Soft Tissue Inflammation: PET-CT and SPECT-CT Imaging
Klaus Strobel
Katrin D. M. Stumpe
Gustav K. von Schulthess
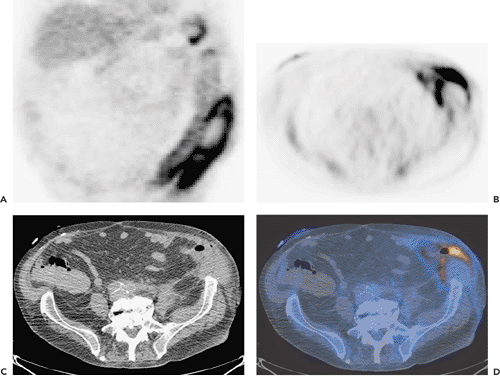
Soft-tissue infections, eluding clinical detection, occur in many settings. Because their therapy depends on the type and extent of the infectious foci, knowing where the infection is located is very important. Imaging can define whether an infection is unifocal or multifocal, whether abscess formation has supervened, and whether soft tissue involvement alone is present or involvement of bones and joints has occurred. Positron emission tomography (PET) and integrated PET–computed tomography (CT) in soft tissue inflammation imaging are likely to become important imaging methods in patients with a suspected infected focus (Fig. 59.1). The current lack of widespread use has to do with the logistics involved: frequently emergency imaging is required, for which PET is not very suitable. Delayed PET imaging after institution of antibiotic therapy may not be very sensitive, so we do not advise the use of PET to detect infection in patients who have been receiving antibiotic therapy. Nevertheless, interesting data have appeared over the last few years on imaging of soft tissues. With increasing use of PET and better availability of fluorodeoxyglucose (FDG), FDG-PET is likely to become available even in emergency situations, and thus its use may increase in the next few years. As in tumors, anatomic location of a lesion is frequently important; thus PET-CT also is believed to be important in PET infection imaging. Experimental studies with FDG-labeled leucocyte PET-CT are promising. The future will show wether the experimental results can be transferred into clinical routine.
Introduction
As noted in the previous chapter, various imaging methods can identify infectious foci in the soft tissues. CT is the mainstay to detect inflammation and infection in the chest, and ultrasonography and magnetic resonance imaging (MRI) are probably used most frequently in patients with soft tissue infections in the musculoskeletal system. Such patients are dealt with in Chapter 60.
The most frequently used nuclear medicine methods to identify soft tissue foci of infection have been gallium imaging, imaging with labeled leukocytes (either with indium [In], technetium [Tc], or with Tc-labeled antibodies against leukocyte surface antigens), colloids, or nonspecific immunoglobulins. All these methods have drawbacks. Gallium (Ga) imaging (1), leukocyte imaging (2), or antigranulocyte antibody imaging (3) all have a relatively poor spatial resolution; imaging of inflammation in the liver and spleen is difficult because of the normal accumulation of these radiopharmaceuticals in these organs. Nuclear imaging methods with these radiopharmaceuticals are lengthy procedures, typically requiring recurrent imaging over a 24-hour period. Moreover, swallowing of activity from sinus or upper respiratory infections leads to bowel activity in the absence of any intestinal disease. To aid interpretation, additional images of the head and chest as
well as repeated delayed images must be obtained. In patients with sepsis, the leukocytes are activated and migrate physiologically into the marginated pool of the lungs, so that a lobar pneumonia cannot be diagnosed with certainty.
well as repeated delayed images must be obtained. In patients with sepsis, the leukocytes are activated and migrate physiologically into the marginated pool of the lungs, so that a lobar pneumonia cannot be diagnosed with certainty.
The glucose analog fluorodeoxyglucose (FDG) has been demonstrated to accumulate in various infections (4,5,6), including abdominal abscess (Fig. 59.1) (7), brain abscess (8), lung abscess (9), lobar pneumonia (10), tuberculosis (11,12), Mycobacterium avium-intracellulare infection (13), mastitis (14), acute enterocolitis (15), and infectious foci in patients with acquired immunodeficiency syndrome (16). Compared with conventional nuclear imaging, FDG positron emission tomography (PET) appears to have several advantages. First, it is a relatively high-resolution tomographic method; second, it demonstrates only activated white cells, as only those take up FDG (see Chapter 58). Hence, infection imaging of the liver and the spleen with good contrast is possible; and third, the examination is relatively brief, providing definitive imaging results 1 to 2 hours after injection of FDG. It is therefore not surprising that a number of articles suggest an important role of PET in soft tissue infection. Furthermore, FDG also appears to be a more specific contrast agent than the extracellular fluid contrast agents used in MRI and computed tomography (CT).
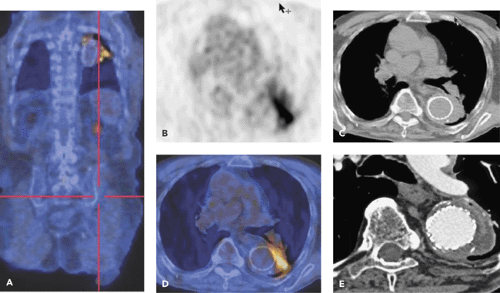
In thoracic inflammatory disease, PET plays a minor role because of the excellent ability of CT to distinguish airspaces from soft tissues. However, recognizing inflammatory disease in the chest as an incidental finding is still relevant. In vascular infections, mycotic aneurysms and graft infections are very interesting indications for PET-CT. In graft infections, care must be taken not to be overly sensitive in image interpretation, because a foreign-body reaction to a graft or stent may cause mild but clinically irrelevant inflammation. Typically, a florid graft infection shows substantial fluorodeoxyglucose (FDG) uptake (Fig. 59.2). The lung is not an organ in
which it is usually difficult to diagnose infection, but if lung FDG uptake is noted, it is always important to keep infection on the list of diagnoses. Little experience exists in the genitourinary system, as the renal collecting system contains much FDG, thus not providing good contrast to lesions in the kidneys and bladder. In identifying infected cysts in patients with polycystic kidney disease, FDG-PET/CT may help. Abdominal infectious disease is well diagnosed with PET; however, problems exist in the bowel because of considerable nonspecific uptake of FDG into bowel loops in many patients. The causes are usually not known, but in many instances, the uptake does not seem to reveal relevant pathology. Soft tissue and skin infections are readily recognized on PET images, but frequently these infections are emergency cases, and so few data exist. Finally, infection PET imaging seems to be valuable for the monitoring of disease activity, and few but promising infection PET data exist in patients with acquired immunodeficiency syndrome.
which it is usually difficult to diagnose infection, but if lung FDG uptake is noted, it is always important to keep infection on the list of diagnoses. Little experience exists in the genitourinary system, as the renal collecting system contains much FDG, thus not providing good contrast to lesions in the kidneys and bladder. In identifying infected cysts in patients with polycystic kidney disease, FDG-PET/CT may help. Abdominal infectious disease is well diagnosed with PET; however, problems exist in the bowel because of considerable nonspecific uptake of FDG into bowel loops in many patients. The causes are usually not known, but in many instances, the uptake does not seem to reveal relevant pathology. Soft tissue and skin infections are readily recognized on PET images, but frequently these infections are emergency cases, and so few data exist. Finally, infection PET imaging seems to be valuable for the monitoring of disease activity, and few but promising infection PET data exist in patients with acquired immunodeficiency syndrome.
In this and the following two chapters, we deal with soft tissue and bone infections, whereas sterile inflammatory processes of soft tissues in rheumatologic diseases are discussed in Chapter 62. Infections of the brain are dealt with in Chapter 24. Inflammation in children is addressed in Chapter 66.
Our experience with PET-CT tells us that the combination is very useful when the identification of the anatomic location is important (i.e., whether a lesion is in the vessel wall or surrounding a vessel, or whether the lesion is in the soft tissues or adjacent bones). Some soft tissue infections or inflammations may be adequately imaged with single-photon emission computed tomography (SPECT)-CT; however, substantial data are still missing.
Infections in the Lungs
Imaging diagnosis of lung infections is preformed with conventional chest x-rays and CT. PET is excellent in finding infected lung foci, but such foci are currently found incidentally. Therefore, PET is not used for this purpose, and we do not address the use of PET extensively in such patients. The key incidental findings of pulmonary inflammation/infection are in patients with chronic bronchitis and reactive lymph nodes accumulating some FDG as well as FDG uptake into sarcoidosis. Though the former presents typically with spotted foci in the mediastinum, which have to be differentiated from tumorous lymph nodes in bronchial carcinoma (Chapters 38 and 39), the latter condition may be easily recognized in some cases by a “cauliflowerlike”
bihilar uptake pattern that is almost pathognomonic (see Fig. 38.10).
bihilar uptake pattern that is almost pathognomonic (see Fig. 38.10).
Infections in the Cardiovascular System
FDG-PET infection imaging of the heart has not been explored, as the heart can have intense FDG uptake, thus making it impossible to be certain whether a myocardial accumulation is pathologic. Valvular endocarditis would be difficult to image because of the small structures involved. However, a preliminary report suggests that FDG-PET accurately detects infective endocarditis and may become a useful adjunct to echocardiography (17).
FDG accumulation in vessels and in the wall of the aorta can be observed regularly, and we must call this a normal finding, although some authors believe that such accumulation may correspond to vulnerable plaque formation (18,19,20) (see also Chapter 33). Activity in the vessels is due to incomplete clearing of FDG from the circulation (see Figs. 33.10 and 33.11), whereas weak aortic wall activity of grade 2 or less (see Fig. 33.9) is less frequently observed, and the reasons for its occurrence are unclear. It is important not to mistake this weak activity for a pathologic condition. Therefore it is suggested that when evaluating PET images with suspected vascular pathology, reading should not be overly sensitive, as sometimes is necessary in PET tumor imaging.
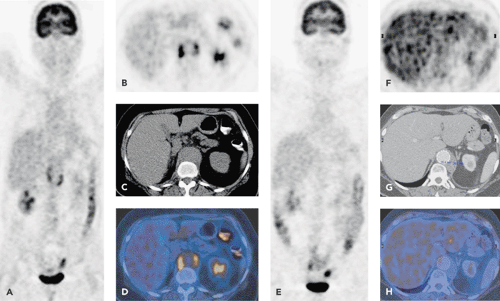 Figure 59.3 A 58-year-old female patient with back pain, fever, and elevated inflammatory blood parameters. FDG-active tissue around an aortic aneurysm is clearly seen on the preoperative PET/CT images (A–D). Blood cultures were positive for pneumococcus. PET/CT follow-up examination 1 month after implantation of an aortic stent graft and antibiotic treatment shows complete regression of the FDG uptake (E–H). Patient had normal C-reactive protein at this time. (See also Case 54).
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|