Skin and Soft Tissue
Jacob C. Miss
Bradley W. Frazee
INTRODUCTION
Skin and soft tissue infections and foreign bodies are encountered on a daily basis by emergency physicians. Ultrasound provides detailed images of subcutaneous and submucosal tissue, and is an extremely useful tool in the rapid assessment of these common problems. This chapter is divided into three sections that cover the diagnosis and evaluation of skin and soft tissue infections, subcutaneous foreign bodies, and soft tissue masses. Soft tissue procedures are covered in Chapter 22.
SKIN AND SOFT TISSUE INFECTIONS
Clinical Applications
Faced with an undifferentiated skin and soft tissue infection, ultrasound is useful to:
Confirm the presence of cellulitis
Detect occult or deep abscesses
Localize abscess pockets for accurate aspiration or incision, and
Identify fluid adjacent to fascial planes, indicative of necrotizing fasciitis.
Image Acquisition
Sonographic evaluation of skin and soft tissue infections is usually best accomplished with a 5 to 7.5 MHz linear array transducer. A 3.5 MHz convex array probe may be preferable in the case of deep collections, such as an intramuscular buttock abscess.  PEDIATRIC CONSIDERATIONS: A high frequency (6 to 13 MHz) small footprint linear probe is indicated in young children. Often the vascular probe can serve this purpose. Given the high water content of the subcutaneous tissue of children, increase the gain to visualize subtle details of pediatric soft tissue infections.
PEDIATRIC CONSIDERATIONS: A high frequency (6 to 13 MHz) small footprint linear probe is indicated in young children. Often the vascular probe can serve this purpose. Given the high water content of the subcutaneous tissue of children, increase the gain to visualize subtle details of pediatric soft tissue infections. Fluid collections should be interrogated in two planes to define their shape. Depth is estimated using the depth markers at the side of the display. It is helpful to compare the area of interest to the contralateral side to define the normal depth of subcutaneous tissue, fascial planes, and muscle. In the case of superficial infections, particularly of the hand, use of a standoff pad or water bath is recommended to optimize image quality where small anatomic structures and bones are located near the skin surface.
Fluid collections should be interrogated in two planes to define their shape. Depth is estimated using the depth markers at the side of the display. It is helpful to compare the area of interest to the contralateral side to define the normal depth of subcutaneous tissue, fascial planes, and muscle. In the case of superficial infections, particularly of the hand, use of a standoff pad or water bath is recommended to optimize image quality where small anatomic structures and bones are located near the skin surface.
 PEDIATRIC CONSIDERATIONS: A high frequency (6 to 13 MHz) small footprint linear probe is indicated in young children. Often the vascular probe can serve this purpose. Given the high water content of the subcutaneous tissue of children, increase the gain to visualize subtle details of pediatric soft tissue infections.
PEDIATRIC CONSIDERATIONS: A high frequency (6 to 13 MHz) small footprint linear probe is indicated in young children. Often the vascular probe can serve this purpose. Given the high water content of the subcutaneous tissue of children, increase the gain to visualize subtle details of pediatric soft tissue infections. Fluid collections should be interrogated in two planes to define their shape. Depth is estimated using the depth markers at the side of the display. It is helpful to compare the area of interest to the contralateral side to define the normal depth of subcutaneous tissue, fascial planes, and muscle. In the case of superficial infections, particularly of the hand, use of a standoff pad or water bath is recommended to optimize image quality where small anatomic structures and bones are located near the skin surface.
Fluid collections should be interrogated in two planes to define their shape. Depth is estimated using the depth markers at the side of the display. It is helpful to compare the area of interest to the contralateral side to define the normal depth of subcutaneous tissue, fascial planes, and muscle. In the case of superficial infections, particularly of the hand, use of a standoff pad or water bath is recommended to optimize image quality where small anatomic structures and bones are located near the skin surface.Normal Ultrasound Anatomy
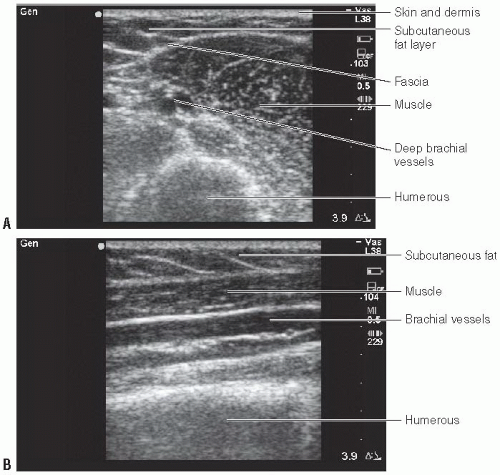
Examination of the skin and subcutaneous tissue reveals several layers of tissue, beginning with the cutaneous layer of epidermis and dermis, deep to which lies the subcutaneous fat which is separated from muscle by fascia. The cutaneous layer occupies only a few millimeters of the near field and is not visualized in detail using typical frequencies employed by most emergency department (ED) equipment. Normal subcutaneous tissue is composed primarily of fat, which appears hypoechoic, and is traversed by irregular strands of
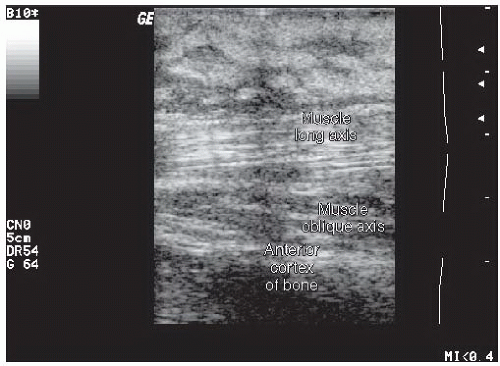
hyperechoic connective tissue. Fascia is comprised of connective tissue that is sharply defined, usually thin, regular, and hyperechoic. Fascia demarcates the subcutaneous fat from the underlying muscle fibers. Muscle fibers are organized into bundles that are divided by fibroadipose septa. The muscle fibers themselves are hypoechoic (isoechoic with subcutaneous fat); the fibroadipose septa that traverse the muscle fibers are hyperechoic and regular. In the long axis of a muscle, these septa give a characteristic appearance described by some as “veins on a leaf” or “feather-like.” In short axis, the echogenic septa are scattered between the muscle fibers, giving a speckled appearance sometimes referred to as a “starry night.” Vessels are tubular and anechoic. In long axis, they appear retangular; in short axis, they are round or oval. Arteries usually are pulsatile, while veins compress with gentle transducer pressure. Both demonstrate color flow by Doppler. Lymph nodes are seen as irregular, circular structures, often with an echogenic center surrounded by a hypoechoic rim. Bones, with their brightly echogenic cortex and dense acoustic shadow, can often be seen in the far field of the image, providing a useful landmark and depth perspective. Figure 20.1 demonstrates normal sonographic appearance of the subcutaneous structures of the arm.
hyperechoic connective tissue. Fascia is comprised of connective tissue that is sharply defined, usually thin, regular, and hyperechoic. Fascia demarcates the subcutaneous fat from the underlying muscle fibers. Muscle fibers are organized into bundles that are divided by fibroadipose septa. The muscle fibers themselves are hypoechoic (isoechoic with subcutaneous fat); the fibroadipose septa that traverse the muscle fibers are hyperechoic and regular. In the long axis of a muscle, these septa give a characteristic appearance described by some as “veins on a leaf” or “feather-like.” In short axis, the echogenic septa are scattered between the muscle fibers, giving a speckled appearance sometimes referred to as a “starry night.” Vessels are tubular and anechoic. In long axis, they appear retangular; in short axis, they are round or oval. Arteries usually are pulsatile, while veins compress with gentle transducer pressure. Both demonstrate color flow by Doppler. Lymph nodes are seen as irregular, circular structures, often with an echogenic center surrounded by a hypoechoic rim. Bones, with their brightly echogenic cortex and dense acoustic shadow, can often be seen in the far field of the image, providing a useful landmark and depth perspective. Figure 20.1 demonstrates normal sonographic appearance of the subcutaneous structures of the arm.
Pathology
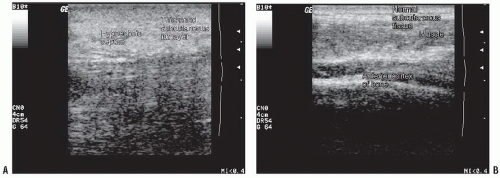
Most of the findings associated with cellulitis arise from edema formation and are nonspecific. Swelling is reflected in an increased distance between the skin and underlying fascia or bone (Fig. 20.2). The echogenicity of the subcutaneous tissue is diffusely increased, and often is traversed by a lattice of broad hypoechoic bands, giving rise to a cobblestone appearance (Figs. 20.3, 20.4 and 20.6). Differentiating interconnected bands of edema fluid from an irregular pus collection can be difficult (Figs. 20.5 and 20.6).
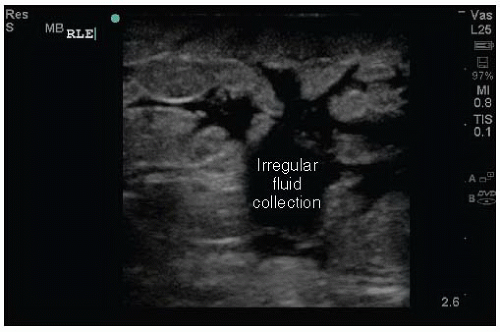
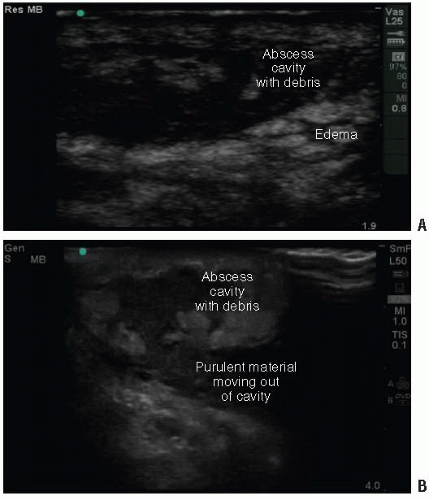
Although subcutaneous abscesses most commonly appear as hypoechoic roughly spherical masses (Figs. 20.7 and 20.8), it is important to realize that the sonographic appearance can be quite variable (1). Abscesses are organized collections of purulent material and debris. Some are well formed and sharply demarcated. However, in some, the contour may be lobulated or interdigitated with surrounding edema and tissue planes (Figs. 20.5 and 20.9). The interior may contain hyperechoic sediment (Fig. 20.7), septae, or gas and may be isoechoic or hyperechoic compared to surrounding tissue (Fig. 20.10). In the latter case, clues to the presence of liquefied pus are the findings of posterior acoustic enhancement (Figs. 20.7, 20.8, and 20.10) and the ability to induce motion of the material with palpation (Fig. 20.11;  VIDEO 20.1) (2,3). Figure 20.12 (
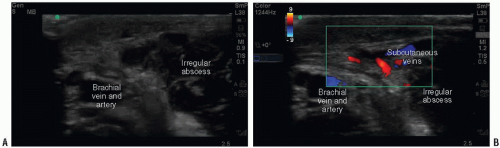
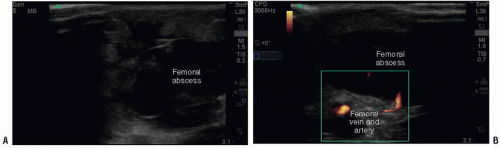
VIDEO 20.1) (2,3). Figure 20.12 ( VIDEO 20.2) demonstrates the typical appearance of a deep intramuscular abscess. Once an abscess is identified, ultrasound is also useful to identify adjacent vascular
VIDEO 20.2) demonstrates the typical appearance of a deep intramuscular abscess. Once an abscess is identified, ultrasound is also useful to identify adjacent vascular
structures prior to drainage to avoid inadvertent puncture (Figs. 20.13 and 20.14; VIDEOS 20.3 and 20.4). A standoff pad or water bath may be helpful to improve the image for small structures such as digits (Figs. 20.15 and 20.16;
VIDEOS 20.3 and 20.4). A standoff pad or water bath may be helpful to improve the image for small structures such as digits (Figs. 20.15 and 20.16;  VIDEO 20.5).
VIDEO 20.5).
 VIDEO 20.1) (2,3). Figure 20.12 (
VIDEO 20.1) (2,3). Figure 20.12 ( VIDEO 20.2) demonstrates the typical appearance of a deep intramuscular abscess. Once an abscess is identified, ultrasound is also useful to identify adjacent vascular
VIDEO 20.2) demonstrates the typical appearance of a deep intramuscular abscess. Once an abscess is identified, ultrasound is also useful to identify adjacent vascular structures prior to drainage to avoid inadvertent puncture (Figs. 20.13 and 20.14;
 VIDEOS 20.3 and 20.4). A standoff pad or water bath may be helpful to improve the image for small structures such as digits (Figs. 20.15 and 20.16;
VIDEOS 20.3 and 20.4). A standoff pad or water bath may be helpful to improve the image for small structures such as digits (Figs. 20.15 and 20.16;  VIDEO 20.5).
VIDEO 20.5).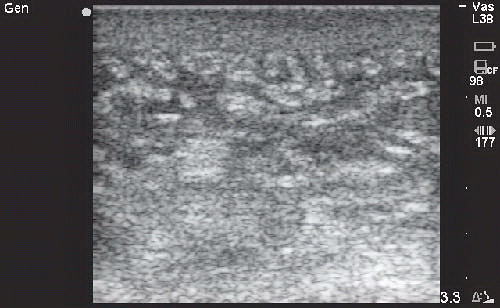 FIGURE 20.3. Cellulitis of the Forearm Demonstrating Prominent Hypoechoic Septae in the Subcutaneous Fat Layer, Giving Rise to a Cobblestone or Lattice Appearance. |
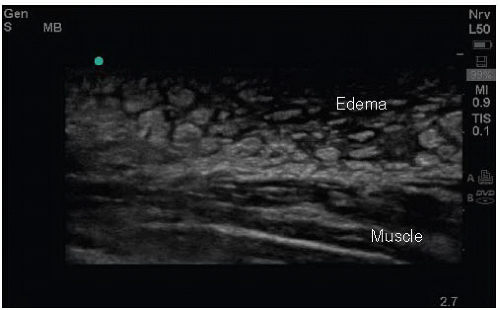 FIGURE 20.6. Lower Extremity Cellulitis with Prominent Near Field Edema Fluid that could be Confused with Pus. (Courtesy of Arun Nagdev, MD, Highland Hospital.) |
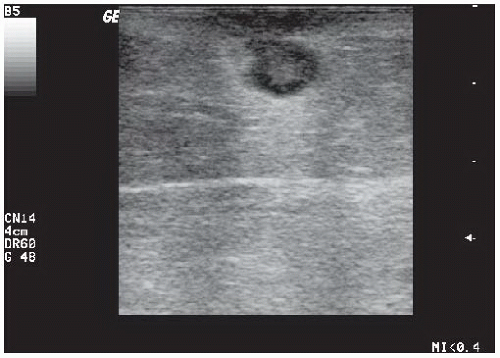 FIGURE 20.7. Typical Abscess. Spherical abscess cavity containing hyperechoic debris. Note far field acoustic enhancement. |
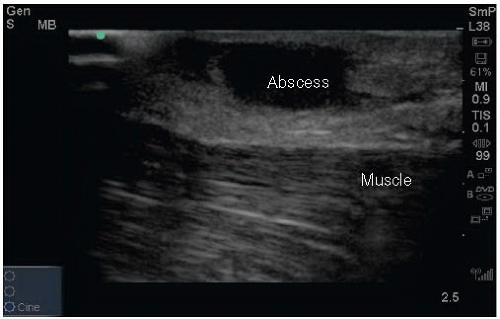 FIGURE 20.8. Axillary Abscess with Adjacent Cellulitis. Note the far field acoustic enhancement and deep muscle layer. |
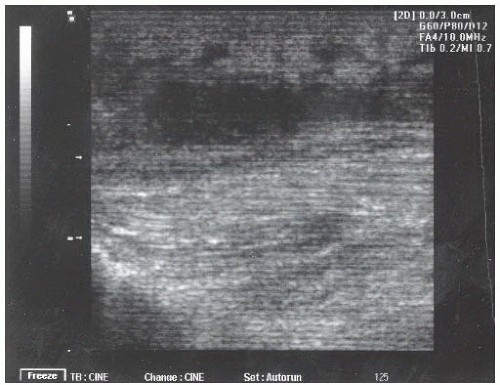 FIGURE 20.9. Atypical Appearing Subcutaneous Abscess. A broad irregular anechoic fluid collection is seen deep and adjacent to what appears to be cellulitis in the near field. |
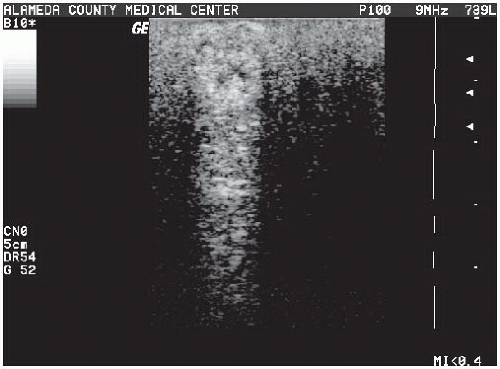 FIGURE 20.10. Iso-Hyperechoic Abscess Cavity Giving Rise to Prominent Far Field Acoustic Enhancement. |
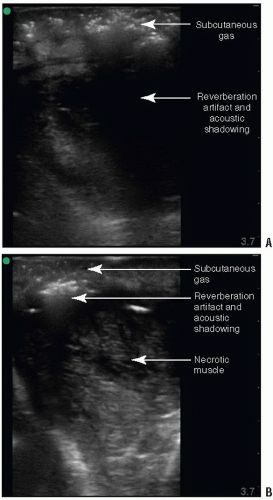
The sonographic appearance of necrotizing fasciitis includes marked thickening of the subcutaneous tissue when compared to the contralateral side (as seen in cellulitis) combined with a layer of anechoic fluid tracking along the fascia (Fig. 20.17;  VIDEO 20.6) (4). Yen and co-authors reported that the fluid layer should measure at least 4 mm, although this criteria has yet to be confirmed by others (1). Subcutaneous gas, which may give rise to acoustic shadowing and reverberation artifact, is reliably detected by ultrasound (5), and is present in some cases of necrotizing fasciitis (Fig. 20.18;
VIDEO 20.6) (4). Yen and co-authors reported that the fluid layer should measure at least 4 mm, although this criteria has yet to be confirmed by others (1). Subcutaneous gas, which may give rise to acoustic shadowing and reverberation artifact, is reliably detected by ultrasound (5), and is present in some cases of necrotizing fasciitis (Fig. 20.18;  VIDEOS 20.7 and 20.8) (4, 5, 6, 7). Yen and coworkers found that ED ultrasound had a sensitivity of 88.2% and specificity of 93.3% for necrotizing fasciitis in a case series of 62 patients (1).
VIDEOS 20.7 and 20.8) (4, 5, 6, 7). Yen and coworkers found that ED ultrasound had a sensitivity of 88.2% and specificity of 93.3% for necrotizing fasciitis in a case series of 62 patients (1).
 VIDEO 20.6) (4). Yen and co-authors reported that the fluid layer should measure at least 4 mm, although this criteria has yet to be confirmed by others (1). Subcutaneous gas, which may give rise to acoustic shadowing and reverberation artifact, is reliably detected by ultrasound (5), and is present in some cases of necrotizing fasciitis (Fig. 20.18;
VIDEO 20.6) (4). Yen and co-authors reported that the fluid layer should measure at least 4 mm, although this criteria has yet to be confirmed by others (1). Subcutaneous gas, which may give rise to acoustic shadowing and reverberation artifact, is reliably detected by ultrasound (5), and is present in some cases of necrotizing fasciitis (Fig. 20.18;  VIDEOS 20.7 and 20.8) (4, 5, 6, 7). Yen and coworkers found that ED ultrasound had a sensitivity of 88.2% and specificity of 93.3% for necrotizing fasciitis in a case series of 62 patients (1).
VIDEOS 20.7 and 20.8) (4, 5, 6, 7). Yen and coworkers found that ED ultrasound had a sensitivity of 88.2% and specificity of 93.3% for necrotizing fasciitis in a case series of 62 patients (1).Artifacts and Pitfalls
Potential pitfalls in the ultrasound assessment of soft tissue infections include the following.
Failure to recognize an isoechoic abscess cavity (evident by the presence of far field acoustic enhancement),
Failure to recognize that irregular hypoechoic areas may represent pus collections rather than simply edema, and
Failure to optimize scanning technique with use of a standoff pad to interrogate superficial infections, particularly in the hand.
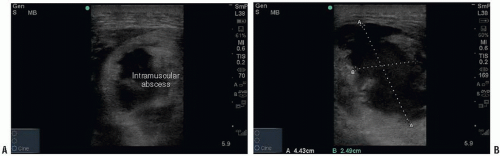 FIGURE 20.12. A: Intramuscular abscess in the triceps. B: Notice the irregularity of the internal wall of the abscess and deeper extension of the abscess toward the humerus. |
Comparison with Other Imaging Modalities
Computed tomography (CT) has been used extensively to evaluate soft tissue infections, and may be considered the gold standard for imaging abscesses. Its advantages are that it reveals deep fluid collections well, it can delineate the extent of inflammation (in relation to fascia, vessels and bone), and it is well accepted by surgeons. Disadvantages compared to ultrasound are its high cost, that it is time consuming, and that it cannot be employed at the bedside to directly guide aspiration or incision.
For the evaluation of possible necrotizing soft tissue infection, the gold standard remains operative findings. Plain films reveal the characteristic soft tissue gas in as little as 39% of cases (8). CT scan and magnetic resonance imaging (MRI) may demonstrate edema adjacent to fascial planes or small amounts of soft tissue gas, but these imaging modalities are time consuming and may present an additional risk to an unstable patient (9). Ultrasound is an attractive alternative in this setting because it can be performed rapidly at the bedside. While one prospective study has reported favorable results with screening ED ultrasound for suspected necrotizing fasciitis, published clinical experience from other centers remains limited to case reports, and data comparing ultrasound to more accepted imaging modalities such as CT or MRI are still lacking (1,6,7).
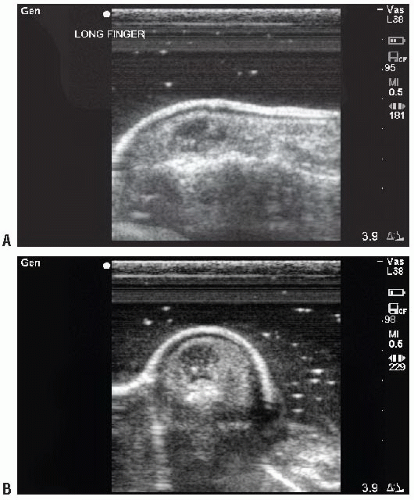 FIGURE 20.15. Fingertip Felon. A water-filled latex glove was used as a standoff pad. A: Longitudinal view. B: Transverse view. |
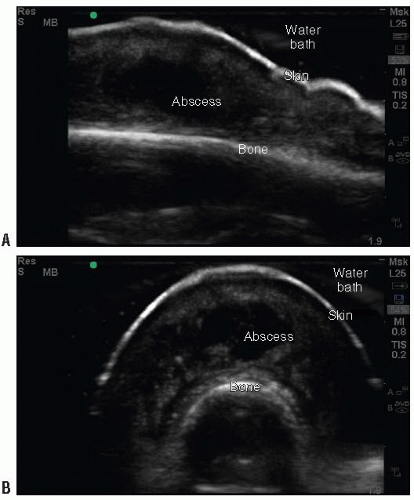 FIGURE 20.16. Dorsal Finger Abscess. Images were obtained by placing the hand in a water bath. A: Longitudinal view. B: Transverse view. |
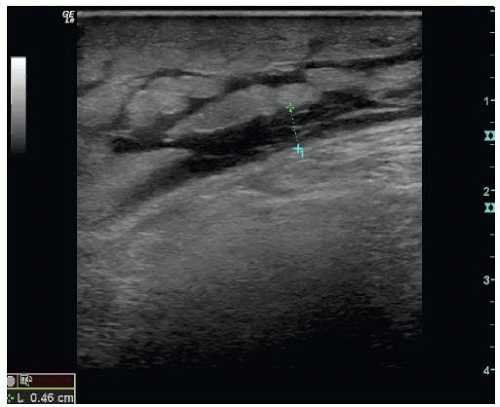 FIGURE 20.17. Necrotizing Fasciitis of the Thigh with Marked Subcutaneous Edema and a Fluid Layer along the Fascia. |
Use of the Image in Clinical Decision Making
Although CT scanning is known to reliably identify soft tissue fluid collections, bedside ultrasound may reveal the correct diagnosis much more rapidly and at less cost, and it provides real-time localization (8). Even novice ED sonographers were capable of identifying abscesses by ultrasound with minimal training (10). A general approach to skin and soft tissue infections that incorporates bedside ultrasound is presented in Figure 20.19. In many cases the diagnosis of abscess is clinically obvious based on the finding of fluctuance or drainage. On the other hand, when cellulitis seems likely, the provider should be careful to consider the possibility of an occult or early abscess, or necrotizing soft tissue infection NSTI. When doubt exists about the possibility of an abscess, ultrasound is used to search below the surface for a subcutaneous or intramuscular fluid collection. In addition, ultrasound can be used to define the best location for aspiration or incision, where the collection is largest and closest to the skin surface.
The utility of such an approach in the ED setting has been investigated by multiple groups. In one study of 107 patients with skin and soft infections, addition of bedside ultrasound to the history and physical resulted in a change in clinical impression in 17% of cases, and led to successful abscess drainage in eight cases in which it otherwise would not have been attempted (2). In another study of 126 patients, ultrasound correctly changed management in 48% of cases in which providers thought drainage was not needed on the basis of physical exam alone. Ultrasound also changed management in 73% of cases where drainage was thought to be needed, including 8 cases in which the location or depth of the incision was changed (11). Ultrasound has also been shown to improve diagnostic accuracy and change management in pediatric skin and soft tissue infections (12,13). A study involving 50 children found that bedside ultrasound changed management in 22% of cases and had a sensitivity of 90% and a specificity of 83% in detecting fluid collections requiring drainage (14).  PEDIATRIC CONSIDERATIONS: An important consideration in children is that abscess drainage may require conscious sedation with its attendant risks. Correct identification of soft tissue infections by ultrasound helps reduce unnecessary interventions.
PEDIATRIC CONSIDERATIONS: An important consideration in children is that abscess drainage may require conscious sedation with its attendant risks. Correct identification of soft tissue infections by ultrasound helps reduce unnecessary interventions. Ultrasound may be particularly useful in abscesses occurring around the head and neck and in the groin, where vascular structures are numerous (Figs. 20.13 and 20.14) and in sites where prior infections and surgical scars can alter the surface presentation of an underlying pus pocket (15, 16, 17, 18). (See Case at the end of the chapter.)
Ultrasound may be particularly useful in abscesses occurring around the head and neck and in the groin, where vascular structures are numerous (Figs. 20.13 and 20.14) and in sites where prior infections and surgical scars can alter the surface presentation of an underlying pus pocket (15, 16, 17, 18). (See Case at the end of the chapter.)
 PEDIATRIC CONSIDERATIONS: An important consideration in children is that abscess drainage may require conscious sedation with its attendant risks. Correct identification of soft tissue infections by ultrasound helps reduce unnecessary interventions.
PEDIATRIC CONSIDERATIONS: An important consideration in children is that abscess drainage may require conscious sedation with its attendant risks. Correct identification of soft tissue infections by ultrasound helps reduce unnecessary interventions. Ultrasound may be particularly useful in abscesses occurring around the head and neck and in the groin, where vascular structures are numerous (Figs. 20.13 and 20.14) and in sites where prior infections and surgical scars can alter the surface presentation of an underlying pus pocket (15, 16, 17, 18). (See Case at the end of the chapter.)
Ultrasound may be particularly useful in abscesses occurring around the head and neck and in the groin, where vascular structures are numerous (Figs. 20.13 and 20.14) and in sites where prior infections and surgical scars can alter the surface presentation of an underlying pus pocket (15, 16, 17, 18). (See Case at the end of the chapter.)NSTI can be rapidly fatal without prompt recognition and definitive surgical debridement. Yet accurate diagnosis remains notoriously difficult. Plain x-rays are insensitive, whereas CT and MRI may be impractical in an unstable patient. Although the role of bedside ultrasound remains to be defined, findings of marked subcutaneous edema, fluid adjacent to fascia and subcutaneous gas support the diagnosis and may be sufficient confirmatory evidence to proceed to surgery (4, 5, 6, 7). With the possible exception of MRI, no imaging modality is considered sensitive enough to exclude the diagnosis of necrotizing soft tissue infection once it is suspected on clinical grounds. A low threshold for surgical exploration should be maintained regardless of the results of imaging.
SOFT TISSUE FOREIGN BODY
Clinical Applications
Retained foreign bodies can complicate skin and soft tissue injuries. Despite their usual superficial location, foreign bodies are difficult to detect by history and physical exam alone and are frequently overlooked. In a retrospective review of 200 patients referred for evaluation of retained foreign bodies in the hand, 38% were misdiagnosed on their index visit (19). Missed foreign bodies are also one of the most common causes of malpractice claims against emergency physicians (20,21). In the case of a suspected soft
tissue foreign body, ultrasound can be used to accomplish the following:
tissue foreign body, ultrasound can be used to accomplish the following:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree