CHAPTER 109 Sonography of the Renal Vessels
TECHNICAL REQUIREMENTS
Successful sonography of renal vessels requires the use of gray-scale sonography, tissue harmonics, color flow imaging, power Doppler, and spectral Doppler wave analysis. Additionally, ultrasound contrast agents can aid in the sonographic evaluation of renal vessels. In adult patients, a transducer frequency range between 3.5 and 5 MHz is required, whereas in pediatric patients a higher transducer frequency range can be used.1,2 Transducers with higher frequencies, of 6 to 8 MHz or more, are used to evaluate renal allografts because of their superficial location as compared with native kidneys. The highest transducer frequency that will provide the best resolution should be selected, depending on the depth of penetration required.3
Patients should fast or be on a clear liquid diet starting at midnight the day before the examination.2 Patients should also be encouraged to drink at least two 8-oz glasses of water the previous night and the morning of the examination.4 An oral dose of simethicone, an antigas medication, may be helpful in reducing bowel gas.
TECHNIQUES
Renal vascular ultrasound is indicated for a broad range of renal arterial and venous indications (Box 109-1). Clinically, renal arterial indications are more common, notably for the evaluation of possible renal artery stenosis. Select indications are detailed later. There are no known contraindications for the sonography of renal vessels.
BOX 109-1
Indications for Renal Vascular Ultrasound
 Malignant or accelerated hypertension or grade 3 or 4 hypertensive retinopathy; diastolic BP > 110 mm Hg
Malignant or accelerated hypertension or grade 3 or 4 hypertensive retinopathy; diastolic BP > 110 mm Hg Monitoring of the renal functional response to reperfusion and prediction of clinical outcome after renal artery revascularization
Monitoring of the renal functional response to reperfusion and prediction of clinical outcome after renal artery revascularization Patients with renal disease in whom MDCT angiography is problematic or contraindicated (e.g., poor renal function or first trimester of pregnancy)
Patients with renal disease in whom MDCT angiography is problematic or contraindicated (e.g., poor renal function or first trimester of pregnancy)Renal Artery Stenosis
The detection of renal artery stenosis in hypertensive patients (i.e., evaluation for renal vascular hypertension) represents the overwhelming indication in most practices. Renal artery stenosis (RAS) is estimated to be responsible for less than 5% of cases of hypertension. However, because it is one of the few treatable causes of hypertension, second only to the secondary hypertension caused by the use of oral contraceptives in women,5 it remains a common indication for renal artery imaging. About one quarter to one third of all patients with RAS eventually develop ischemic nephropathy. Renovascular hypertension is also responsible for the development of end-stage renal disease in 20% of patients. RAS is also seen in approximately 7% of all patients who have cardiovascular diseases (e.g., atherosclerosis, myocardial infarction, congestive heart failure). Its association with stroke has also been reported. Atherosclerosis is the most common cause of RAS, with fibromuscular dysplasia representing a distant second, but other entities such as Takayasu arteritis can also result in renal artery stenosis.
Atherosclerotic Renal Artery Stenosis
Atherosclerotic RAS is mostly progressive, because 20% to 50% of patients with 50% stenosis of renal arteries show progression of the disease within a few years, and 12% to 20% of those having greater than 75% RAS end up with complete occlusion within a year (Figs. 109-1 to 109-9). If RAS patients are left untreated, then in addition to worsening renovascular hypertension, 5% to 16% of these patients will progress to complete occlusion of the renal artery. Even in cases of unilateral RAS, damage to the other kidney in the form of nephrosclerosis caused by increased systemic blood pressure will occur if RAS is left untreated.
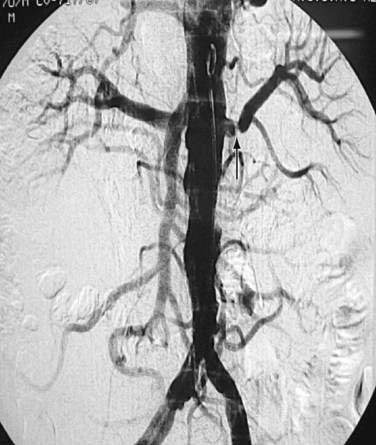
 FIGURE 109-9 Renal angiogram shows stenosis (arrow) in the proximal segment of left renal artery.
FIGURE 109-9 Renal angiogram shows stenosis (arrow) in the proximal segment of left renal artery.
(Courtesy of Dr. Gurpreet Singh Gulati, New Delhi, India.)
Fibromuscular Dysplasia
Fibromuscular dysplasia (FMD) results in RAS involving mainly the mid or distal part, and sometimes the intrarenal branches, of the renal artery (Fig. 109-10). FMD is almost eight times more commonly seen in females than males and usually occurs in younger individuals. FMD represents a collection of vascular diseases that affect the intima, media, and adventitia. It generally accounts for less than 10% of cases of RAS. FMD can be classified according to the layer of the arterial wall involved. Clinically, FMD involves the renal artery in three forms, with most (up to 90% of patients) having medial fibroplasia, which typically affects patients younger than 35 years. About one third of patients with medial fibroplasia show progression of the disease, but complications such as dissection and thrombosis are rarely seen.
The classic appearance of FMD, which is seen in 85% of patients, is known as the string of beads appearance, as seen angiographically. An endovascular ultrasound study of FMD by Gowda and colleagues6 has challenged the status of renal angiography as the gold standard for RAS in FMD patients. Other findings of FMD, such as a fibrous diaphragm, may not be seen sonographically; however, focal narrowing of the main artery caused by medial or adventitial hyperplasia might be seen.
Takayasu Arteritis
Takayasu arteritis, or nonspecific arteritis, is associated with stenosis (and occlusion) of the aorta and renal arteries (Figs. 109-11 to 109-15). This disease is more prevalent in Far Eastern and Southeast Asian countries.7 The disease is classified into four types, with each type assigned to the vessels involved: aortic arch, thoracoabdominal aorta and its branches, both aortic arch and thoracoabdominal aorta, and pulmonary arteries.8 The thoracoabdominal type is more common in the Indian subcontinent and Southeast Asia, as is middle aortic syndrome. The disease predominantly involves the media of the vessel and then progresses to cause fibrosis of intima and the adventitia. Most of the patients present during adulthood, very frequently during the third decade of life.
Renal Artery Thrombosis
A renal artery can be occluded by atherosclerotic embolism, thromboembolism, thrombus in situ, aortic dissection, or vasculitis. Renal artery embolism is a common cause of renal insufficiency in older patients, especially those with atherosclerosis. Renal artery thromboembolism can occur in association with a variety of conditions, such as aortic aneurysm, myocardial infarction, bacterial endocarditic, aseptic vegetations, and even paradoxical emboli originating in the right heart caused by congenital heart diseases such as atrial septal defect (ASD; Fig. 109-16).
Renal Vein Thrombosis
Renal vein occlusion can occur because of thrombus formation, intraluminal tumor, or external compression of the renal vein. The predisposing factors for renal vein thrombosis (RVT) are nephrotic syndrome, membranous glomerulonephritis, hypercoagulable states, abdominal surgery, dehydration, trauma, renal cell carcinoma and, rarely, hypereosinophilic syndrome (Figs. 109-17 and 109-18).9–13 Renal vein thrombosis is commonly seen in patients with nephrotic syndrome and can present as acute or chronic RVT. RVT occurs in up to 40% of patients of nephrotic syndrome caused by membranous glomerulopathy, membranoproliferative glomerulonephritis, and amyloidosis. RVT is frequently bilateral in cases of nephrotic syndrome.
Intraluminal extension of tumor into the renal vein can occur with renal malignancy, notably renal cell carcinoma, but also may be seen with renal lymphoma, transitional cell carcinoma, and adrenal tumors such as Wilms’ tumor.14,15 Extension of the thrombus from ovarian veins into the renal vein can also occur.16
Renal Transplant Assessment
Renal transplantation is becoming routine practice and evaluation presents a particular challenge. Ultrasound is an ideally suited modality for renal transplant assessment because of its relatively lower cost and excellent ability to assess the transplant noninvasively without the need for ionizing radiation or the use of iodinated contrast agents, with their inherent nephrotoxicity concerns. Further discussion of renal transplant imaging can be found in Chapter 112.
TECHNIQUE DESCRIPTION
Anatomic Considerations
Renal Arteries
Both renal arteries arise from the abdominal aorta approximately 1 to 1.5 cm below the origin of the superior mesenteric artery and at the level of the superior border of the L2 vertebra, with the origin of the left renal artery (LRA) slightly inferior to the right renal artery (RRA; Fig. 109-19). The RRA arises from the anterolateral aspect of the aorta at approximately the 10 o’clock position and the left main renal artery arises from the posterior or lateral aspect of the aorta at about the 4 o’clock position. The RRA courses anterolaterally in its proximal few centimeters, and then courses posterior to the inferior vena cava (IVC) and eventually follows a posterolateral course towards the right kidney (Figs. 109-20 and 109-21). Sonographically, it is identified as the largest vessel seen posterior to the inferior vena cava. The LRA runs a shorter course and passes between the superior mesenteric artery and the left adrenal vein (Fig. 109-22). Bannister and associates17 have reported accessory renal arteries in approximately 25% to 30% of individuals; however, most imaging studies have reported these in from 12% to 22% of patients (Fig. 109-23). The accessory renal arteries can arise from the aorta or iliac arteries. The rate of successful imaging of the accessory renal artery varies between 0% and 24%. In the presence of a normal main renal artery, a concerted attempt should be made to search for these vessels because stenosis of an accessory renal artery can similarly result in renovascular hypertension.18–20 The small caliber of the main renal artery is an indirect clue to the presence of the accessory renal artery.21
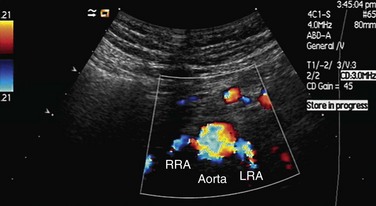
 FIGURE 109-19 Color Doppler image acquired by the midline transverse approach shows origin of both renal arteries from aorta.
FIGURE 109-19 Color Doppler image acquired by the midline transverse approach shows origin of both renal arteries from aorta.
Intrarenal Arteries: Segmental, Interlobar, and Arcuate Arteries
After entering the hilum, the main renal arteries split into anterior and posterior divisions. The arteries in these divisions give rise to segmental arteries, usually four, that supply each of the four vascular regions of the kidney—apical, anterior, posterior, and inferior. The segmental arteries give rise to lobar and interlobar arteries that travel between the medullary pyramids (Fig. 109-24). After traversing the corticomedullary junction, interlobar arteries give rise to arcuate arteries. Arcuate arteries give rise to the cortical and medullary branches, which supply the cortex and medulla, respectively. Most of the blood flow (90%) to the kidney goes to the cortex, with only 10% flowing into the medulla.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






























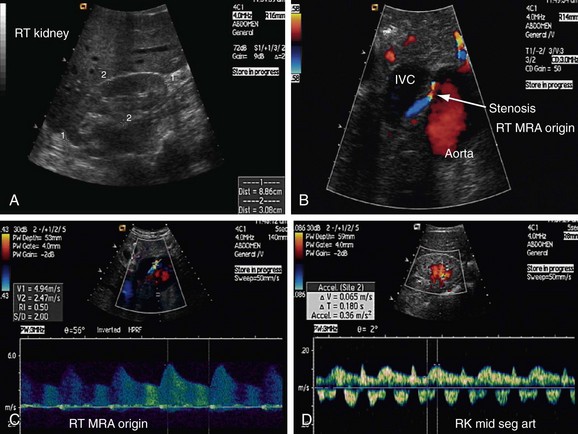
 FIGURE 109-1
FIGURE 109-1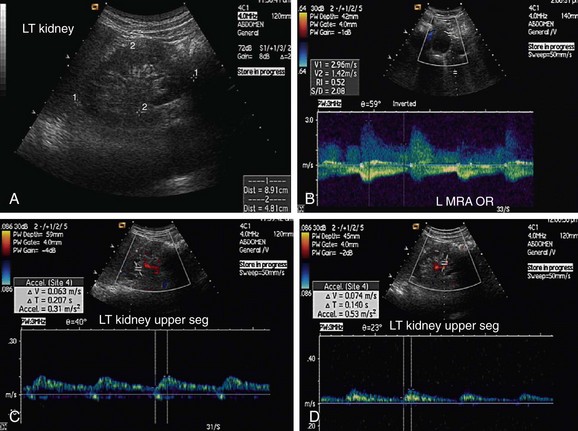
 FIGURE 109-2
FIGURE 109-2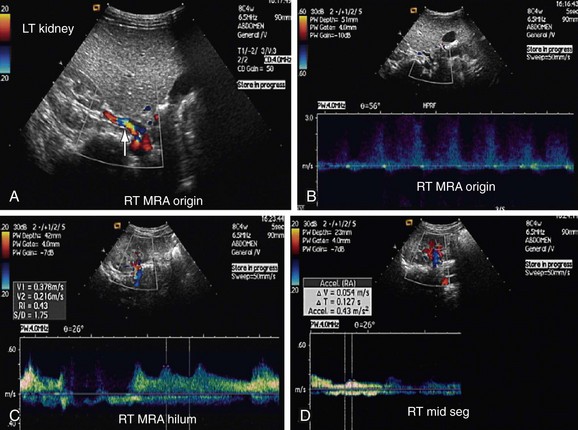
 FIGURE 109-3
FIGURE 109-3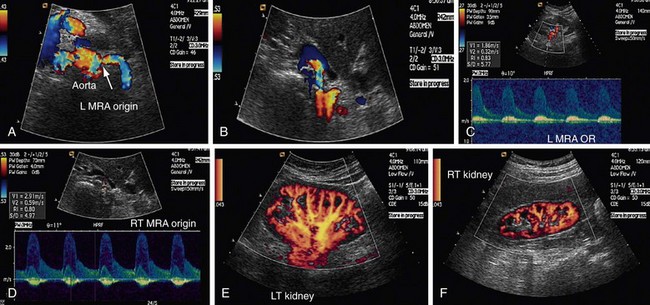
 FIGURE 109-4
FIGURE 109-4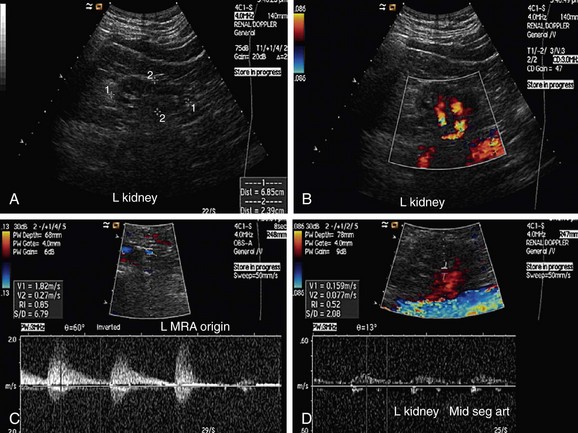
 FIGURE 109-5
FIGURE 109-5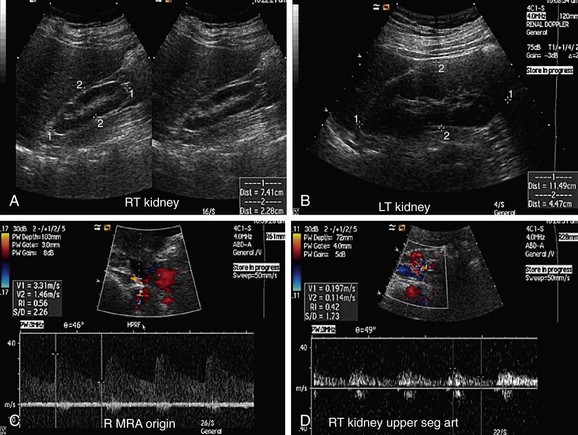
 FIGURE 109-6
FIGURE 109-6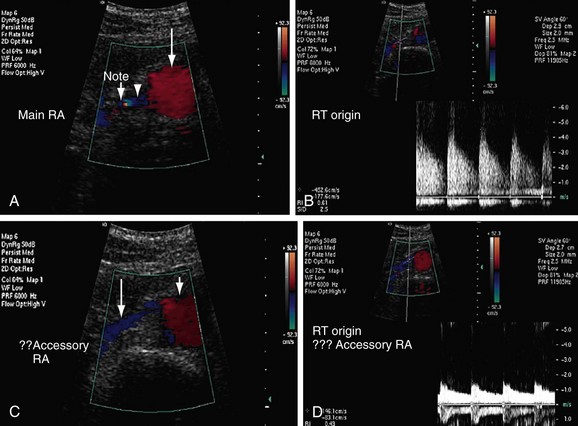
 FIGURE 109-7
FIGURE 109-7
 FIGURE 109-8
FIGURE 109-8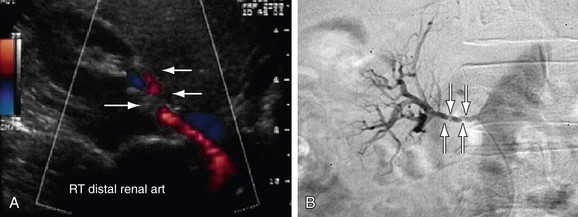
 FIGURE 109-10
FIGURE 109-10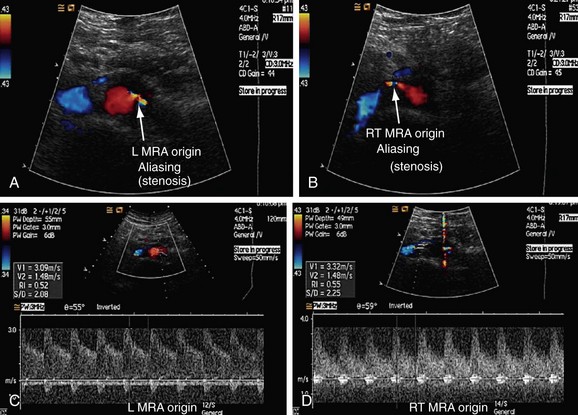
 FIGURE 109-11
FIGURE 109-11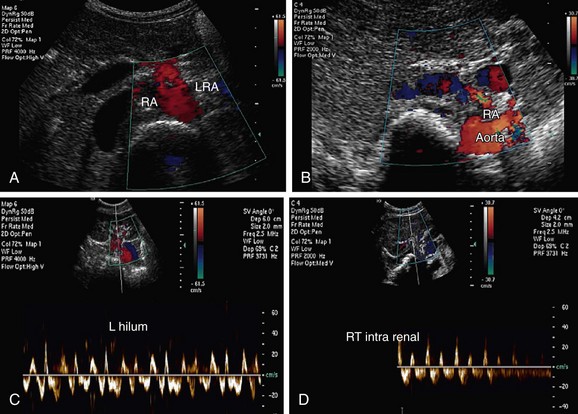
 FIGURE 109-12
FIGURE 109-12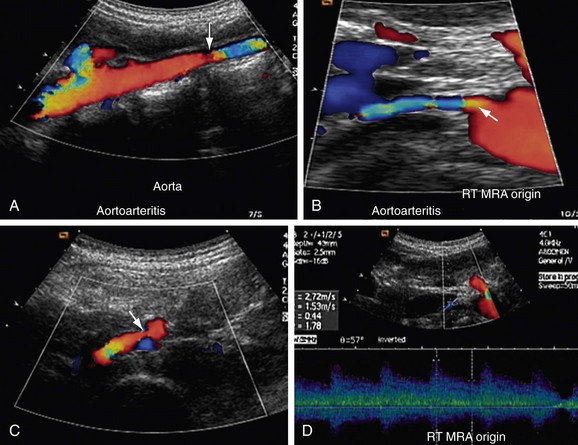
 FIGURE 109-13
FIGURE 109-13
 FIGURE 109-14
FIGURE 109-14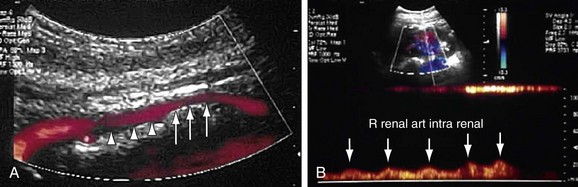
 FIGURE 109-15
FIGURE 109-15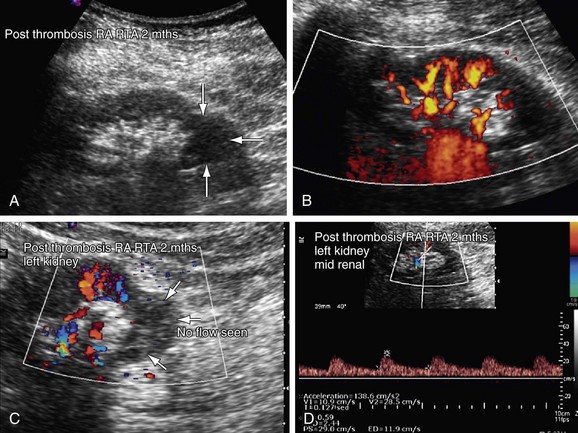
 FIGURE 109-16
FIGURE 109-16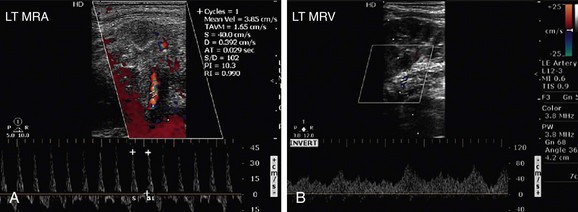
 FIGURE 109-17
FIGURE 109-17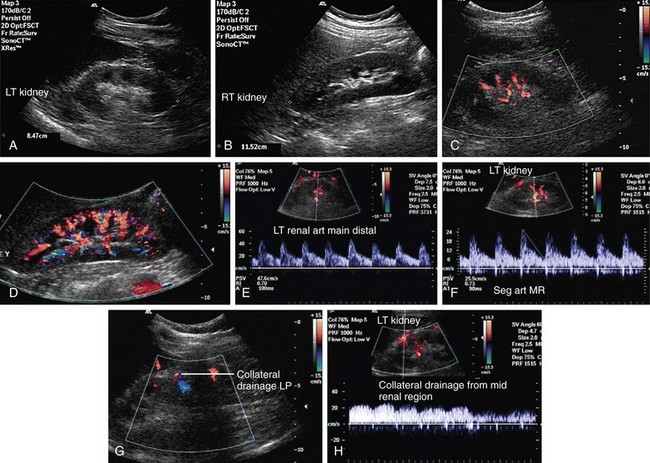
 FIGURE 109-18
FIGURE 109-18
 FIGURE 109-20
FIGURE 109-20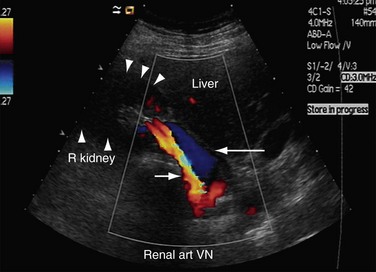
 FIGURE 109-21
FIGURE 109-21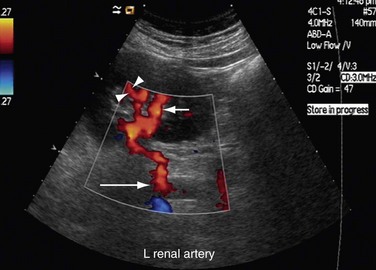
 FIGURE 109-22
FIGURE 109-22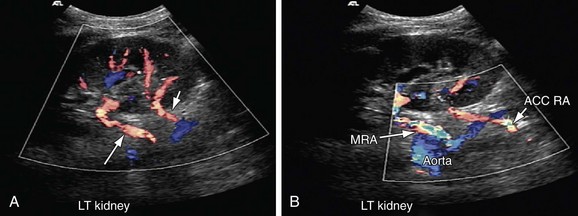
 FIGURE 109-23
FIGURE 109-23