Soft Tissue and Musculoskeletal Procedures
Andrew J. French
Joy English
Michael B. Stone
Bradley W. Frazee
INTRODUCTION
As ultrasound has been universally adopted in the practice of emergency medicine, its tremendous value in providing procedural guidance has increasingly been recognized. Ultrasound guidance has been shown to improve the speed, accuracy, and safety of many common procedures in the emergency department (ED). The improved image quality of newer ultrasound systems has contributed to the burgeoning list of procedures benefiting from ultrasound guidance, including many musculoskeletal and soft tissue applications.
PERIPHERAL NERVE BLOCKS
Clinical Applications
Peripheral nerve blocks have long been utilized for analgesia and anesthesia for invasive procedures and pain control after acute trauma (1,2). While regional anesthesia has traditionally been performed by a landmark approach with the assistance of nerve stimulation, the use of ultrasoundguidance provides multiple additional benefits to peripheral nerve blocks. A Cochrane review highlighted the following advantages of ultrasound-guided blocks compared to nonultrasound techniques (3):
Decreased rate of vascular puncture
Improved quality of both motor and sensory blocks
Faster time to onset nerve blockade
Decreased procedural time
Significantly lower volume of required anesthetic
Other studies have shown that the use of ultrasound decreases the number of needle passes, lowers the rate of block failure, and increases the duration of the block compared to nonultrasound techniques (4, 5, 6). Ultrasound guided nerve blocks have many applications in the ED, including pain relief from fractures and dislocations, and facilitation of procedures such as abscess drainage and closed reductions (7).
Image Acquisition
Due to the small size and relatively superficial nature of peripheral nerves, a high-frequency linear array transducer should be used for identification and block guidance. A nerve preset should be utilized when available, with a frequency in the 14 to 10 MHz range. Patient positioning and preparation will vary depending on the particular block.
Anatomy and Landmarks
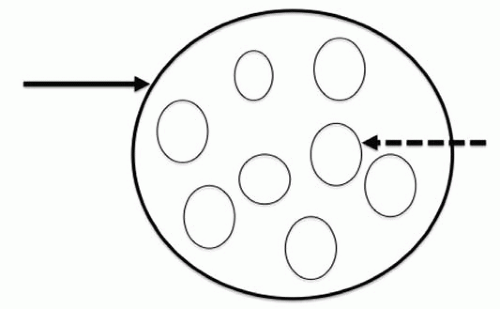
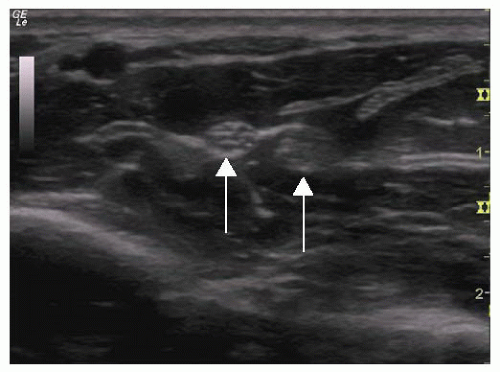
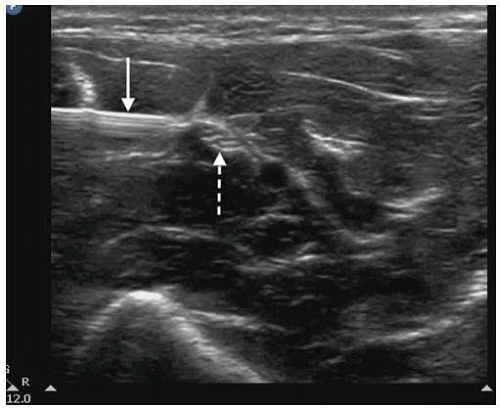
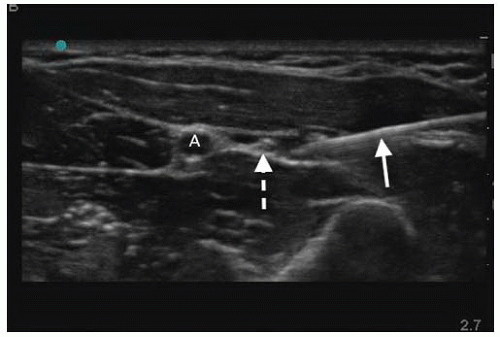
In the short axis, peripheral nerves appear as oval or round structures with a hyperechoic epineurium and internal hypoechoic fascicles, which are encased in perineurium (Fig. 22.1). In general, large peripheral nerves above the clavicles have a predominantly hypoechoic appearance, and nerves below the clavicles are predominantly hyperechoic with small internal hypoechoic fascicles. Most nerves targeted for blocks are relatively superficial (<3 cm deep to skin) and are also often adjacent to a vascular structure. Diameter may vary from subcentimeter in larger nerves such as the femoral nerve to millimeters as with the radial nerve. Nerves may appear similar to tendons; however, tendons are internally brighter, move with range of motion, and will typically transition into muscle as they are scanned more proximally (Fig. 22.2;  VIDEO 22.1).
VIDEO 22.1).
 VIDEO 22.1).
VIDEO 22.1).General Approach to Nerve Blocks
Patient preparation
Prior to beginning any nerve block, it is recommended that a detailed motor and sensory exam be documented for the affected extremity for multiple reasons. Injured nerves may be prone to increased complications of regional anesthesia, and a thorough exam will insure that any pre-existing deficits are not falsely attributed to the block post recovery.
Patient and operator positioning
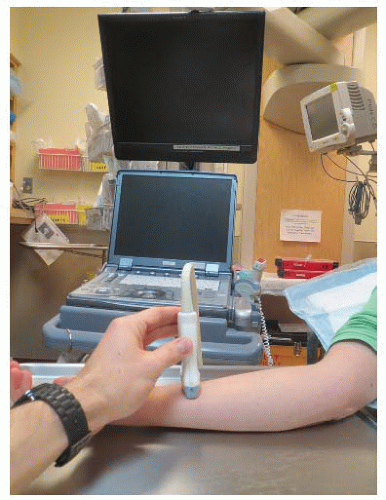
Patient positioning depends on the type of block being performed. The ultrasound should be placed so that the screen is in the operator’s direct line of vision, which may necessitate placing the machine on the opposite side of the procedure site (Fig. 22.3). A survey scan both proximal and distal to the anticipated site of needle insertion will allow the operator to determine the optimal location for the procedure by helping to identify the site with the clearest image of the nerve without adjacent vasculature.
Equipment selection
The next step in preparing for a nerve block includes selection of needles, anesthetic, and skin sterilizing solution. Equipment may vary depending on the type and indication of block.
Needle size
Sizes may range from 21 to 27 gauge needles (7, 8, 9). The size and location of the nerve may affect the gauge selection. A larger needle may be beneficial for a deeper nerve block, as its size may improve visualization at steeper entry angles. A smaller peripheral nerve is often best anesthetized with a smaller needle as the entry angle is typically shallower and its size may facilitate fine adjustments in needle tip placement. Although larger needles are typically easier
to visualize under ultrasound guidance, histologic examination reveals that smaller needles produce less nerve injury in cases of nerve penetration (10). Needle tip has also shown to play a histologic role in direct nerve trauma. Fascicular trauma is minimized with shorter beveled cutting needles (11,12). However long tapered (pencil-tip) needles have also shown to minimize the number of transected nerve fibers compared to cutting needles (13). The last consideration in needle selection concerns the use of echogenic needles. While the literature supports increased sonographic visualization of echogenic needles, no study has yet identified a clear benefit in safety or efficacy of echogenic needles in peripheral nerve blockade (14, 15, 16).
to visualize under ultrasound guidance, histologic examination reveals that smaller needles produce less nerve injury in cases of nerve penetration (10). Needle tip has also shown to play a histologic role in direct nerve trauma. Fascicular trauma is minimized with shorter beveled cutting needles (11,12). However long tapered (pencil-tip) needles have also shown to minimize the number of transected nerve fibers compared to cutting needles (13). The last consideration in needle selection concerns the use of echogenic needles. While the literature supports increased sonographic visualization of echogenic needles, no study has yet identified a clear benefit in safety or efficacy of echogenic needles in peripheral nerve blockade (14, 15, 16).
Anesthetic
Operators should choose an anesthetic agent based on the preferred duration of anesthesia. Bupivacaine is the most commonly used long-acting amide anesthetic, yet is significantly more cardiotoxic than lidocaine. As a result, if procedures can be adequately accomplished with lidocaine alone, it is our recommendation to avoid bupivacaine use until sufficiently experienced with these techniques.
Additional considerations with regard to anesthetic volume must be taken into account. Table 22.1 shows common anesthetics and maximum doses. In peripheral nerve blocks, volume is an important issue as it relates to block effect and duration, as well as patient safety. While multiple studies have examined the minimum volume necessary for a given block, it is difficult to generalize the results as the concentrations and anesthetic additives may vary (17, 18, 19, 20). The primary goal of the block should be to circumferentially surround the nerve with a volume of anesthetic, which does not exceed the mg/kg dose for the patient. One small study demonstrated that lower volumes of an equivalent concentration of anesthetic primarily decrease block duration without altering efficacy; therefore, increasing volume may help prolong block duration, but not change the degree of anesthesia (21).
Sterile barrier
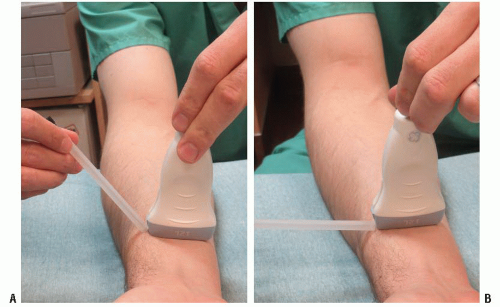
While some anesthesia literature describes most peripheral nerve blocks as a sterile practice, this is often in the setting of an operative procedure and/or placement of a nerve block catheter. Alternative descriptions include skin prep with betadine or chlorohexadine with sterile gel and a sterile adhesive dressing covering over the ultrasound probe (Fig. 22.4) (7,8,22). Still others only describe skin prep without specific gel or probe covers (8). From a practical standpoint, if the needle is visualized throughout its entire track from skin to nerve, ideally, only penetration of subcutaneous and muscular tissue will occur. Therefore, while skin prep is still necessary, the procedure should not be significantly different than any other intramuscular or subcutaneous injection provided that the needle does not pass directly through nonsterile ultrasound gel prior to skin penetration.
TABLE 22.1 Common Anesthetics and Maximum Dosing | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||
Technique
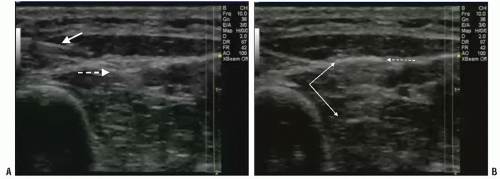
Performance of the block is often done using an in-plane technique wherein the needle is advanced in parallel to the long axis of the probe, while the nerve is imaged in the short axis (Fig. 22.5). A short axis view of the nerve provides the best view for circumferential deposition of anesthetic while viewing the surrounding structures and layers of the nerve bundle. Some practitioners favor an out-of-plane technique in which the nerve remains imaged in the short axis but the needle is placed perpendicular to the long axis of the probe. There is no clear evidence suggesting a clear
advantage to either approach. The probe should be held in the nondominant hand, with the needle and syringe held in the dominant hand, allowing finer control of the anesthetic. Prior to inserting the needle into the skin, any air remaining in the syringe or needle tip should be expelled, as inadvertent injection of air into the tissue will cause scatter artifact, making it difficult to visualize both needle and tissue anatomy (Fig. 22.6; VIDEO 22.2). As the needle is advanced, anesthetizing the tract to the nerve can help visualize the needle by decreasing the attenuation coefficient of the tissue. It is imperative that anesthetic should not be injected around the nerve or into tissue unless the needle tip is visualized. This is an essential step to decrease the risk of intravascular and intrafascicular injection. Minimizing the angle of the needle entry in relation to the probe will increase needle visualization by bringing it into a more perpendicular orientation to the ultrasound beam (Fig. 22.7). Once the needle tip is clearly visualized with the nerve in short axis, anesthetic should be deposited circumferentially around the nerve to ensure a complete block. It is important to note that due to the depth and location of surrounding structures, circumferential deposition of anesthetic may require needle redirection or more than one needle pass.
VIDEO 22.2). As the needle is advanced, anesthetizing the tract to the nerve can help visualize the needle by decreasing the attenuation coefficient of the tissue. It is imperative that anesthetic should not be injected around the nerve or into tissue unless the needle tip is visualized. This is an essential step to decrease the risk of intravascular and intrafascicular injection. Minimizing the angle of the needle entry in relation to the probe will increase needle visualization by bringing it into a more perpendicular orientation to the ultrasound beam (Fig. 22.7). Once the needle tip is clearly visualized with the nerve in short axis, anesthetic should be deposited circumferentially around the nerve to ensure a complete block. It is important to note that due to the depth and location of surrounding structures, circumferential deposition of anesthetic may require needle redirection or more than one needle pass.
advantage to either approach. The probe should be held in the nondominant hand, with the needle and syringe held in the dominant hand, allowing finer control of the anesthetic. Prior to inserting the needle into the skin, any air remaining in the syringe or needle tip should be expelled, as inadvertent injection of air into the tissue will cause scatter artifact, making it difficult to visualize both needle and tissue anatomy (Fig. 22.6;
 VIDEO 22.2). As the needle is advanced, anesthetizing the tract to the nerve can help visualize the needle by decreasing the attenuation coefficient of the tissue. It is imperative that anesthetic should not be injected around the nerve or into tissue unless the needle tip is visualized. This is an essential step to decrease the risk of intravascular and intrafascicular injection. Minimizing the angle of the needle entry in relation to the probe will increase needle visualization by bringing it into a more perpendicular orientation to the ultrasound beam (Fig. 22.7). Once the needle tip is clearly visualized with the nerve in short axis, anesthetic should be deposited circumferentially around the nerve to ensure a complete block. It is important to note that due to the depth and location of surrounding structures, circumferential deposition of anesthetic may require needle redirection or more than one needle pass.
VIDEO 22.2). As the needle is advanced, anesthetizing the tract to the nerve can help visualize the needle by decreasing the attenuation coefficient of the tissue. It is imperative that anesthetic should not be injected around the nerve or into tissue unless the needle tip is visualized. This is an essential step to decrease the risk of intravascular and intrafascicular injection. Minimizing the angle of the needle entry in relation to the probe will increase needle visualization by bringing it into a more perpendicular orientation to the ultrasound beam (Fig. 22.7). Once the needle tip is clearly visualized with the nerve in short axis, anesthetic should be deposited circumferentially around the nerve to ensure a complete block. It is important to note that due to the depth and location of surrounding structures, circumferential deposition of anesthetic may require needle redirection or more than one needle pass.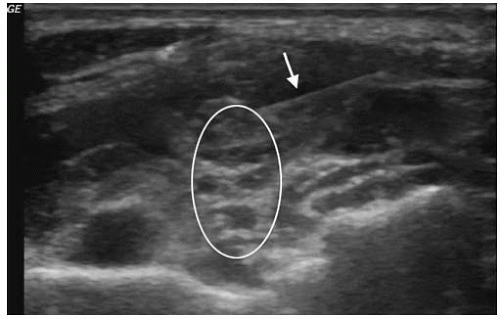 FIGURE 22.5. The Needle (Arrow) is Advanced in the Longitudinal Plane Toward the Nerve (Oval Arrow) that is Imaged in the Transverse Plane. |
Perineural (around the nerve), intraneural (within the epineurium), and intrafasicular (within the perineurium) are all sonographically visible sites and have anatomic relevance in nerve blocks. A perineural block wherein the anesthetic is placed completely outside of the epineurium is generally the most accepted location of block with minimal risk of nerve injury (Fig. 22.8;  VIDEO 22.3). Although an intraneural injection is considered unfavorable, there is little evidence to support this opinion (23). Multiple studies have
VIDEO 22.3). Although an intraneural injection is considered unfavorable, there is little evidence to support this opinion (23). Multiple studies have
demonstrated that intentional and unintentional intraneural injections do not result in neurologic dysfunction after a normal recovery period (24). In some cases, intraneural injection has actually shown to be favorable in block onset time (Fig. 22.9; VIDEO 22.4) (12). In contrast, intrafascicular blocks are considered harmful and must be avoided, as damage to fascicles may result in near immediate damage (25). Also, the site of peripheral nerve blockade may play a role in the risk of fascicular damage as it relates to the ratio of cross-sectional fascicle to epineurium (25). For example, the sciatic nerve at the popliteal fossa contains more non-neural tissue than fascicles, which may explain the relatively low incidence of post-block neuropathy (26). Alternatively, the brachial plexus trunks are characterized by a higher ratio of neural to connective tissue. Subsequently, an advancing needle is more likely to encounter fascicles, thereby potentially increasing the risk of injury (25). This again highlights the necessity to maintain visualization of the needle tip at all times during needle advancement.
VIDEO 22.4) (12). In contrast, intrafascicular blocks are considered harmful and must be avoided, as damage to fascicles may result in near immediate damage (25). Also, the site of peripheral nerve blockade may play a role in the risk of fascicular damage as it relates to the ratio of cross-sectional fascicle to epineurium (25). For example, the sciatic nerve at the popliteal fossa contains more non-neural tissue than fascicles, which may explain the relatively low incidence of post-block neuropathy (26). Alternatively, the brachial plexus trunks are characterized by a higher ratio of neural to connective tissue. Subsequently, an advancing needle is more likely to encounter fascicles, thereby potentially increasing the risk of injury (25). This again highlights the necessity to maintain visualization of the needle tip at all times during needle advancement.
 VIDEO 22.3). Although an intraneural injection is considered unfavorable, there is little evidence to support this opinion (23). Multiple studies have
VIDEO 22.3). Although an intraneural injection is considered unfavorable, there is little evidence to support this opinion (23). Multiple studies have demonstrated that intentional and unintentional intraneural injections do not result in neurologic dysfunction after a normal recovery period (24). In some cases, intraneural injection has actually shown to be favorable in block onset time (Fig. 22.9;
 VIDEO 22.4) (12). In contrast, intrafascicular blocks are considered harmful and must be avoided, as damage to fascicles may result in near immediate damage (25). Also, the site of peripheral nerve blockade may play a role in the risk of fascicular damage as it relates to the ratio of cross-sectional fascicle to epineurium (25). For example, the sciatic nerve at the popliteal fossa contains more non-neural tissue than fascicles, which may explain the relatively low incidence of post-block neuropathy (26). Alternatively, the brachial plexus trunks are characterized by a higher ratio of neural to connective tissue. Subsequently, an advancing needle is more likely to encounter fascicles, thereby potentially increasing the risk of injury (25). This again highlights the necessity to maintain visualization of the needle tip at all times during needle advancement.
VIDEO 22.4) (12). In contrast, intrafascicular blocks are considered harmful and must be avoided, as damage to fascicles may result in near immediate damage (25). Also, the site of peripheral nerve blockade may play a role in the risk of fascicular damage as it relates to the ratio of cross-sectional fascicle to epineurium (25). For example, the sciatic nerve at the popliteal fossa contains more non-neural tissue than fascicles, which may explain the relatively low incidence of post-block neuropathy (26). Alternatively, the brachial plexus trunks are characterized by a higher ratio of neural to connective tissue. Subsequently, an advancing needle is more likely to encounter fascicles, thereby potentially increasing the risk of injury (25). This again highlights the necessity to maintain visualization of the needle tip at all times during needle advancement.Pitfalls and Complications
The use of ultrasound in peripheral nerve blocks does not eliminate complications associated with regional anesthesia. A study of over 12,000 patients found that complications such as prolonged neurologic dysfunction, vascular puncture, and pneumothorax still occur with ultrasound. However, the incidence was not >0.2% (27). The root cause of complications with ultrasound-guided nerve blocks can be linked to three major categories: patient exam, real-time needle guidance, and sonographic anatomy.
Animal studies suggest that pre-existing nerve pathology puts patients at risk for prolonged duration of blocks and increased neurotoxicity of local anesthetics (28). Therefore, failure to perform a detailed neurologic exam focused on detection of neurologic deficits can lead to unanticipated but avoidable complications. A standardized approach to examination of motor and sensory function for upper and lower extremities is recommended prior to execution of any block.
The skill set required to safely perform an ultrasoundguided nerve block should not be underestimated. A cadaver study assessing needle guidance in peripheral nerve blockade demonstrated that a novice operator needs approximately 28 supervised trials with feedback to achieve competency (29). Therefore, proper training should be completed prior to unsupervised block performance.
Theoretically, vascular puncture, misplacement of anesthetic, fascicular trauma, and pneumothorax should not occur if the length of the needle tip is visualized throughout the entire procedure. Tissue distortion and movement are only indicators of needle location. Ultrasound provides two-dimensional imaging for a three-dimensional procedure therefore, advancement of the needle without complete visualization cannot identify which structures are penetrated. Anesthetic should never be injected without the needle tip in clear view, and injections should be halted immediately if spread of local anesthetic solution within the tissues is not visualized.
Despite preparation and training, complications do occur. Interscalene blocks are associated with temporary paralysis of the phrenic nerve; caution should be exercised to select patients with sufficient respiratory reserve to tolerate paralysis of the hemidiaphragm. The most feared complication of a peripheral nerve block is local anesthetic systemic toxicity (LAST). While ultrasound guidance and aspiration prior to injection can minimize intravascular injection, toxicity may still occur. Seizure, coma, respiratory arrest, ventricular arrhythmias, and cardiac arrest can all be consequences of LAST. Initial treatment of these events still begins with standard ACLS algorithms, but lipid emulsion therapy may be indicated when these efforts fail. Prior to performing a peripheral nerve block, it is important to confirm that lipid emulsion is stocked in the ED and that it can be obtained quickly if needed.
When performed properly, ultrasound-guided peripheral nerve blocks can be a safe and effective alternative therapy for pain control in the ED in a variety of indications. Comfort with sonographic anatomy and needle guidance can enable the general emergency physician to successfully perform these blocks.
Guide to Specific Nerve Blocks
Once the general principles of nerve blocks are understood, each site requires a mastery of site specific anatomy and landmarks as shown in the following figures. Anesthesia of the upper extremity can be achieved with a block of the brachial plexus (Figs. 22.10 and 22.11) (7,8,30, 31, 32, 33, 34); the hand, with forearm blocks (Figs. 22.12, 22.13 and 22.14) (9). Anesthesia to most of the lower extremity can be achieved with a proximal block of the femoral nerve (Fig. 22.15) (7,22,35, 36, 37, 38). The lower leg can be anesthetized with a block of the sciatic nerve at the popliteal fossa (Fig. 22.16) (7,39). The sole of the foot can be anesthetized with a block of the posterior tibial nerve (Fig. 22.17) (40,41).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree