A. Jejunal diverticulosis
B. Ischemic small bowel strictures
C. Carcinoid
D. Crohn disease
2 A 56-year-old patient presents with a long-standing history of diarrhea (12 months). Colonoscopy was reported as unremarkable. What is most likely diagnosis on this MR enterography?

T2 weighted fat saturated.

Diffusion weighted.

Postcontrast T1 weighted.
A. Active Crohn disease
B. Chronic Crohn disease
C. Small bowel lymphoma
D. Acute gastroenteritis
3 A 48-year-old male presents with mild right lower quadrant pain and a 2-day history of diarrhea. What is the most likely diagnosis?

A. Appendicitis
B. Lymphoma
C. Adenocarcinoma
D. Infection
4 Match the patient with the optimal imaging choice. Each choice may be used once, more than once, or not at all.
1. A 35-year-old male who has recently started a course of immunosuppressive therapy for newly diagnosed Crohn presents to the emergency department with worsening of abdominal pain for 1 week. On examination, he exhibits right lower quadrant guarding and is found to have a leukocytosis and fever.
2. A 20-year-old female diagnosed at age 15 with Crohn disease with a history of ileal strictures presents with a history of mild postprandial abdominal pain increasing over the past month.
3. A 56-year-old female with long-standing history of Crohn disease and history of a prior hysterectomy presents with urinary tract infections and pneumaturia.
4. A 73-year-old male who underwent an ileocolonoscopy for investigation of cramping abdominal pain with findings of mild ileal erosions suspicious for Crohn disease.
A. MR enterography
B. CT enterography or conventional CT
C. Barium small bowel follow-through
D. Capsule endoscopy
5a A 23-year-old female has a 5-year history of cramping abdominal pain and occasional diarrhea. Stool tests demonstrate increased fat. She undergoes a small bowel follow-through. What diagnosis is suggested by the findings?

A. Celiac disease
B. Crohn disease
C. Zollinger-Ellison syndrome
D. Giardiasis
5b The most common malignancy associated with untreated celiac disease is
A. Squamous cell carcinoma of the esophagus
B. T-cell lymphoma of the small bowel
C. Adenocarcinoma of the small bowel
D. Ovarian carcinoma
5c Cavitary mesenteric lymph node syndrome consists of
A. Low-attenuation lymph nodes, splenic atrophy, and villous atrophy
B. Low-attenuation lymph nodes, small bowel fold thickening, and mycobacterium tuberculosis infection
C. Low-attenuation lymph nodes, small bowel fold thickening, and migratory arthralgias
D. Low-attenuation lymph nodes, thyroiditis, and myasthenia gravis
6 A 68-year-old female with a history of total abdominal hysterectomy and bilateral salpingo-oophorectomy for cervical cancer with positive nodes presents 3 years later with cramping abdominal pain. A CT is obtained. What is the most likely diagnosis?


A. Graft versus host disease
B. Late-stage chemotherapy enteritis
C. Recurrent tumor
D. Chronic radiation enteritis
7 A 33-year-old male with a history of asthma and multiple food allergies (but not to wheat products) presents for the evaluation of chronic intermittent abdominal pain. A small bowel follow-through and a CT scan are performed. What diagnosis may best fit this clinical presentation?



A. Zollinger-Ellison syndrome
B. Celiac sprue
C. Giardiasis
D. Eosinophilic enteritis
8 A 39-year-old female with a history of bloating and postprandial abdominal pain undergoes a CT scan. A capsule endoscopy was originally planned, but based upon the CT findings, a small bowel follow-through was performed. What is the likely etiology for the findings?


A. Adenocarcinoma
B. Congenital atresia
C. Crohn disease
D. Nonsteroidal anti-inflammatory drug (NSAID)
9 A 56-year-old male presented to the emergency department with a history of 2-day acute onset of severe abdominal pain and nausea. He is afebrile, in normal sinus rhythm, but has a mild leukocytosis of 12.2 × 109/L. An abdominopelvic CT is performed. Images revealed no vascular occlusions. His medication list is reviewed. Which medication is most likely related to the findings on CT?


A. Aspirin
B. Propranolol (beta-blocker)
C. Lisinopril (angiotensin-converting enzyme inhibitor)
D. Omeprazole (proton pump inhibitor)
A. Anisakis
B. Ascaris
C. Hookworm
D. Trichuris
10b Extended matching:
Each answer may be used only once.
1. Ingestion of sushi
2. Rectal prolapse
3. Iron deficiency anemia
4. Cholangitis or pancreatitis
A. Ascaris
B. Trichuris
C. Hookworm
D. Anisakis
11a A 50-year-old patient with a history of intermittent diarrhea and facial flushing undergoes a CT of the abdomen. No other abnormalities of the GI tract were present on other images. The patient denies any significant travel history. What is the most likely diagnosis?


A. Tuberculosis of distal ileum and associated nodal enlargement
B. Small bowel lymphoma
C. Ileal carcinoid and calcified nodal metastasis
D. Crohn disease
11b What do the patient’s presenting symptoms likely indicate?
A. The tumor is metastatic to the liver.
B. The tumor is metastatic to the lungs.
C. The tumor is unresectable.
D. The tumor is likely multifocal.
12 A 49-year-old male with abdominal pain, diarrhea, and weight loss has a CT showing a large mass involving the jejunum. What is the most likely diagnosis?

A. Adenocarcinoma
B. Gastrointestinal stromal tumor
C. Non-Hodgkin lymphoma
D. Carcinoid
13 A 45-year-old male presents with postprandial abdominal bloating. A small bowel follow-through is performed. What is the likely diagnosis?
D.


A. Normal peristalsis
B. Crohn disease
C. Gastrointestinal stromal tumor
D. Adenocarcinoma
A. GISTs most commonly present with small bowel obstruction.
B. The associated lymphadenopathy is typically larger than the primary tumor.
C. Cystic transformation is commonly seen with treated metastases.
D. The lungs are the most common site of metastases.
A. Brunner gland hamartomas
B. Heterotopic gastric mucosa
C. Flexural pseudotumor
D. Prolapsing gastric mucosa
A. Gastrointestinal stromal tumor
B. Carcinoid
C. Lymphoma
D. Adenocarcinoma
17 The most common type of malignancy involving the small bowel is
A. Gastrointestinal stromal tumor
B. Lymphoma
C. Carcinoid
D. Metastases
18 The most common cause for small bowel obstruction in the United States is
A. Adhesions
B. Hernias
C. Neoplasm
D. Crohn disease
19 A 78-year-old male develops nausea, vomiting, and increased abdominal pain 2 days after a cystectomy. Supine and upright abdominal films are performed. The most appropriate test to order next would be


A. No further test needed; the exam is diagnostic.
B. CT
C. Small bowel follow-through
D. MRI
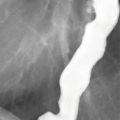
20a A 78-year-old female has a history of intermittent episodes of abdominal pain. An esophagogastroduodenoscopy (EGD) is negative. She undergoes a small bowel follow-through (SBFT). What description best fits the findings?

A. Small bowel folds are nodular and irregularly thickened.
B. Small bowel folds are thickened and closely spaced.
C. Small bowel folds are thin and widely spaced.
D. Small bowel folds are normal in thickness.
20b Which of the following is the most likely cause?
A. Intramural hemorrhage
B. Crohn disease
C. Eosinophilic enteritis
D. Progressive systemic sclerosis
A. Herniation
B. Adhesions
C. Congenital bands
D. Peritoneal mass
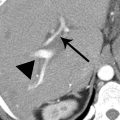
22 A 54-year-old male develops abdominal pain after a prolonged period of hypotension, and a CT is obtained. What finding raises the concern for mesenteric ischemia?


A. Pneumatosis intestinalis
B. Pneumobilia
C. Pneumoperitoneum
D. Pneumoretroperitoneum
23a A 65-year-old female presents with intermittent right upper quadrant colicky pain, nausea, vomiting, and abdominal distension. A CT scan is performed. What is the most likely diagnosis?



A. Adynamic ileus
B. Bezoar-induced small bowel obstruction
C. Small bowel intussusception
D. Gallstone ileus
23b Which of the following findings is not illustrated in the images shown but is still likely to be present?
A. A distal ileal stricture
B. A biliary enteric fistula
C. A mesenteric arterial thrombus
D. A distal ileal mass
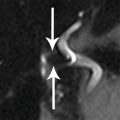
24a A 48-year-old male underwent a CT scan after a motor vehicle collision. The incidental abnormality indicated by the arrows occurs via


A. The fossa of Landzert
B. The fossa of Waldeyer
C. The foramen of Winslow
D. The mesocolic window
24b Right paraduodenal hernias account for what percentage of all paraduodenal hernias?
A. 25
B. 50
C. 75
D. 90
25 A patient who was a restrained passenger in an MVA has the following CT scan. Which of the following statements is most likely TRUE?


A. In blunt trauma, duodenal injuries are commonly associated with other organ injury.
B. Duodenal injuries are usually clinically apparent immediately.
C. Water-soluble contrast duodenography may help establish the diagnosis of duodenal injury if CT is equivocal.
D. Duodenal intramural hematoma requires urgent surgical repair.
26 A 90-year-old female developed nausea and vomiting 2 days after lifting a heavy box. On examination, she has a tender palpable mass in her right inguinal region. A CT scan is obtained. What is the diagnosis? (FV = femoral vein; IEV = inferior epigastric vessels; H = loop extending into hernia)



A. Indirect inguinal hernia
B. Direct inguinal hernia
C. Spigelian hernia
D. Femoral hernia
27 A 53-year-old female with a history of a Whipple procedure for pancreatic cancer presents at routine follow-up visit 2 years later with nausea, mild upper abdominal pain, and an elevated bilirubin and alkaline phosphatase. Her Ca 19-9 is normal. What is the likely diagnosis?




A. Hepaticojejunostomy stricture
B. Contained bile leak
C. Afferent limb syndrome
D. Pancreatitis with pseudocyst
28 A 64-year-old male presents with a bloody stools and a hematocrit of 22. He has no prior surgical history. He undergoes a CT of the abdomen and pelvis. What possible bleeding source is suggested by the findings?



A. Aortoenteric fistula
B. Gastrointestinal stromal tumor
C. Jejunal vascular malformation
D. Small bowel lymphoma
29 A 39-year-old female with a history of Roux-en-Y gastric bypass surgery presents with increasing abdominal pain. A CT scan was performed, and coronal reformatted images were generated. What finding is demonstrated?


A. Small bowel obstruction with dilated alimentary/Roux limb
B. Small bowel obstruction with dilated biliopancreatic limb
C. Small bowel obstruction with dilated common enteric channel
D. Adynamic ileus
30 A 45-year-old female with a history of diarrhea undergoes a barium small bowel examination with the findings below. Which of the following statements is TRUE?

A. The findings are congenital and more commonly present in the pediatric population.
B. Treatment involves surgical resection of the involved segments.
C. CT would have been a better initial examination if this entity was suspected clinically.
D. This finding can be associated with malabsorption, bowel perforation, obstruction, or GI bleeding.
31 What is the entrance exposure limit for standard operation of a fluoroscope?
A. 1 R/min
B. 5 R/min
C. 10 R/min
D. 20 R/min
32 A 17-year-old female with a history of cramping abdominal pain undergoes a small bowel follow-through. A spot film of the ileocecal region is taken. What is the most likely diagnosis?

A. Crohn disease
B. Lymphoid nodular hyperplasia
C. Non-Hodgkin lymphoma
D. Carcinoid
33 Which of the following maneuvers will decrease the patient dose during fluoroscopy?
A. Increasing the distance of the image intensifier from the patient
B. Removing the grid
C. Increasing the pulse rate using pulsed fluoroscopy
D. Selecting a lower kilovolt peak
34 A 45-year-old female presents for the evaluation of chronic abdominal pain, which she states has been waxing and waning for 10 to 15 years and is exacerbated by meals. A small bowel follow-through was obtained. What finding is demonstrated?

Early

Later
A. Small bowel obstruction
B. Intestinal malrotation
C. Increased number of small bowel folds
D. Multiple tiny colonic polyps
35 A 45-year-old female presents with cough, constipation, and substernal chest pain. A barium upper GI and small bowel follow-through is performed. What is the best diagnosis?


A. Gastroesophageal reflux
B. Gastric and small bowel ileus
C. Small bowel obstruction
D. Scleroderma
36 Reduction of the frame rate using pulsed fluoroscopy from 30 frames per second to 15 frames per second
A. Results in no dosage change
B. Reduces the dosage by about 25%
C. Reduces the dosage by about 50%
D. Increases the dosage by about 50%
37a A 57-year-old male presented with GI bleeding. Upper endoscopy was negative, and colonoscopy demonstrated a pool of blood in the ileum without a clear source. A technetium-99m red blood cell (99mTc RBC) scan followed by a CT enteroclysis is performed. What is the most likely diagnosis?





A. Gut duplication cyst with perforation
B. Meckel diverticulum with active bleeding
C. Crohn disease with abscess
D. Appendiceal mucocele with pseudomyxoma peritonei
37b What other anomaly may arise from the same embryologic origin as a Meckel diverticulum?
A. Vitelline duct cyst
B. Single umbilical artery
C. Urachal cyst
D. Unicornuate uterus
38 A 24-year-old female with a history of anorexia nervosa presents with abdominal pain and vomiting. A CT scan is obtained. What anatomic factors may be responsible for these findings?




A. Presence of a median arcuate ligament
B. Narrowed angle between the superior mesenteric artery and aorta
C. Abnormal position of the ligament of Treitz
D. Retroaortic location of the left renal vein
39a Early transient erythema is encountered at what approximate threshold dose?
A. 0.2 Gy
B. 2 Gy
C. 20 Gy
D. 200 Gy
39b For a patient of average build, at what approximate duration of fluoroscopy time does erythematous skin change become a risk?
A. 5 minutes
B. 20 minutes
C. 1 hour
D. 2 hours
40 A 29-year-old female presents with a progressive history of radiating back pain, nausea, and vomiting. Currently, the patient is only able to eat yogurt and juice consistencies. An upper GI procedure was performed. What is the best diagnosis?

A. Duodenal carcinoma
B. Duodenal polyp
C. Duodenal ulcer
D. Duodenal intraluminal diverticulum
ANSWERS AND EXPLANATIONS
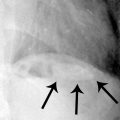
1 Answer D.The small bowel follow-through (SBFT) demonstrates findings of long segmental strictures in the ileum with pseudosacculations consistent with Crohn disease. The inflammation leads to fibrofatty proliferation causing asymmetric straightening and shortening along the mesenteric side of the bowel, with the uninvolved wall along the antimesenteric side forming redundant saccules. The skip involvement is typical of Crohn disease. Narrowing of the lumen may be due to a combination of spasm, which may not cause significant upstream obstruction, or fibrosis and proliferation of smooth muscle, which is associated with upstream dilatation.
Jejunal diverticulosis does not involve luminal narrowing as seen in this case. Small bowel ischemia may resemble acute Crohn disease with smooth fold thickening, but in this case, the folds are effaced due to marked wall thickening. Carcinoid can cause a mesenteric shortening similar to Crohn disease, but the luminal narrowing would not result in the long strictures seen in this case and would be fixed, leading to a greater degree of obstructions.
The SBFT demonstrates the findings of Crohn enteritis with excellent mucosal detail and is superior to cross-sectional imaging for the evaluation of early disease. Real-time fluoroscopic observation can distinguish between strictures and segments of peristalsis. It is limited in its ability to evaluate extraintestinal manifestations of disease and is not ideal for frequent follow-up due to radiation dosage concerns.
References: Boland G. Gastrointestinal imaging: the requisites. Philadelphia, PA: Elsevier, 2014.
Gore RM, Levine MS. Textbook of gastrointestinal radiology, 4th ed. Philadelphia, PA: Elsevier/Saunders, 2015.
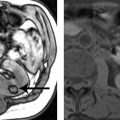
2 Answer A.A long segment of ileum demonstrates wall thickening, T2-hyperintense mural signal, restricted diffusion, and mucosal enhancement. These findings are highly suggestive of active Crohn disease, as compared to chronic disease. Note that some enhancement may be seen with fibrotic disease, but the intensity tends to be less than with active disease. Additional findings of active disease not shown in this case include mesenteric vascular engorgement (comb sign), prominent enhancing regional mesenteric lymphadenopathy, mucosal ulcerations, and fistulous disease.
With effective treatments available for Crohn disease, the goal is to develop a treat-to-target strategy that will alter the natural history of the disease and prevent irreversible fibrostenotic lesions as well as the penetrating extraintestinal complications.
Small bowel lymphoma demonstrates aneurysmal dilatation of bowel loop along with regional lymphadenopathy and would not typically show preferential mucosal enhancement. The patient’s chronic symptomatology does not suggest acute gastroenteritis.
References: Bruining DH, Bhatnagar G, Rimola J, et al. CT and MR enterography in Crohn’s disease: current and future applications. Abdom Imaging 2015;40(5):965–974.
Griffin N, Grant LA, Anderson S, et al. Small bowel MR enterography: problem solving in Crohn’s disease. Insights Imaging 2012;3(3):251–263.
3 Answer D.The CT demonstrates mild uniform circumferential wall thickening of the terminal ileum. The colon is not fully distended, but the cecum and ascending colon also demonstrate mild wall thickening. There is a small amount of free fluid present.
The appendix is not shown, but the abnormality involves the ileum and the ascending colon and is not concentrated at the cecal tip. The wall thickening is regular and mild, not mass-like, and therefore unlikely to be neoplastic. Adenocarcinoma of the ileum is annular and constricting, and the lumen is normal in this case.
With the relatively mild wall thickening (<1 cm), an infectious or inflammatory etiology is most likely. Crohn disease (not included in the options) could have this appearance. Infections involving the ileum and right colon are usually caused by Yersinia (as in this case), Campylobacter, or Salmonella species. Tuberculous infection also involves this area and may mimic Crohn disease. With infectious ileocecitis, lymphadenopathy (not shown in this case) is commonly present.
Reference: Hoeffel C, Crema MD, Belkacem A, et al. Multi-detector row CT: spectrum of diseases involving the ileocecal area. Radiographics 2006;26(5):1373–1390.
4 Answers:
1. Answer B.Given the patient’s fever and leukocytosis, concern is raised for extraluminal extension of disease. CT is widely available and the scan time minimal, which is helpful for a patient in significant pain. The examination may be performed as a CT enterography study with an attempt at maximizing bowel distention for optimal wall analysis. If the patient is too ill to tolerate the oral contrast, a standard CT with intravenous contrast will still be sufficient to assess the extraintestinal tissues for complications such as an abscess or fistula.
2. Answer A.Given the patient’s age and probable need for future recurrent imaging, radiation doses should be minimized. MR enterography involves no ionizing radiation and will be able to assess the bowel wall for thickening and enhancement, evaluate the degree of bowel dilatation in the setting of known strictures, and image the extraintestinal tissues.
3. Answer B.The patient’s history raises question of an enterovesical or colovesical fistula. Given her history of a hysterectomy, small bowel loops may be crowded in the pelvis and difficult to separate on a barium small bowel follow-through. Cross-sectional imaging is more appropriate, and given the superior spatial resolution of CT over MR, the CT enterography or conventional CT would be the ideal choice.
4. Answer C.With the findings suspicious for early Crohn disease, investigation of the more proximal small bowel to determine extent of involvement is indicated. Cross-sectional imaging with either CT or MR is insensitive for the evaluation of early disease. The small bowel follow-through is more sensitive for early changes such as aphthae or erosions. A capsule endoscopy will also detect early changes of Crohn but probably should not be attempted as an initial small bowel study in a patient with potential stricturing disease. In one small study, 15% of patients with suspected Crohn disease retained the capsule.
References: Bruining DH, Bhatnagar G, Rimola J, et al. CT and MR enterography in Crohn’s disease: current and future applications. Abdom Imaging 2015;40(5):965–974.
Lee NM, Eisen GM. 10 years of capsule endoscopy: an update. Expert Rev Gastroenterol Hepatol 2010;4(4):503–512.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree