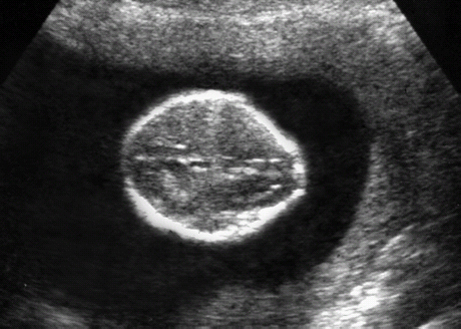
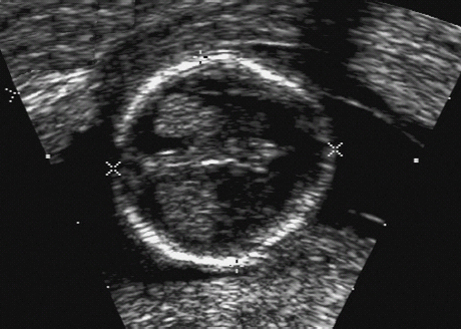
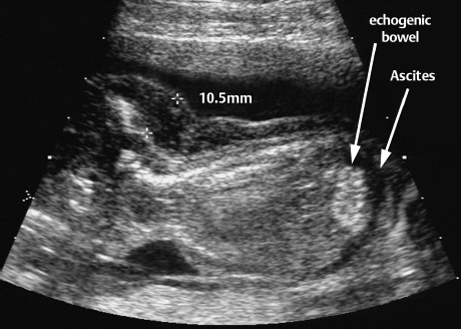
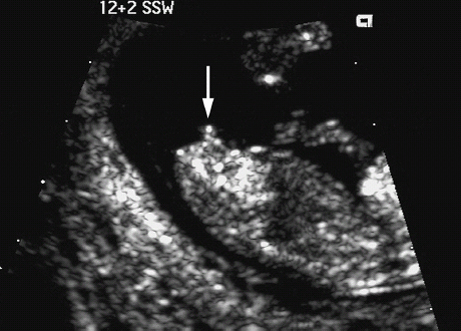
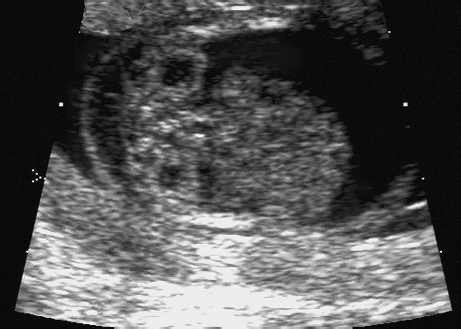
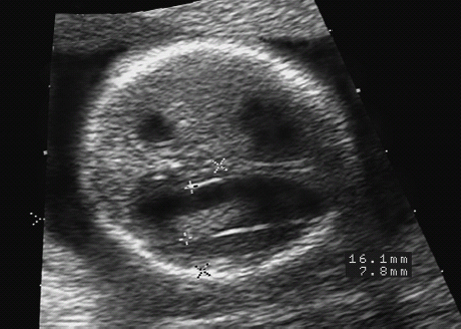
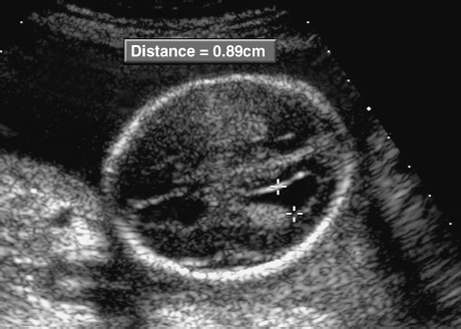
10 Soft Markers of Chromosomal Aberrations Definition: Brachycephaly: the head ratio (biparietal diameter/frontal occipital diameter, BPD/FOD) is above the 95th percentile; for example, head ratio >0.88, depending on the method of measurement. Incidence: As defined above, this applies to about 5% of all fetuses. Ultrasound findings: The horizontal cross-section shows a round shape, with the BPD being relatively large compared to the FOD. Fig. 10.1 Strawberry sign, in a case of trisomy 18at 19+1 weeks. Fig. 10.2 Brachycephaly. Rounded head at 14 + 1 weeks in trisomy 13. References Becker R, Brinnef C, Arabin B. Der Kopfindex—ein vernachlässigter Parameter der fetalen Standardbiometrie. Ultraschall Med 1992; 13: 2–6. Borrell A, Costa D, Martinez JM, et al. Brachycephaly is ineffective for detection of Down syndrome in early midtrimester fetuses. Early Hum Dev 1997; 4: 57–61. Buttery B. Occipitofrontal-biparietal diameter ratio: an ultrasonic parameter for the antenatal evaluation of Down’s syndrome. Med J Aust 1979; 2: 662–4. Stempfle N, Huten Y, Fredouille C, Brisse H, Nessmann C. Skeletal abnormalities in fetuses with Down’s syndrome: a radiographic post-mortem study. Pediatr Radiol 1999; 29: 682–8. Definition: A connection between the fourth ventricle and the cisterna magna is a normal finding up to 18 weeks of gestation; thereafter, this diagnosis is applicable. It is advisable to determine the chromosome set, as an association with a chromosomal disorder is frequent. Detailed ultrasound screening should also be carried out to detect other malformations. The boundary to Dandy–Walker syndrome is hazy. Associated syndromes: Smith–Lemli–Opitz syndrome, Joubert syndrome, Meckel–Gruber syndrome, Neu–Laxova syndrome, Walker–Warburg syndrome, Ellis–van Creveld syndrome, Majewski syndrome, TAR syndrome, tetrasomy 12 p, triploidy, trisomy 9, trisomy 18, arthrogryposis, CHARGE association, Fryns syndrome, MURCS association. Ultrasound findings: A small, slit-like connection is detected between the fourth ventricle and the cisterna magna, without widening of the latter. This finding distinguishes the Dandy–Walker variant from the Dandy–Walker syndrome. False–positive as well as false-negative findings can be produced by inaccurate ultrasound scanning in the wrong plane. Caution: At 13 weeks of gestation, Dandy–Walker variant is almost always detectable, and is considered to be a normal finding up to 18 weeks. Prognosis: This may be a harmless finding with a good prognosis, or may be associated with other syndromes with a poor prognosis. References Blaicher W, Ulm B, Ulm MR, Hengstschlager M, Deutinger J, Bernaschek G. Dandy–Walker malformation as sonographic marker for fetal triploidy. Ultraschall Med 2002; 23: 129–33 Bromley B, Nadel AS, Pauker S, Estroff JA, Benacerraf BR. Closure of the cerebellar vermis: evaluation with second trimester US. Radiology 1994; 193: 761–3 Ecker JL, Shipp TD, Bromley B, Benacerraf B. The sonographic diagnosis of Dandy–Walker and Dandy–Walker variant: associated findings and outcomes. Prenat Diagn 2000; 20: 328–32. Laing FC, Frates MC, Brown DL, Benson CB, Di Salvo DN, Doubilet PM. Sonography of the fetal posterior fossa: false appearance of mega-cisterna magna and Dandy–Walker variant. Radiology 1994; 192: 247–51. Definition: Increased echogenicity of the bowel in the second trimester, such that it is equal to that of surrounding fetal bone. The most frequent cause is intra-amniotic bleeding. The echogenicity is a soft marker for chromosomal anomaly, especially for Down syndrome. In the third trimester, bowel containing echogenic meconium is a normal finding. Incidence: 0.6% of all fetuses in the second trimester. Ultrasound findings: Loops of the bowel show a strong echogenic content. Weak echo can be excluded by reducing the overall density of the ultrasound picture. At the lowest level of reduction, only the bones and the echogenic bowel can be demonstrated if their echogenicity is similar. Differential diagnosis: The differential diagnosis in these findings can be clarified from the study by Yaron et al., who investigated 79 cases of echogenic bowel. No cause was found in 30 cases (38%); intra-amniotic bleeding was the cause in 19% (n = 15); other anomalies were associated in 8% (n = 7); seven fetuses were affected in multiple pregnancies; and five (6.3%) showed bowel obstruction without cystic fibrosis. Chromosomal aberrations were found in five cases, and in a further five cases, intrauterine infection was the cause. Cystic fibrosis was diagnosed in only two cases (2.5%). Three fetuses (3.8%) were stillborn without any obvious cause. Hogge et al. reported two cases of cystic fibrosis in four detected cases. Fig. 10.3 Echogenic bowel. The scan shows echogenic bowel as well as ascites and hygroma colli in a fetus with trisomy 21. Fig. 10.4 Echogenic bowel. Longitudinal section of a male fetus (arrow: penis) at 12 + 2 weeks. Fig. 10.5 Echogenic bowel. Fetus at 17 + 2 weeks. Clinical management: Further ultrasound screening, including fetal echocardiography, karyotyping, TORCH serology, exclusion of cystic fibrosis (frequency 2–3%). Pregnancy should be followed up closely, using Doppler monitoring, as there is a high risk of stillbirth. Prognosis: Benacerraf found Down syndrome in 16% of cases of echogenic bowel; the findings were isolated, with no other anomaly, in only 1.4% of cases of echogenic bowel. Sipes et al. observed spontaneous disappearance of echogenic bowel in five of seven cases during the course of pregnancy; in the other two cases, the infants did not show any anomalies after birth. Nicolaides reports that there is a fivefold increase in the incidence of Down syndrome in fetuses with echogenic bowel. References Al-Kouatly HB, Chasen ST, Streltzoff J, Chervenak FA. The clinical significance of fetal echogenic bowel. Am J Obstet Gynecol 2001; 185: 1035–8. Dunne M, Haney P, Sun CC. Sonographic features of bowel perforation and calcific meconium peritonitis in utero. Pediatr Radiol 1983; 13: 231–3. Font GE, Solari M. Prenatal diagnosis of bowel obstruction initially manifested as isolated hyperechoic bowel. J Ultrasound Med 1998; 17: 721–3. Hogge WA, Hogge JS, Boehm CD, Sanders RC. Increased echogenicity in the fetal abdomen: use of DNA analysis to establish a diagnosis of cystic fibrosis. J Ultrasound Med 1993; 12: 451–4. Nyberg DA, Souter VL, El-Bastawissi A, Young S, Luthhardt F, Luthy DA. Isolated sonographic markers for detection of fetal Down syndrome in the second trimester of pregnancy. J Ultrasound Med 2001; 20: 1053–63. Sipes SL, Weiner CP, Wenstrom KD, Williamson RA, Grant SS, Mueller GM. Fetal echogenic bowel on ultrasound: is there clinical significance? Fetal Diagn Ther 1994; 9: 38–43. Smith-Bindman R, Hosmer W, Feldstein VA, Deeks JJ, Goldberg JD. Second-trimester ultrasound to detect fetuses with Down syndrome: a meta-analysis. JAMA 2001; 285: 1044–55. Souter VL, Nyberg DA, El-Bastawissi A, Zebelman A, Luthhardt F, Luthy DA. Correlation of ultrasound findings and biochemical markers in the second trimester of pregnancy in fetuses with trisomy 21. Prenat Diagn 2002; 22: 175–82. Yaron Y, Hassan S, Geva E, Kupferminc MJ, Yavetz H, Evans MI. Evaluation of fetal echogenic bowel in the second trimester. Fetal Diagn Ther 1999; 14: 176–80. Definition and clinical significance: The kidneys are more echogenic than the liver. This may be a normal finding, or may be the first sign of nephrotic syndrome or other renal anomalies. A case associated with cytomegalovirus infection has been reported. Benacerraf published 19 cases, in which there was a normal postnatal outcome in only four (21 %). Five (26%) died and had either infantile polycystic kidneys or multicystic renal dysplasia. In two cases, oligohydramnios only developed after 24 weeks; in one case, partial trisomy 10 was found. Associated syndromes: Infantile polycystic kidneys, Meckel–Gruber syndrome, trisomy 13, Perlman syndrome, cystic renal dysplasia, Beck-with–Wiedemann syndrome. Ultrasound findings: The volume of the kidneys is increased (above the 95th percentile), with a high echogenicity. If the renal function is affected, oligohydramnios or anhydramnios are found and the bladder is hardly filled. In some cases, oligohydramnios may even be detected at 15 weeks. Prognosis: The decisive prognostic criterion is renal function, determined by the extent of amniotic fluid. Cases of severe oligohydramnios have a poor outcome. References Carr MC, Benacerraf BR, Estroff JA, Mandell J. Prenatally diagnosed bilateral hyperechoic kidneys with normal amniotic fluid: postnatal outcome. J Urol 1995; 153: 442–4. Choong KK, Gruenewald SM, Hodson EM. Echogenic fetal kidneys in cytomegalovirus infection. J Clin Ultrasound 1993; 21: 128–32. Lilford RJ, Irving HC, Allibone EB. A tale of two prior probabilities: avoiding the false positive antenatal diagnosis of autosomal-recessive polycystic kidney disease. Br J Obstet Gynaecol 1992; 99: 216–9. Nyberg DA, Hallesy D, Mahony BS, Hirsch JH, Luthy DA, Hickok D. Meckel–Gruber syndrome: importance of prenatal diagnosis. J Ultrasound Med 1990; 9: 691–6. Vintzileos AM, Egan JF. Adjusting the risk for trisomy 21 on the basis of second-trimester ultrasonography [review]. Am J Obstet Gynecol 1995; 172: 837–44. Wisser J, Hebisch G, Froster U, et al. Prenatal sonographic diagnosis of autosomal-recessive polycystic kidney disease (ARPKD) during the early second trimester. Prenat Diagn 1995; 15: 868–71. Fig. 10.6 Echogenic kidneys. Dilation of the renal pelvis and fetal ascites in a fetus with trisomy 9. Definition: The upper limit of the width of the posterior horn of lateral cerebral ventricle lies at 8–10 mm. Dilation of the posterior horn above 10 mm is definitely a pathological finding. Mild ventriculomegaly is regarded as a soft marker for chromosomal aberrations. It may be a harmless finding, or may be the earliest sign of a developing hydrocephalus. Ultrasound findings: The posterior horns of the lateral ventricles (the first and second ventricles) can be well detected and measured behind the choroid plexus. As defined above, one differentiates between the marginal form (8–10 mm) and pathological form (>10 mm) of ventriculomegaly. Asymmetrical dilation of the ventricles is a common finding. On scanning, the ventricle lying nearest to the transducer is difficult to measure, due to loss of scanning intensity immediately behind the skull bone. However, by changing the plane of the transducer and thus altering the angle, it is almost always possible to demonstrate it, especially in the second trimester. Fig. 10.7 Mild ventriculomegaly. Marginal dilation of the cerebral ventricles: 7.8 mm at 15 +6 weeks, in a fetus with trisomy 13. Fig. 10.8 Mild ventriculomegaly. The width of the posterior horn of the left lateral ventricle is 8.9 mm, without pathology. Clinical management: Further ultrasound screening, including fetal echocardiography, TORCH serology (especially cytomegalovirus infection, toxoplasmoses). Karyotyping should be offered. Procedure after birth: The finding should be confirmed by transfontanelle scanning of the neonate’s skull. The plane of measurement used in prenatal scanning is not always reproducible after birth, so that confirmation of the diagnosis after birth is often difficult. Prognosis:
Abnormal Shape of the Head
Dandy–Walker Variant (Open Cerebellar Vermis)
Echogenic Bowel

Echogenic Kidneys
Mild Ventriculomegaly
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree