Key Points
- •
Upper extremity deep venous thrombosis (DVT) is underdiagnosed, and the incidence of pulmonary embolism due to upper extremity DVT is underestimated.
- •
The major veins of the upper extremity are divided into deep and superficial. The deep veins should be visualized in a transverse plane to evaluate for DVT, with the exception of the subclavian vein.
- •
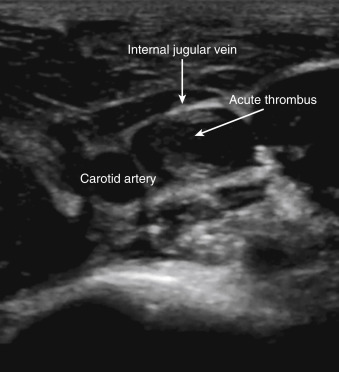
The cardinal feature of DVT is noncompressibility of the vein. Acute thrombi appear hypoechoic and are loosely attached to vein walls, whereas chronic thrombi are hyperechoic and adherent to the walls.
Background
Ultrasonography of the upper extremity venous system has wide applications, including evaluation for thrombus, guidance of venous catheter insertion, preoperative mapping for hemodialysis arteriovenous fistula or graft placement, and postoperative assessment of venous patency. This chapter focuses on use of point-of-care ultrasound to diagnose upper extremity deep venous thrombosis (DVT), including examination technique, imaging protocols, and common pitfalls.
Annual incidence of upper extremity DVT (UEDVT) is approximately 3.6/100,000, occurring predominantly in patients with malignancy, critical illness, obesity, and central venous catheters. Underdiagnosis is a concern given the frequent lack of symptoms with nonocclusive internal jugular vein or subclavian vein thrombosis. The reported risk of pulmonary embolism is lower with UEDVT (2–17%) than with lower extremity DVT, although the actual prevalence of UEDVT is not known. The perceived lower risk leads to fewer evaluations for DVT in upper extremities compared to lower extremities. Despite the strong association of venous catheters, pacemaker wires, and infusion ports with thrombosis, few studies have been published about the pathophysiology of UEDVT. Reported incidence of UEDVT with indwelling catheters varies widely from 12% to 35%, with 75% of cases being asymptomatic. In at least one study, the incidence of DVT associated with central venous catheters appears to be higher with subclavian vein rather than internal jugular vein catheters (13% vs. 3%). Similarly, reported incidence of UEDVT associated with peripherally inserted catheters varies significantly, from 1.6% to as high as 27%.
Anatomy
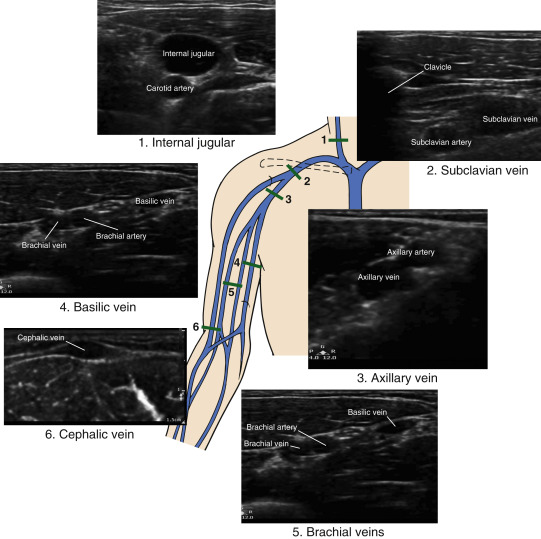
Veins of the upper extremity are divided into deep and superficial veins ( Figure 27.1 ). Deep veins of the upper extremity are paired with arteries that travel alongside the vein and both are named similarly. The ulnar and radial veins ascend medially and laterally, respectively, along the forearm to form the brachial veins in the area of the antecubital fossa. The brachial veins anastomose with the basilic vein in the upper arm to become the single axillary vein at the inferior margin of the teres major muscle. The axillary vein becomes the subclavian vein at the lateral aspect of the first rib. The subclavian vein lies anterior to the subclavian artery at this level. The subclavian and internal jugular veins anastomose behind the medial aspect of the clavicle to form the innominate, or brachiocephalic, vein that drains into the superior vena cava.
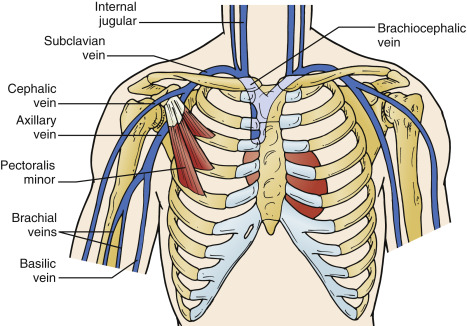
An ultrasound examination of the upper extremity veins is not complete without assessing the internal jugular vein, even though it is located in the neck. The internal jugular vein is within the carotid sheath and travels from the jugular foramen in the base of the skull to behind the clavicle, where it fuses with the subclavian vein.
The main superficial veins of the upper extremities are the cephalic, basilic, and median cubital veins. The superficial veins do not have accompanying arteries. The cephalic vein ascends along the lateral aspect of the biceps, turns medially into the deltopectoral groove, pierces the clavipectoral fascia below the clavicle, and merges with the upper axillary vein. The basilic vein runs along the medial aspect of the upper arm, pierces the deep fascia in the mid–upper arm, and joins the brachial vein to become the axillary vein in the axilla. The median cubital vein runs in the antecubital fossa between the cephalic and basilic veins.
Image Acquisition
The patient should be supine with the arm externally rotated and abducted 90 degrees from the chest, resting comfortably ( Figure 27.2 ). The patient’s head is turned to the contralateral side and kept elevated above the extremity being examined to avoid external compression of the distal subclavian vein between first rib and clavicle.
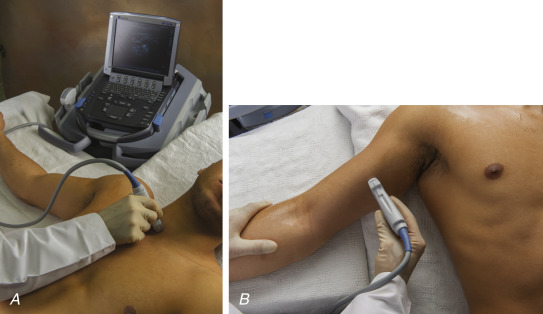
A high-frequency (5–12 MHz) linear transducer is used to scan all upper extremity vessels. For superficial veins, the frequency can be increased to 10 MHz for better resolution of smaller vessels.
When the operator is facing the patient as shown in Figure 27.2 , the transducer is oriented with the marker pointing toward the operator’s left side (patient’s right side) to image veins in a transverse plane, except for the subclavian vein, which is imaged longitudinally below the clavicle.
Technique
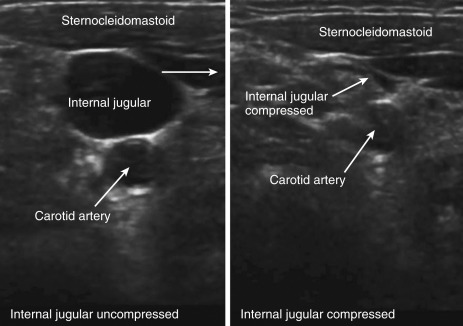
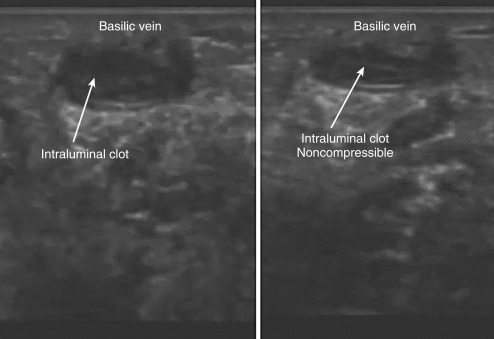
In two-dimensional mode, the transducer is placed transversely over the proximal upper extremity. Depth and gain are adjusted as previously described in Chapter 26, Lower Extremity Deep Venous Thrombosis . The lumen of a normal, patent vein appears anechoic. Compression ultrasound (CUS) consists of visualizing the vessel first without compression, followed by compression with light pressure to assess whether the anterior and posterior walls of the vessel come into contact, obliterating the lumen ( Figure 27.3 and ![]() ). Lack of complete, wall-to-wall compressibility is indicative of intraluminal thrombus, even if echogenic thrombus is not visualized ( Figure 27.4 and
). Lack of complete, wall-to-wall compressibility is indicative of intraluminal thrombus, even if echogenic thrombus is not visualized ( Figure 27.4 and ![]() ) Compressions are performed every 1–2 cm along the course of the vein, requiring a detailed understanding of venous anatomy ( Figure 27.5 ). Because thrombosis often occurs at venous junctions, providers must thoroughly evaluate the cephalic-axillary, basilic-axillary, and internal jugular-subclavian vein junctions. An UEDVT ultrasound exam includes evaluation of the following veins:
) Compressions are performed every 1–2 cm along the course of the vein, requiring a detailed understanding of venous anatomy ( Figure 27.5 ). Because thrombosis often occurs at venous junctions, providers must thoroughly evaluate the cephalic-axillary, basilic-axillary, and internal jugular-subclavian vein junctions. An UEDVT ultrasound exam includes evaluation of the following veins:
- ▪
Internal jugular vein (starting at the most cranial segment)
- ▪
Subclavian vein
- ▪
Axillary vein
- ▪
Brachial veins
- ▪
Basilic vein
- ▪
Cephalic vein
Forearm veins are not usually assessed unless focal findings are suspicious for thrombosis. Although superficial venous thrombosis does not require anticoagulation, a thrombus seen in a proximal segment of a superficial vein may prompt treatment if there is concern for extension into a deep vein.
Image Interpretation
Acute thrombi are typically hypoechoic or anechoic and are loosely attached to the wall of a vein. An acute thrombus fills the central portion of the venous lumen, and as the thrombus expands, the vein becomes occluded and rounder compared to normal ( Figure 27.6 and ![]() ). Nonocclusive thrombi usually do not cause rounding and enlargement of the vein ( Figure 27.7 and
). Nonocclusive thrombi usually do not cause rounding and enlargement of the vein ( Figure 27.7 and ![]() ). Chronic thrombi differ in appearance from acute thrombi; chronic thrombi appear more echogenic and eccentric (retracted to the wall) and are easily recognizable by ultrasound ( Figure 27.8 and
). Chronic thrombi differ in appearance from acute thrombi; chronic thrombi appear more echogenic and eccentric (retracted to the wall) and are easily recognizable by ultrasound ( Figure 27.8 and ![]() ).
).