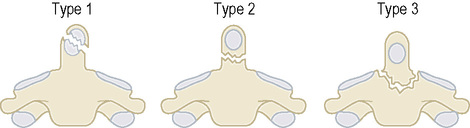
ODONTOID (DENS) FRACTURE (C2)
DEFINITION
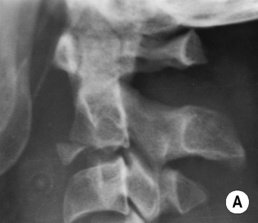
EXTENSION TEARDROP FRACTURE (C2)
DEFINITION
 it is not associated with a neurological deficit
it is not associated with a neurological deficit
 it may occasionally involve the lower cervical vertebral bodies
it may occasionally involve the lower cervical vertebral bodies
UNILATERAL LOCKED FACETS/UNLATERAL INTERFACETAL DISLOCATION (C3–C7)
DEFINITION
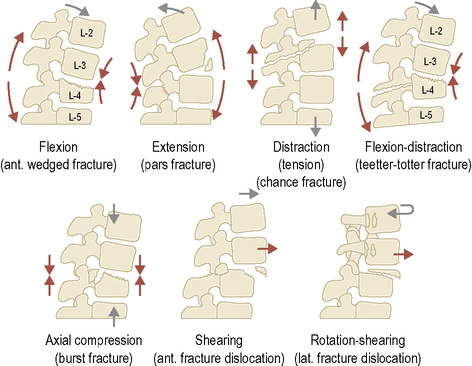
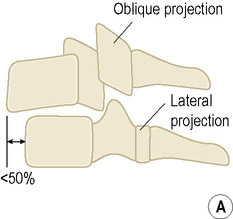
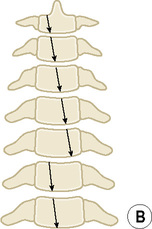
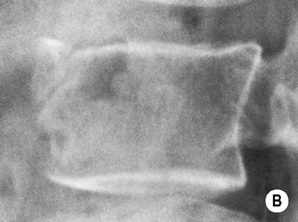
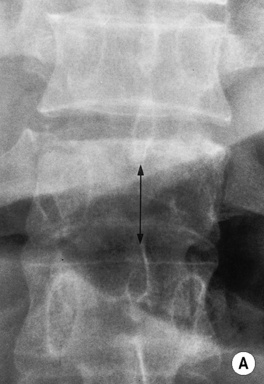
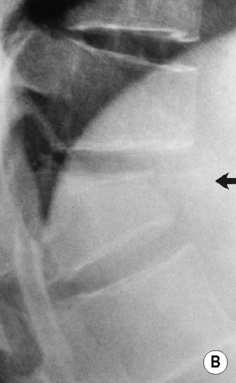
SIMPLE WEDGE (COMPRESSION) FRACTURE (T1–L5)
DEFINITION
 it is associated with a paraspinous haematoma
it is associated with a paraspinous haematoma
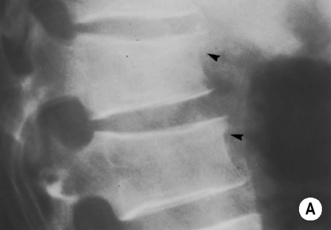
RADIOLOGICAL FEATURES
XR
 impaction is identified by a faint sclerotic band just beneath the deformed end-plate
impaction is identified by a faint sclerotic band just beneath the deformed end-plate
 the posterior height is maintained (as the posterior elements remain intact)
the posterior height is maintained (as the posterior elements remain intact)
PEARLS
Lesions that may mimic a compression fracture
 Schmorl’s nodes (an irregular lucent defect at the end-plate with irregular sclerotic margins)
Schmorl’s nodes (an irregular lucent defect at the end-plate with irregular sclerotic margins)  a limbus vertebra (a distant separate ossicle found on the anterosuperior margin of the vertebral body and representing a developmental abnormality of the ring apophysis)
a limbus vertebra (a distant separate ossicle found on the anterosuperior margin of the vertebral body and representing a developmental abnormality of the ring apophysis)
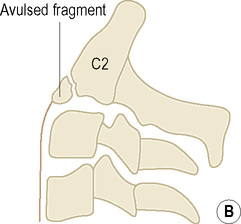
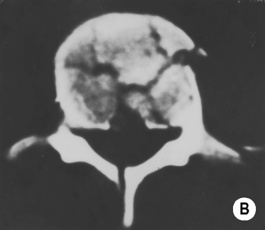
Burst fracture
 a fragment from the superoposterior vertebral body may be displaced into the spinal canal with the potential for neurological injury
a fragment from the superoposterior vertebral body may be displaced into the spinal canal with the potential for neurological injury
FRACTURE–DISLOCATION (T10–L2)
DEFINITION
 neurological injury is common
neurological injury is common
 Stable: limited to a vertebral body or the posterior elements only
Stable: limited to a vertebral body or the posterior elements only
 Unstable: involving both the vertebral bodies and the posterior elements
Unstable: involving both the vertebral bodies and the posterior elements
RADIOLOGICAL FEATURES
AP XR
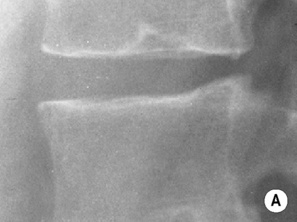
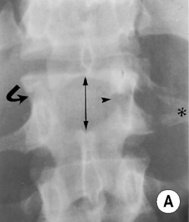
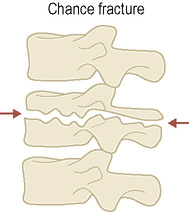
CHANCE FRACTURE (L1–L5)
DEFINITION
RADIOLOGICAL FEATURES
Lateral XR
SHOULDER INJURIES
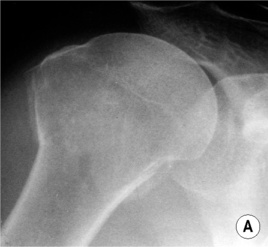
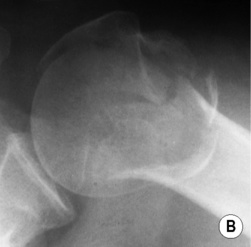
ANTERIOR SHOULDER DISLOCATION
DEFINITION
PROXIMAL HUMERAL FRACTURES
DEFINITION
 they usually involve the surgical neck and are associated with separation of the greater tuberosity
they usually involve the surgical neck and are associated with separation of the greater tuberosity
1 part
There is no displacement of the fracture fragments
2 part
There is displacement of 1 fragment
3 part
There is displacement of 2 fragments (1 tuberosity remains in contact)
4 part
There is displacement of 3 fragments
SLAP LESIONS
DEFINITION
SHOULDER IMPINGEMENT SYNDROME/ROTATOR CUFF TEARS
ANATOMY
 the rotator cuff tendons (supraspinatus, infraspinatus, teres minor and subscapularis) pass through this space
the rotator cuff tendons (supraspinatus, infraspinatus, teres minor and subscapularis) pass through this space
MECHANISM
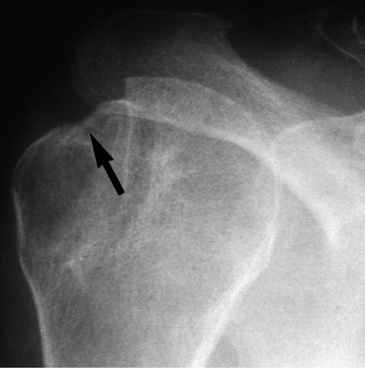
 variations in the shape of the anteroinferior acromion, together with osteoarthritic change, can exacerbate any impingement
variations in the shape of the anteroinferior acromion, together with osteoarthritic change, can exacerbate any impingement

 it is poor at soft tissue assessment
it is poor at soft tissue assessment a lipohaemarthrosis (fat and blood within the joint space) is evidence of an intra-articular fracture
a lipohaemarthrosis (fat and blood within the joint space) is evidence of an intra-articular fracture it is much more sensitive than XR
it is much more sensitive than XR it is very sensitive for the detection of bone oedema (T1WI: low SI
it is very sensitive for the detection of bone oedema (T1WI: low SI  T2WI: high SI)
T2WI: high SI)



 patella
patella  talar dome
talar dome

 this can be seen on a horizontal lateral view of the knee
this can be seen on a horizontal lateral view of the knee  it can also be seen within the shoulder
it can also be seen within the shoulder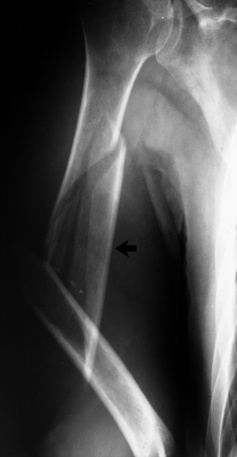









 < 22mm (at the level of C6)
< 22mm (at the level of C6)
 < 14mm (at the level of C6)
< 14mm (at the level of C6)









 it is an uncommon injury
it is an uncommon injury
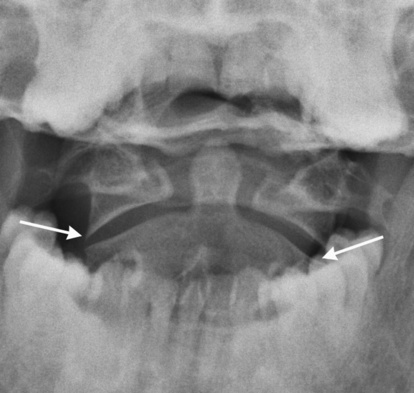
 a widened space between the dens and medial border of the C1 lateral masses
a widened space between the dens and medial border of the C1 lateral masses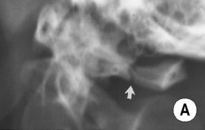
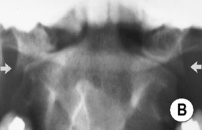

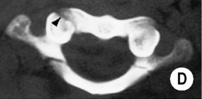
 take care with differentiating it from neural arch gaps that are normal variations
take care with differentiating it from neural arch gaps that are normal variations





 prevertebral soft tissue swelling
prevertebral soft tissue swelling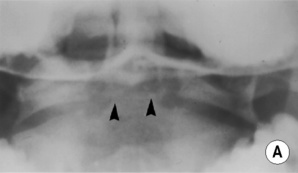



 the anterior vertebral body height is reduced with associated prevertebral soft tissue swelling
the anterior vertebral body height is reduced with associated prevertebral soft tissue swelling

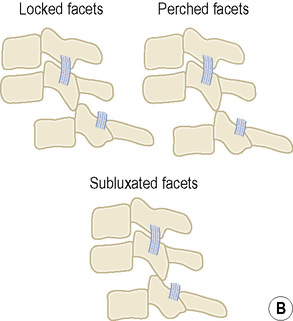
 the spine above the level of dislocation is obliquely oriented (the spine below is in direct lateral orientation)
the spine above the level of dislocation is obliquely oriented (the spine below is in direct lateral orientation)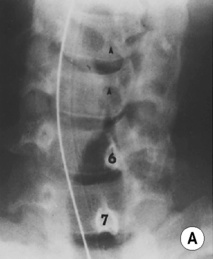
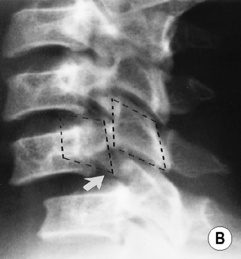

 the articular masses of the superior vertebrae lie anterior to the articular masses of inferior vertebrae (thus ‘locking’ the facets)
the articular masses of the superior vertebrae lie anterior to the articular masses of inferior vertebrae (thus ‘locking’ the facets)  there are often associated
there are often associated

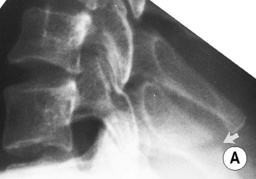

 widening of the interspinous and interlaminar space (‘fanning’)
widening of the interspinous and interlaminar space (‘fanning’)  interfacetal joint subluxation
interfacetal joint subluxation  posterior widening and anterior narrowing of the intervertebral disc (± 1–3mm of vertebral anterior displacement)
posterior widening and anterior narrowing of the intervertebral disc (± 1–3mm of vertebral anterior displacement) the injury is associated with delayed instability
the injury is associated with delayed instability

 it is associated with an avulsion fracture of the greater tuberosity
it is associated with an avulsion fracture of the greater tuberosity there is an increased risk for recurrent dislocations
there is an increased risk for recurrent dislocations there is an increased risk for recurrent dislocations
there is an increased risk for recurrent dislocations it is due to a large haemarthrosis
it is due to a large haemarthrosis the humeral head impinges upon the acromion, which acts as a fulcrum
the humeral head impinges upon the acromion, which acts as a fulcrum  the arm is ‘locked’ in abduction
the arm is ‘locked’ in abduction it accounts for 5% of all shoulder dislocations
it accounts for 5% of all shoulder dislocations there is subtle widening of the joint (> 6mm) or the bones overlap on a Grashey view (a Y or axillary view can confirm this)
there is subtle widening of the joint (> 6mm) or the bones overlap on a Grashey view (a Y or axillary view can confirm this) they are usually located within the scapular neck or body
they are usually located within the scapular neck or body pulmonary contusions and pleural effusions
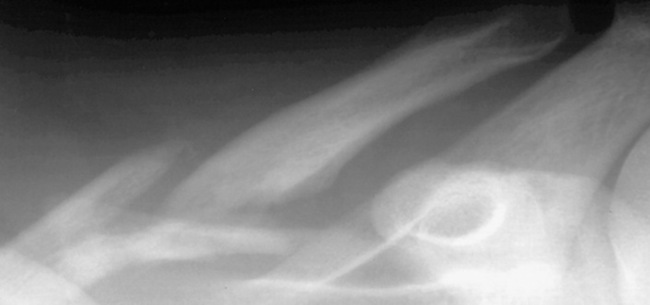
pulmonary contusions and pleural effusions fractures of the mid-third are the most common
fractures of the mid-third are the most common  distal fractures may disrupt the coracoclavicular ligaments (± involve the acromioclavicular joint)
distal fractures may disrupt the coracoclavicular ligaments (± involve the acromioclavicular joint)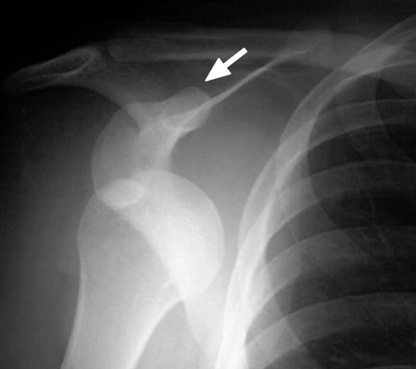
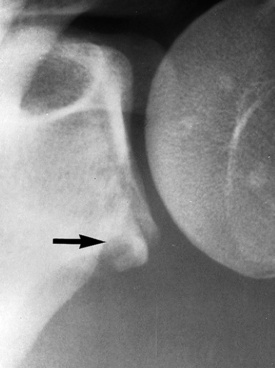


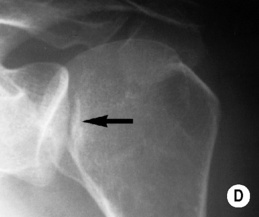

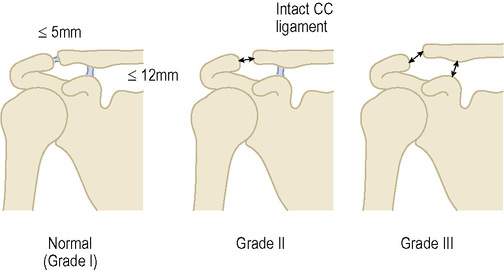
 the coracoclavicular distance is 11–12mm
the coracoclavicular distance is 11–12mm the clavicle is elevated less than a complete shaft width above the acromion
the clavicle is elevated less than a complete shaft width above the acromion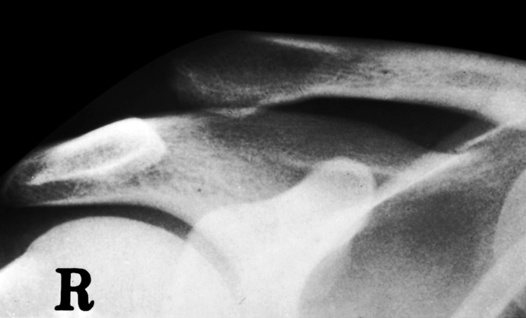





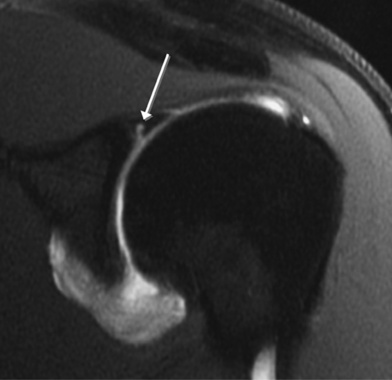
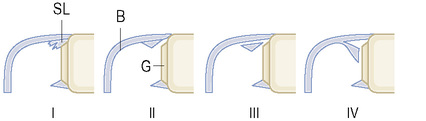
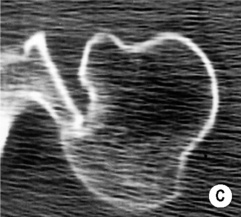
 B: biceps tendon
B: biceps tendon  G: glenoid cartilage.
G: glenoid cartilage.
 there is no surface defect
there is no surface defect