Fig. 21.1
Normal lymph nodes . Note that both small (a) and large (b) lymph nodes are hypoechoic and maintain an elongated shape with a hyperechoic fatty hilum coursing centrally
21.4 Abnormal Cervical Lymph Nodes
Metastatic disease to the cervical lymph nodes is common in thyroid cancer . The pattern of spread tends to follow a specific course in which the central compartment is typically affected first, followed by the lateral comportment. The proximity of the central lymph nodes to the thyroid gland makes these lymph nodes more susceptible to local spread. However, visualization of these lymph nodes is often difficult during initial presentation due to the presence of the thyroid parenchyma anteriorly. Level 6 and 7 lymph nodes are commonly involved first, followed by levels 3 and 4. Levels 2 and 5 are less commonly involved, but may still harbor metastasis ; metastasis to level 1 is very rare [14, 15]. The lower third of the neck (low jugular, midline low neck, and supraclavicular neck regions) is affected in 66.5 % and the middle third in 20.4 % of patients with metastatic thyroid cancer . Only 13 % of patients had metastasis to the upper third of the neck [15]. In evaluating level-specific metastasis in the lateral compartment, levels 3 and 4 harbor 71 % and 79 %, respectively, of the lymph node metastasis [16]. Therefore, identification of metastasis in any lateral neck lymph node during initial evaluation suggests involvement in the central neck. Understanding this pattern of spread is essential to proper operative management. For instance, positive lateral neck metastasis would necessitate a lateral neck dissection in combination with a central neck dissection .
21.5 Ultrasound Abnormalities
Abnormal lymph nodes consistently show deviation from normal morphologic patterns. However, ultrasound is limited in that there is no single sonographic finding or criterion that is diagnostic of malignancy. Specificity and sensitivity for malignancy vary according to individual features. A study evaluating the sonographic criteria for malignancy found that loss of the fatty hyperechoic hilum had the highest sensitivity (100 %), but the lowest specificity (29 %) in predicting malignancy. On the contrary, cystic appearance and hyperechoic punctuations had the highest specificity (100 %), but low sensitivities (11 % and 46 %, respectively) [14]. The importance in analyzing sonographic images is recognizing that deviation from the typical lymph node morphology should prompt further evaluation. Sonographic findings suggestive of malignancy are as follows:
21.5.1 Shape
Shape of cervical lymph nodes can be utilized to differentiate malignant from benign cervical lymph nodes. The classic elliptical form of benign lymph nodes is lost in malignant lymph nodes, and the shape becomes more rounded. Malignant lymph nodes also tend to develop an irregular contour and lose the smooth margin seen in benign lymph nodes (Fig. 21.2a). A round shape has been reported in 80 % of malignant lymph nodes, but in only 30 % of benign lymph nodes [17]. Shape of lymph nodes may be determined on transverse view with measurement of the width (transverse dimension) and height (anteroposterior dimension). Malignant lymph nodes are suspected when the height of the lymph node is equal to or greater than the width causing a more rounded appearance. A round shape is present when the ratio of the lymph node’s shortest to longest dimension is >0.5 [16, 17]. 80 % of malignant and only 30 % of benign lymph nodes have a ratio greater than 0.5, with a sensitivity and specificity of 80 and 71 %, respectfully [17]. A more specific assessment was proposed in which the largest and smallest dimensions are utilized to calculate the longitudinal/transverse ratio. A ratio of >2 defines an oval lymph node and a ratio of <2 defines a round lymph node [15]. Utilizing the longitudinal/transverse ratio of 2, 88 % of benign lymph nodes have a ratio of 2 or greater, while 66 % of malignant lymph nodes have a ratio of less than 2 [15]. Nonetheless, round shape is only 70 % specific and 37 % sensitive for identifying malignant lymph nodes [10, 14].
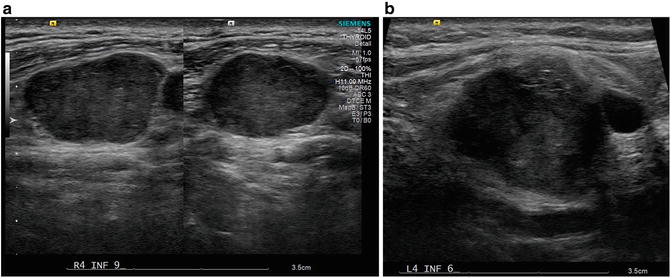
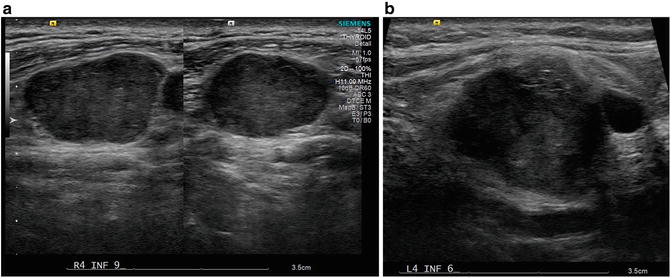
Fig. 21.2
Metastatic lymph nodes . (a) Lateral lymph node (level 4) with loss of elliptical shape, fatty hilum. Also note the irregular margins and heterogeneous echogenic pattern. (b) Level 4 lymph node with round appearance, irregular margins, heterogeneous solid echogenic pattern, and microcalcifications
21.5.2 Echogenic Pattern
Echogenicity is another sonographic finding that can be utilized to stratify the risk of metastatic cervical lymph nodes in patients with thyroid cancer . Hypoechoic lymph nodes, especially with a hyperechoic fatty hilum, are typically benign . In contrast, hyperechogenicity is more commonly associated with malignant lymph nodes. It has been demonstrated that 86 % of malignant lymph nodes are hyperechoic as opposed to only 4.5 % of benign lymph nodes [17]. Hyperechogenicity alone is a strong indicator of malignancy. Hyperechogenicity, with the loss of the fatty hilum, on ultrasound has a predictive value of 96 %, negative predictive value of 84 %, and accuracy of 90 % in identifying malignant lymph nodes in patients with thyroid cancer [17].
In addition to a hyperechogenicity , a heterogeneous solid ultrasound appearance also identifies a malignant lymph node. Benign lymph nodes exhibit a homogenous hypoechoic appearance on sonogram (Fig. 21.1). Malignant lymph nodes, on the other hand, may have a heterogeneous appearance with mixed hypo- and hyperechoic patterns (Fig. 21.2b). Hyperechogenicity and heterogeneity are also found in the solid component of cystic lymph nodes that harbor metastasis (Fig. 21.3). A recent study introducing a predictive model utilizing sonogram demonstrated that the existence of microcalcifications in the presence of a heterogeneous echogenic pattern was the best predictor of malignancy in cervical lymph nodes [18].


Fig. 21.3
Cystic degeneration of malignant lymph nodes. Note that the cystic lymph node may be associated with a (a) dense or (b) sparse central component. (a) Cystic lymph node with a dense, hyperechoic, central solid component with hyperechoic spots. (b) Cystic lymph node with sparse solid component. The solid component has irregular margins and hyperechoic spots
21.5.3 Size
Size in itself is not definitive for the diagnosis of malignancy. However, size may affect the malignant potential of lymph nodes. Metastatic lymph nodes in general tend to be larger than benign lymph nodes. When a minimum axial diameter was set at 6 mm, metastases were found in 93 % of lymph nodes, while only 17 % were benign [17]. The malignant potential significantly increases when lymph nodes are larger than 2 cm. Approximately 22 % of malignant lymph nodes are between 2 and 3 cm, compared to 12 % of benign lymph nodes. One study reported that 14 % of malignant lymph nodules were larger than 3 cm (Fig. 21.2), but only 1 % of benign lymph nodes reached this size cutoff. No difference existed in differentiating malignant risk in lymph nodes smaller than 1 cm, while lymph nodes measuring between 1 and 2 cm were more likely to be benign [15].
21.5.4 Cystic Degeneration
Lymph nodes, whether benign or malignant , are frequently solid. Earlier studies showed that over 80 % of metastatic lymph nodes were homogenous [13] and solid. Less often, malignancy may lead to cellular degeneration resulting in cystic formation within a lymph node. Cystic lymph nodes may also be found in benign diseases such as tuberculosis lymphadenitis, branchial cysts, and lymphoceles [10, 14]. In one study, cystic lymph nodes were found in approximately 20 % of thyroid cancer patients with malignant lymph nodes, and no benign lymph nodes exhibited cystic change [15]. However, others have shown that cystic degeneration may occur in up to 70 % of patients with papillary thyroid cancer [19, 20]. Most cystic lymph nodes are from papillary thyroid cancer (93 %); however, poorly differentiated thyroid cancer (3 %) and papillary serous carcinoma of the ovary (3 %) may also present with cystic degeneration [21]. Although identification of a cystic component has a specificity of 100 %, this finding is limited by a low sensitivity (10–34 %) [10].
Sonographic appearance of cystic lymph nodes varies. Generally, cystic lymph nodes lose the elliptical shape of a benign lymph node. The cystic component is anechoic under sonogram evaluation and may encompass a small single focus and multiple cystic areas or completely replace the lymph node [20]. The solid component is iso- to hyperechoic and may be dense or sparse relative to the cystic portion. Sonographic features of the solid component parallel findings typical of non-cystic malignant lymph nodes. Irregular margins, heterogeneity, microcalcifications, and increased vascularity are typical findings within the solid portion of cystic lymph nodes (Fig. 21.3).
21.5.5 Microcalcifications
Microcalcifications are classic finding in malignant thyroid nodules and lymph nodes of thyroid cancer patients, most commonly with well-differentiated thyroid cancer. Microcalcifications may be found in nearly 70 % of metastatic lymph nodes in patients with thyroid cancer [13, 15]. Though commonly associated with papillary thyroid cancer, microcalcifications may also occur in medullary thyroid cancer [22]. Identification of microcalcifications within a lymph node has a specificity of 100 %, but only 46 % sensitivity for malignancy [14]. A recent study showed that microcalcifications in the presence of a heterogeneous echo pattern were predictive of malignancy [18].
On ultrasound, microcalcifications appear as hyperechoic bright spots or reflectors (Fig. 21.4). As opposed to macrocalcifications found in thyroid nodules, microcalcifications do not refract the ultrasound waves. Therefore, the posterior acoustic shadow typical of macrocalcifications is not visible with microcalcifications. Microcalcifications may be found in homogenous lymph nodes or within the solid component of partially cystic lymph nodes .
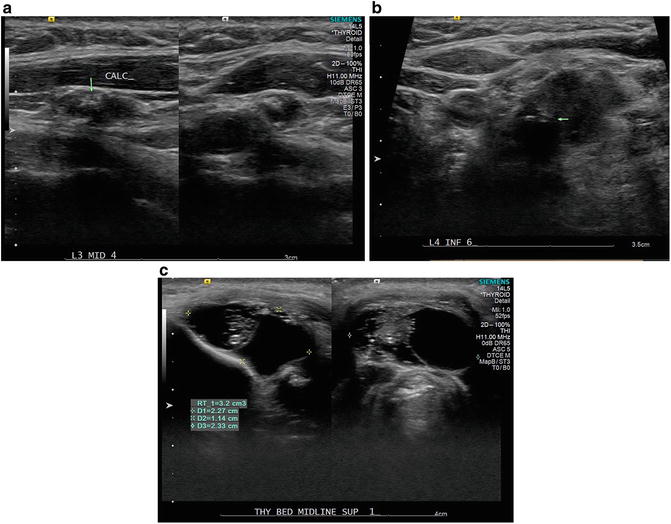
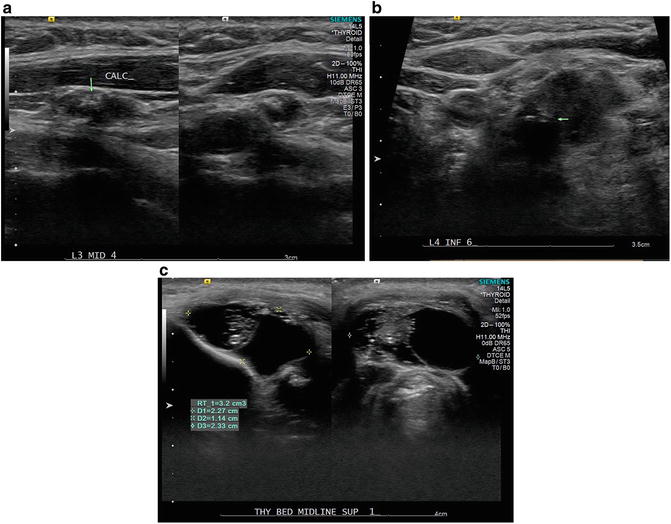
Fig. 21.4
Metastatic lymph nodes depicting varying patterns of microcalcifications . (a) Level 3 lymph node with aggregate of calcifications. (b) Heterogeneous lymph node with irregular margins and microcalcifications (arrow). (c) Metastatic lymph node with cystic degeneration and small punctate microcalcifications within the solid component
21.5.6 Vascularity
Increased vascularity within a tumor is commonly associated with malignancy. This is an important factor in evaluating cervical lymph nodes. Yet, benign factors (inflammation and infection) may also affect vascularity in cervical lymph nodes. Therefore, increased vascularity cannot be used as a single diagnostic criterion for malignancy. However, taking other ultrasound features into account, peripheral vascularity is one of the best factors for assessing malignant potential with a specificity of 82 % and sensitivity of 86 % for lymph node metastasis [14]. Other studies have shown a broader range with specificity of 57–93 % and sensitivity of 40–86 % [10].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree