Key Points
- •
Point-of-care ultrasound can aid in diagnosis of cellulitis and identify patients with underlying abscess or necrotizing fasciitis.
- •
Diagnosis and removal of retained foreign bodies can be guided by use of bedside ultrasound.
- •
Tendonitis and fracture are two common conditions that can be accurately diagnosed using point-of-care ultrasound.
Background
Ultrasonography of skin and soft tissues is an extremely useful tool for providers of different specialties. Interrogation of the skin and soft tissues can inform the provider of a variety of ailments including cellulitis, abscess, foreign bodies, fractures, and tendonitis.
Infection
One of the most common uses of point-of-care ultrasound is to help distinguish between cellulitis and subcutaneous abscess. With the increasing prevalence of methicillin-resistant Staphylococcus aureus , presentation of patients with skin infections has increased. In many circumstances, physical exam is limited in differentiating cellulitis from abscess, and definitive therapy, namely, abscess incision and drainage, may be delayed. Bedside ultrasound expedites initiation of appropriate management in patients with cellulitis with or without abscess. In patients with suspected necrotizing fasciitis, ultrasonography can be performed rapidly at the bedside to expedite confirmation of diagnosis and initiation of emergent therapy.
Tendonitis and Fracture
Use of bedside ultrasonography to diagnose tendonitis and fractures has increased rapidly due to the availability of less expensive, portable devices that generate high-quality images. A focused bedside ultrasound exam following physical examination has been used to diagnose various tendon pathologies, including tendonitis and tendon rupture or tear.
Ultrasonography is a simple and accurate technique to diagnose fractures at the bedside in time-sensitive situations and austere environments with limited access to plain film radiography. Studies are ongoing to validate the utility of bedside ultrasound to aid in reduction of fractures.
Foreign Bodies
Retained foreign bodies are common and are a nidus for soft tissue infection. Physical examination is insensitive for detecting foreign bodies, and retained foreign bodies are associated with high medical-legal risk. Point-of-care ultrasonography can aid in identifying retained foreign bodies such as wood, metal, or glass and can delineate borders to guide removal of the foreign body.
Neoplasm
Providers can use ultrasonography to differentiate soft tissue tumors from fluid collections (cysts, abscess) in patients presenting with a soft tissue nodule. Abnormal findings seen on ultrasound must be considered in clinical context. Additional workup, including imaging or biopsy of the lesion, should be obtained if neoplasm is suspected.
Image Acquisition
A high-frequency linear array transducer (5–12 MHz) should be used to provide the best resolution when imaging the skin and soft tissues. When visualizing structures deeper than 4 cm, a high-frequency transducer may not provide adequate penetration, and a low-frequency transducer may be used. For example, a low-frequency transducer is often required to image a deep abscess over the femur in an obese adult patient.
When imaging areas of suspected infection, it is recommended to cover the transducer with a barrier, such as nonsterile glove or plastic sheath, to minimize contamination of the transducer with potentially resistant bacteria. Gel should be placed inside the barrier. After every ultrasound exam, the transducer must be cleaned with approved antiseptic wipes.
The transducer should be used to evaluate the area of interest methodically and systematically. Orthogonal views (i.e., longitudinal and transverse views) should be obtained of the area of interest to elucidate the surrounding anatomy. Important surrounding structures, such as blood vessels, nerves, and lymph nodes, should be identified. Dimensions of fluid collections should be measured in two planes, along with depth of collections. Compressibility may help differentiate fluid collections from solid lesions. Color flow Doppler and power Doppler can be used to evaluate the area of interest to identify surrounding vessels.
Pathologic Findings
Cellulitis, Subcutaneous Abscess, and Necrotizing Fasciitis
A transducer cover or barrier is recommended when acquiring images from an infected area of skin or soft tissues. A copious amount of gel over the area of interest minimizes pressure of the transducer on the skin, thereby decreasing patient discomfort during the exam.
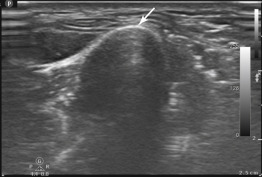
Normal anatomy can be compared to abnormal areas with suspected pathology ( Figure 36.1 ). Initially, cellulitis will result in thickening of the subcutaneous layer. As cellulitis progresses, subcutaneous edema increases and appears as a “cobblestone” pattern ( Figure 36.2 ). This is a result of edema forming around fat and connective tissue. Color flow Doppler may highlight areas of hyperemia due to inflammation ( Figure 36.3 ).
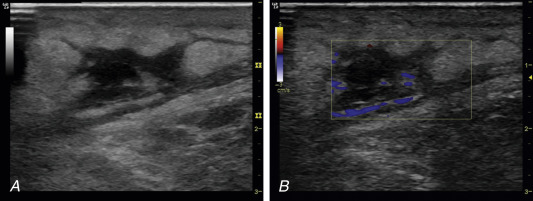
Ultrasound appearance of abscesses can be anechoic, hypoechoic, or hyperechoic, but all abscesses exhibit posterior acoustic enhancement. A hyperechoic rim often surrounds abscesses with some hyperemia demonstrated by color flow Doppler. Absence of flow centrally within a suspected abscess ensures that the anechoic area is not a vessel ( Figure 36.4 ). Compression of an abscess may cause swirling of pus to be visualized sonographically ( ![]() ).
).
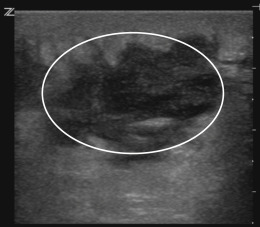
In clinically suspected cases of necrotizing fasciitis, availability of bedside ultrasound can expedite confirmation of diagnosis. The presence of air within soft tissues is pathognomonic for necrotizing fasciitis. Air creates multiple comet-tail artifacts that create shadows and obscure visualization of deep structures ( Figure 36.5 ). In addition, fluid along the deep fascia greater than 5 mm in thickness may be an early sonographic sign of necrotizing fasciitis.
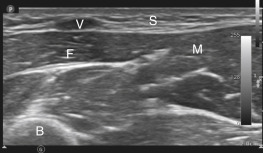
Tendonitis
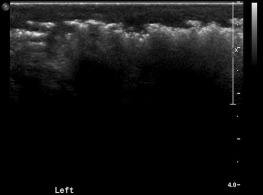
Normal tendons appear as discrete fibrillar structures. Tendonitis is seen on ultrasound as thickened, hypoechoic areas as a result of edema within the tendon ( Figure 36.6 ). It is important to recognize when interpreting scans of tendons, particularly at insertion points, that a hypoechoic area may result from anisotropy rather than actual pathology. Anisotropy occurs when tendons are visualized at an angle. Hypoechoic areas created by anisotropy disappear by changing the angle of the transducer, and therefore tendons should be visualized in orthogonal planes to rule out anisotropy.
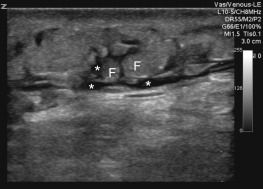
Fracture
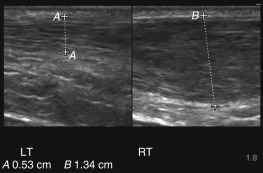
Outer cortex of bone appears as a hyperechoic line with shadowing posteriorly ( Figure 36.7 ). Disruption of the cortical hyperechoic line represents a fracture and is best visualized in a longitudinal plane ( Figures 36.8 and 36.9 ). Reverberation artifact may sometimes appear in a longitudinal plane, and determining which hyperechoic line is bone versus artifact may be difficult. Turning the probe in a transverse plane and noting the depth of the cortex helps determine which hyperechoic line represents bone ( Figure 36.7 ).