Fig. 1
Two patients presenting with spinal cord symptoms. Myelopathic changes and enlarged perimedullary veins were evident on MRI. Complete spinal angiography must include the intracranial vessels and the pelvic vessels. (a) A right petrous apex dural AV fistula has caused venous high flow stenosis, and venous drainage has is now via the ipsilateral basal vein and from there to give retrograde flow in the contralateral basal vein, pontomedullary venous plexus, and finally to the spinal perimedullary veins. (b) Patient known to have spina bifida occulta. The lateral sacral artery supplies a DAVF at the spina bifida defect. This was not evident with a pelvic flush aortogram series and was only visualized with a selective internal iliac injection

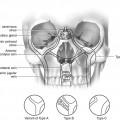
Fig. 2
Typical magnetic resonance imaging (MRI): (a) and DSA (b) appearances of a spinal DAVF. The combination of cord edema, mild cord swelling, and abnormally enlarged perimedullary veins is strongly indicative of a spinal vascular abnormality. The DSA reveals the arterial supply from a small radicular branch, the fistula (+), and the draining vein (x) which follows the nerve root to reach the perimedullary venous plexus
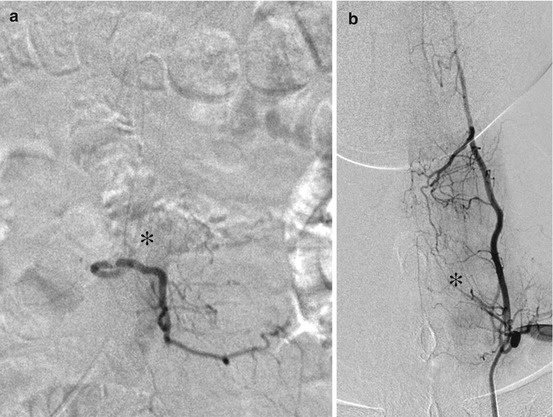
Fig. 3
Care is needed with every injection. (a) Patient presented with rapidly progressive paraparesis. MRI suggested cord ischemia but possible abnormal perimedullary vessels also noted. The DSA at T12 on the left revealed a tight stenosis of the radicular vessel and the Adamkiewicz artery taking origin distal to the stenosis. Atheromatous disease is more frequently encountered at the vessel origins, and even careful catheterization may cause vessel occlusion. Avoid excessive catheter and wire manipulation. (b) Proximal injection in the left thyrocervical trunk reveals a large radiculomedullary artery (+) taking origin from the origin of the ascending cervical artery. Inadvertent trauma with a guidewire could have disastrous consequences
Increased perimedullary venous pressure with cord venous ischemia.
Progressive, often stepwise, myelopathic symptoms commonly pain.
Most frequent in middle age males.
Coexistent spinal degenerative disease often blamed (diagnostic delay).
MRI – usually swollen/edematous (occasionally hemorrhagic) lower cord and conus (irrespective of the fistula site) and prominent vessels in spinal subarachnoid space.
MRI appearances overlap with other causes of cord swelling, including spinal cord infarction, tumor, and demyelination.
Spontaneous Intraspinal Hemorrhage
Spontaneous intraspinal hemorrhage is rare in the absence of a coagulation disorder or a history of spinal instrumentation.
Spinal arteriovenous abnormalities are a recognized cause of spontaneous epidural, subdural, and subarachnoid hemorrhage.
Spinal angiography should be considered in patients with intracranial subarachnoid hemorrhage where cerebral angiography has been normal, particularly if there is a heavy posterior fossa/foramen magnum blood load.
Structural (and possibly angiographic) MR imaging is desirable prior to undertaking DSA.
Planning for Surgery/Embolization
Vascular spinal tumors are surgically challenging to treat, and preoperative embolization reduces operative time and blood transfusion requirement.
Diagnostic angiography is indicated to map the vascular supply to the tumor deposit prior to surgery, and plan preoperative embolization.
Surgery to the lower thoracic/upper lumbar spine or to the adjacent aorta risks occlusion of the Adamkiewicz vessel. Angiography is indicated to localize the segmental vessel which gives rise to Adamkiewicz.
Diagnostic Spinal Angiography
Cross-Sectional Angiographic Imaging
Spinal vascular lesions fall into the differential diagnosis in a relatively large number of patients where there is evidence of myelopathy and possibly abnormal spinal vascularity on cross-sectional CT/MRI. It may be desirable to establish the exact position of the artery of Adamkiewicz prior to embarking on major spinal or thoracic vascular surgery. Comprehensive spinal DSA is not always appropriate in these circumstances due to the inherent risk of spinal cord ischemia. Safer, but less sensitive, spinal angiography can be obtained with noninvasive cross-sectional techniques.
CT Angiography
Multi-slice scanners have improved acquisition times, contrast, and spatial resolution.
Low sensitivity for spinal vascular lesions due to proximity of bony structures.
Bone subtraction techniques are improving and may further improve sensitivity.
Low risk and well tolerated.
Large radiation dose to cover whole spine.
MR Angiography
Contrast-enhanced elliptically centered acquisition.
Low spatial resolution but very good contrast resolution now possible.
Moderate sensitivity for spinal vascular lesions.
Some difficulty studying patients with myelopathy due to involuntary movements.
Low risk.
Time resolved studies can now be performed with promising results – may aid localization of level of shunt allowing more targeted catheter angiography.
Cone Beam CT
Modern angiographic equipment can be used to obtain cross-sectional imaging during aortic contrast injection.
Very good spatial and contrast resolution (very high arterial contrast concentrations can be achieved with aortic injection).
Invasive but risk lower than selective angiography and better tolerated.
Sensitivity in detection of spinal vascular lesions not well established but likely to be significantly better than with CT or MRI.
Can be used in combination with selective injections to clarify complex vascular anatomy.