Special Considerations in Pediatric PET-CT and SPECT-CT Imaging
Lise Borgwardt
Annika Loft
Liselotte Højgaard
Children are not just small adults. They differ in their psychology, normal physiology, and pathophysiology, and various issues specific to pediatric patients should be considered when planning a positron emission tomography (PET) scan, a PET–computed tomography (CT) scan, a single-photon emission computed tomography (SPECT) scan, or a SPECT-CT scan. SPECT studies have been used for more than 2 decades in pediatric patients, and different protocols and regimes have been presented. PET imaging of children is a relatively new but growing area, and it presents challenges common in pediatric nuclear medicine but not pertinent to the imaging of adult patients. These include dealing with children, dosimetry, organization within the pediatric department and with other departments, and preparation of the child. Further, informing the child and parents on the fasting procedure, the imaging procedure, and the tracer injection is extremely important, and there is a need for proper positioning, sedation, and bladder emptying. Finally, there are various pitfalls in the performance and interpretation of pediatric PET scans that must be avoided to ensure both proper interpretation and the safety and comfort of the patients.
Both PET and conventional nuclear medicine have recently added hybrid scanners with integrated CTs for better anatomic referencing. These scanners raise new considerations, including the increased radiation dose and which indications justify the increased radiation exposure.
Introduction
Positron emission tomography (PET) is a well-established diagnostic imaging technique used in oncology, infection imaging, neurology, and cardiology in adults. The technique is used less often in children, but recent advances have improved the imaging quality and shortened the length of the imaging procedure (1), making pediatric PET scanning increasingly relevant. Single-photon emission computed tomography (SPECT) has been used for more than 2 decades in pediatric patients, and different protocols and regimes have been presented (2,3).
Nuclear medical and PET examinations in children are very rewarding, especially when the staff understand the requirements of the child and parent. A successful examination can be defined as one in which a high-quality study is achieved and the child and parents feel that their emotional needs are met (4).
Dealing with Children
“Children are very special persons who need to be treated with caution and care and whose integrity must be
respected” (5). In nuclear medicine, dealing with children is very different from dealing with adults. Children are not just small adults. They differ in their psychology, normal physiology, and pathophysiology, and various special issues need to be considered when planning a PET or a SPECT scan for a child. Everybody involved must enjoy working with children, and the scans should be performed by a child-oriented staff. Patience, flexibility, imagination, and truthfulness are crucial qualities when dealing with children.
respected” (5). In nuclear medicine, dealing with children is very different from dealing with adults. Children are not just small adults. They differ in their psychology, normal physiology, and pathophysiology, and various special issues need to be considered when planning a PET or a SPECT scan for a child. Everybody involved must enjoy working with children, and the scans should be performed by a child-oriented staff. Patience, flexibility, imagination, and truthfulness are crucial qualities when dealing with children.
Children have parents, and the parents are just as worried as the children, often even more so. In each case, the parents’ anxiety affects the child and hence the entire examination, but the parents also are able to offer the child the best comfort and security. This is why dealing with children also means dealing with the parents, and this is done successfully through communication and understanding and by figuring out how best to use their potential as contributors to the imaging process.
Dosimetry in PET
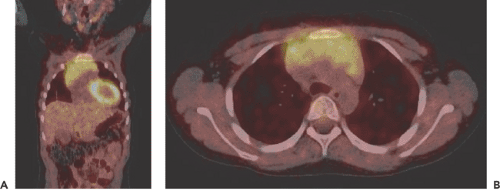
An important principle in diagnostic imaging in general is to limit the use of radiation, especially in children and in those with chronic diseases (see Chapter 9). The tracer most frequently used for clinical studies is fluorodeoxyglucose (FDG) (Fig. 66.1). The injected activity is 3 MBq per kilogram of body weight for brain studies (effective dose equivalent ≈ 4 mSv) and 6 MBq per kilogram of body weight for whole-body scans (effective dose equivalent ≈ 6 mSv.). The dose to the brain is 0.24 ± 0.05. The target organ (the organ receiving the highest radiation dose), the bladder wall, receives 1.03 ± 2.10 MBq. This can be reduced by good hydration and rapid drainage of radioactive urine. The heart wall is estimated to receive 0.89 ± 0.26 MBq. These figures are from a study that demonstrated that FDG-PET studies in newborns resulted in radiation doses lower than in adults and lower than infants who underwent conventional scintigraphy with technetium 99m (99mTc)-DTPA or 99mTc-MDP (6).
Dosimetry in SPECT
The amount of activity administered to an adult can be reduced for children by one of the following methods: body weight/70 kg, body surface area/1.73 m2, or height/174 cm (7). The pediatric task group of the European Association of Nuclear Medicine (EANM) has published a dose schedule (8) (Table 66.1). Furthermore, the child should be well hydrated, since frequent micturition reduces the radiation to gonads.
Organization
Organization and good communication are important in the nuclear medicine and the PET departments, especially between the camera and laboratory staffs. Equally important is comprehensive contact with the pediatric departments. This is not easily done, because nuclear medicine examinations are only some of many different examinations for which pediatric patients are referred, and they are definitely among the most complicated to prepare for. It is beneficial to give lectures in the pediatric departments not only for the physicians but most importantly for the staff nurses and also to have a contact person in each department for every specific examination (9). This will generally be the nurse taking care of the child, as these complicated examinations necessitate special arrangements. The technologist who is to perform the examination has to make the arrangements with the pediatric department, and all communications concerning a specific examination should be written on the referral in case another technologist has to take over. Good cooperation with the team of anesthesiologists is essential, as it takes flexibility to assist a nuclear medicine and PET department in performing pediatric scans. It saves time if both staffs are familiar with one another’s procedures during the examination in order to minimize the time spent.
Table 66.1 Eanm Dose Schedule for Recommended Activity in Children According to Body Weight | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Information
Information on planned examinations should be given both verbally and in writing. Good information will help to ensure compliance and keep the child’s anxiety at a minimum. The information leaflets for children should be specific for the different age groups, and pictures can be used for children who cannot read but are old enough to discuss the pictures.
Special Considerations in PET
Preparation for PET
Children, like adults, should fast for 6 hours (4 hours in the case of infants) before the FDG injection so as to establish the optimal target–background ratio (9,10). Fasting reduces the physiological utilization of glucose and brings down serum levels of insulin to near basal values, thereby minimizing the uptake of unspecific tracer into various organs (11). Infants may be fed 30 minutes after the tracer injection, when most of the FDG uptake period has passed (9). When other PET tracers are used, such as H215O, carbon 11 [11C]methionine (12), and nitrogen 13 [13N]ammonia, fasting is not necessary.
Activity Administration in PET
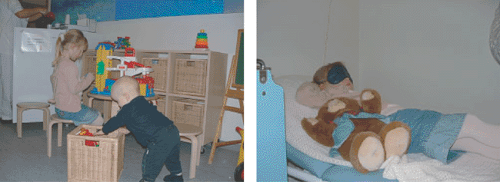
It is beneficial if the pediatrician has established intravenous entry by the time the child arrives at the PET department. It is also beneficial if the technologist who will perform the examination is waiting to receive the child and parents in the waiting room. This is the technologist’s first contact with the child and parents, and it is of great importance to get on good terms with the child immediately, for instance, by taking the child to a special corner of the room that contains toys, books, and small chairs (Figs. 66.2 and 66.3). It also provides a good opportunity to find out if anything special needs to be taken into account.
It is essential that the child and parents be informed about and understand the estimated time the procedure will take so that impatience does not impair the chances of obtaining a high-quality study. To ensure optimal conditions, the staff should not show signs of stress, and if it can be arranged, the child should be the first patient on the program in order to eliminate any delay on the camera.
To provide some quietness during the imaging procedure, the staff at the other cameras should be informed that a pediatric examination is underway via signs posted on the relevant doors in the department. The signs might say, “QUIET, CHILDREN’s EXAMINATION.” If possible, the child should be the only patient in the preparation room.
Before the FDG injection, the fasting child must rest for 30 minutes with eyes blindfolded for a brain scan and for 10 to 15 minutes without a blindfold for a whole-body scan, since it is important to minimize environmental effects on the distribution of glucose consumption in the brain. A pair of eyeshades can be used, and most children
accept wearing them, especially if they are told they are “Superman’s shades” (see Fig. 66.2B). Some of the younger children, however, will have to rest in a completely dark room, either because they refuse to have their eyes covered or because they are too curious about what is going on around them. After the injection, the child rests for another 30 minutes before the scanning begins. To ensure frequent emptying of the bladder, water should be offered.
accept wearing them, especially if they are told they are “Superman’s shades” (see Fig. 66.2B). Some of the younger children, however, will have to rest in a completely dark room, either because they refuse to have their eyes covered or because they are too curious about what is going on around them. After the injection, the child rests for another 30 minutes before the scanning begins. To ensure frequent emptying of the bladder, water should be offered.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree