Key Points
- •
Evaluation of enlarged lymph nodes with ultrasound includes assessment of size, shape, echogenicity, borders, and vascularity. In general, normal-sized lymph nodes are <1 cm, but size varies by location in the body from 0.5 to 2 cm.
- •
Abnormal lymph nodes are markedly hypoechoic, especially the hilum, and may have irregular borders, increased cortical thickness, and increased vascularity.
- •
In patients with enlarged cervical lymph nodes, a core-needle biopsy can be safely performed at the bedside using ultrasound guidance. Biopsy of lymph nodes <1 cm is not recommended because the procedure has low diagnostic yield and poses unnecessary risk to the patient.
Background
Increased availability of portable ultrasound with advanced technology has allowed providers to safely perform more procedures at the bedside. In particular, use of ultrasound to evaluate and guide percutaneous needle biopsies of head, neck, axillary, and inguinal lymph nodes has become more readily available. This chapter focuses on evaluation of neck lymph nodes, but the basic principles described in this chapter can be applied to evaluation of lymph nodes in other parts of the body.
Normal Anatomy
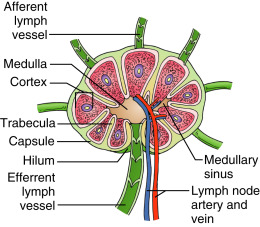
Lymph nodes are solitary structures composed of lymphoid tissue and are distributed along the course of lymphatic vessels. Each node is divided internally into cortex and medulla, and encased by a capsule. Lymph nodes are permeated by blood vessels. Both artery and vein enter and exit the lymph node at the hilus ( Figure 33.1 ).
Normal distribution of lymph nodes of the head and neck is illustrated in Figure 33.2 . In the cervical chains, at least six nodes can be routinely identified. In general, normal lymph nodes are not larger than 0.7–1 cm, but the normal size of lymph nodes varies greatly from 0.5 to 2.0 cm depending on the location in the body. Normal size of cervical nodes varies from 0.3 to 0.8 cm. Lymph nodes in the upper neck, specifically submandibular and upper cervical nodes, tend to be larger. A classification system of lymph nodes has been established to simplify ultrasound evaluation of the neck into eight regions ( Figure 33.3 ). This classification is distinct and does not replace the AJCC classification of cervical lymph nodes for cancer staging.
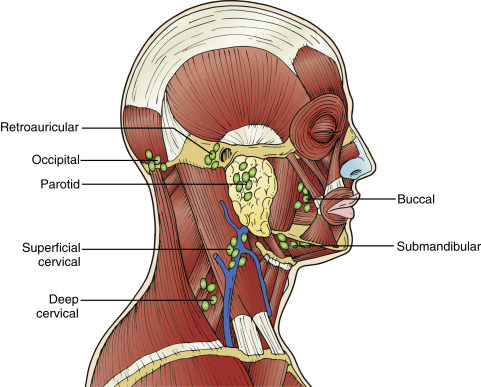
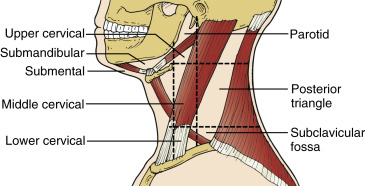
Image Acquisition
A high-frequency, linear array ultrasound transducer (5–10 MHz) should be used to examine lymph nodes. A linear transducer maximizes resolution of soft tissue structures while giving an adequate depth of 6–10 cm to visualize lymph nodes, vessels, and pleura.
For optimal imaging of neck lymph nodes, position the patient supine with a pillow between the scapulae. The head should be rotated to the contralateral side with the neck extended. Start by scanning the neck in a transverse plane in the submental area. Next, slide the transducer toward the submandibular area and orient the transducer parallel to the lower edge of the mandible with the ultrasound beam aimed superiorly toward the head. Sweep laterally toward the angle of the mandible. Obtain images of parotid lymph nodes in transverse and longitudinal planes. To scan cervical lymph nodes, start at the angle of the mandible with the transducer in a transverse orientation. Sequentially evaluate the upper, middle, and lower cervical nodes by sliding the transducer along the path of the internal jugular vein and common carotid artery, from the angle of the mandible to the junction of the internal jugular and subclavian veins.
Image Interpretation
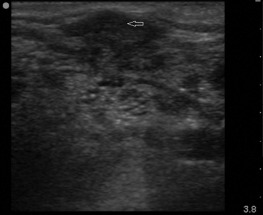
Normal size of head and neck lymph nodes is generally less than 0.8 cm. Diagnostic yield of biopsy will increase with lymph node size, and specificity might decrease if biopsy is performed of nodes <1 cm in size. As described above, normal lymph nodes are oval shaped and have a homogeneous echotexture. Normal lymph nodes have a distinct appearance of cortex and medulla. The outer cortex is hypoechoic due to lymphoid follicles, while the central medulla is hyperechoic due to a dense network of lymphatic cords and sinuses ( Figure 33.4 ). The center of lymph nodes may have some distinctly echogenic foci. Lymph node atrophy with cortical thinning, and fatty replacement of the hilum, is seen with aging.

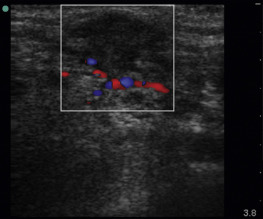
Abnormal lymph nodes are markedly hypoechoic with heterogeneous echotexture and change shape from oval to round ( Figures 33.5 and 33.6 ). Central hyperechogenicity of the hilum is reassuring of a benign lymph node, but a thin, hypoechoic hilum is suspicious of a pathologic lymph node that is infiltrated, inflamed, or malignant. Asymmetric cortical thickening is seen with subcapsular and sinusoidal metastatic invasion, along with irregular or sharp nodal borders. Cortical thickness more than half the transverse diameter of the hilum is abnormal. When color flow Doppler is applied to malignant lymph nodes, increased vascularity may be seen, especially in the hilar and perihilar areas ( Figure 33.7 and ![]() ). Abnormal lymph nodes with necrotic centers have a heterogeneous appearance with little to no vascularity detected ( Figure 33.8 ).
). Abnormal lymph nodes with necrotic centers have a heterogeneous appearance with little to no vascularity detected ( Figure 33.8 ).