, Joon Woo Lee1 and Jong Won Kwon2
(1)
Department of Radiology, Seoul National University Bundang Hospital, Seongnam, Kyonggi-do, Republic of Korea
(2)
Department of Radiology, Samsung Medical Center, Seoul, Republic of Korea
10.2.2 Hemangioblastoma
10.4 Neuromyelitis Optica
10.7 Syringomyelia
10.8.2 Acute Transverse Myelitis
10.8.3 Multiple Sclerosis
10.8.4 Neuromyelitis Optica
10.8.6 Acute Spinal Cord Infarction
10.8.8 Compressive Myelopathy
10.8.9 Syringomyelia
Abstract
We will explain the differential points of spinal cord tumors and nonneoplastic myelopathies in this chapter. We will describe the radiologic findings of common spinal cord neoplasms, acute transverse myelitis, multiple sclerosis, acute disseminated encephalomyelitis, acute spinal cord infarction, and syringomyelia.
We will explain the differential points of spinal cord tumors and nonneoplastic myelopathies in this chapter. We will describe the radiologic findings of common spinal cord neoplasms, acute transverse myelitis, multiple sclerosis, acute disseminated encephalomyelitis, acute spinal cord infarction, and syringomyelia.
10.1 Spinal Cord Tumors Versus Nonneoplastic Myelopathies
It is very difficult to differentiate spinal cord tumors from nonneoplastic myelopathies even with MRI. It is important to know the differential points between tumorous conditions and intramedullary nonneoplastic myelopathies in order to avoid unnecessary biopsy.
Fusiform enlargement with T2 hyperintensity of the spinal cord is seen in both tumors and nonneoplastic cord lesions. The MR findings that suggest nonneoplastic myelopathies are as follows: (1) multiple lesions with spinal cord swelling and skip area; (2) small focal, nodular, linear, or punctate enhancement in the peripheral white matter; and (3) decreased cord swelling, cord atrophy, or loss of enhancement at follow-up imaging. Spinal cord expansion in nonneoplastic myelopathies tends to be less than tumors. Spinal cord tumors including gliomas, lymphoma, and metastases usually show demarcated low-signal solid lesions within T2 hyperintensity in corresponding to enhancing region. However, nonneoplastic myelopathy shows relatively homogeneous high signal intensity on T2-weighted images regardless of enhancement (Table 10.1).
Table 10.1
Spinal cord tumor versus nonneoplastic myelopathy
Spinal cord tumor | Nonneoplastic myelopathy | |
|---|---|---|
Pattern | Usually single lesion | Can be multiple lesions with skip areas |
Cord expansion | Always present | Can be absent |
Enhancement | Mostly enhanced | Small nodular enhancement in the peripheral white matter |
Some lesions are not enhanced | ||
T2-weighted image | Can contain hypointense solid portion in corresponding to enhancing region | Usually homogeneous hyperintensity |
Cyst in the lesion | Peripheral enhancement | Simply reactive dilatation of the central canal |
Commonly seen in astrocytoma than in ependymoma | Mostly not enhanced | |
Follow-up imaging | Increased size of the lesion | Variable changes |
10.2 Common Neoplasms of the Spinal Cord
10.2.1 Ependymoma Versus Astrocytoma
With MR imaging, both ependymomas and astrocytomas cause fusiform cord expansion and are usually isointense to hypointense on T1-weighted images and hyperintense on T2-weighted images. These tumors usually extend cephalocaudally two to four vertebral segments. Astrocytomas and ependymomas usually have a slow, insidious onset with neck pain, stiffness, and myelopathy, and may cause scoliosis.
It is very difficult to differentiate an intramedullary astrocytoma from an ependymoma based on imaging features alone (Table 10.2). Hemorrhage and intratumoral cysts may exist more commonly with ependymoma, typically occurring rostral or caudal to the solid portion of the tumor (Choi et al. 2002). Syringohydromyelia is common with ependymomas and the margins of the syrinx do not enhance. Astrocytomas are more eccentrically located in the cord and have patchy enhancement and ill-defined margins of the enhancing region. Ependymomas are typically centrally located in the cord and contain an ovoid, well-defined, strongly enhancement region. Ependymomas can be a cause of subarachnoid hemorrhage and subsequently superficial siderosis.
Table 10.2
Ependymoma versus astrocytoma
Ependymoma | Astrocytoma | |
|---|---|---|
Age | Fourth to fifth decades | Pediatric, third to fourth decades |
Sites | Lumbar, cervical, thoracic | Cervical, thoracic |
Location in the spinal cord | Central | Eccentric |
Margin | Well circumscribed | Ill defined |
Contrast enhancement | Homogeneous | Patchy or irregular |
Cystic change and hemorrhage (cap sign) | More frequent | Uncommon |
10.2.2 Hemangioblastoma
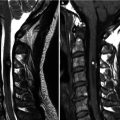
Hemangioblastomas are found more often in the thoracic than in the cervical region. Most of spinal hemangioblastomas (75 %) are intramedullary. But they may be intradural extramedullary or even extradural. Most cord spinal hemangioblastomas (80 %) are solitary and multiple lesions suggest the manifestation of von Hippel–Lindau syndrome. One-third of patients with spinal hemangioblastomas have von Hippel–Lindau syndrome. This is an autosomal dominant disease with cerebellar and spinal hemangioblastoma, retinal angiomatosis, renal cell carcinoma, and pheochromocytoma.
Spinal hemangioblastomas may produce diffuse or focal expansion of the spinal cord. Cord hemangioblastomas are commonly seen as highly vascular, discrete, nodular masses abutting the leptomeninges. There are prominent dilated tortuous feeding arteries and draining pial veins on the posterior cord surface. Associated cyst or syringohydromyelia has signal intensities comparable to CSF. Most of these tumors have peritumoral edema that is T2 hyperintense and T1 hypointense. Occasionally, the tumor may exophytically extend from the spinal cord. Enhanced MRI can easily delineate the strongly enhanced solid nidus of the tumor from surrounding edema and cysts. Cystic mass with an enhancing mural nodule is characteristic appearance of spinal and cerebellar hemangioblastoma. Conventional angiography shows a highly vascular mass, dense prolonged blush, and prominent draining veins.
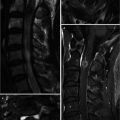
10.3 Acute Transverse Myelitis Versus Multiple Sclerosis
Acute transverse myelopathy (ATM) is acute inflammatory process involving both halves of the spinal cord, producing motor or sensory impairment (Choi et al. 1996). The causes of ATM are inflammatory and noninflammatory lesions, which are viral infections, multiple sclerosis (MS), postviral or postvaccinal processes such as acute disseminated encephalomyelitis, vasculitis such as systemic lupus erythematosus or Behcet’s disease, acute vascular infarction, paraneoplastic syndromes, and idiopathic. The diagnostic criteria of ATM are as follows: (1) development of sensory, motor, or autonomic dysfunction; (2) bilateral signs or symptoms; (3) clearly defined sensory level; (4) exclusion of extra-axial compressive cause by MRI; (5) inflammation with CSF examination or enhanced MR images; and (6) progression of nadir between 4 h and 21 days after the onset of symptom (Goh et al. 2011). The MR imaging appearance is quite variable, with mild spinal cord swelling, ill-defined homogeneous hyperintense regions on T2-weighted image, and isointense to hypointense regions on T1-weighted image over 3 or 4 spinal segments. Lesions occur most frequently in the thoracic cord. There are variable enhancement patterns after administration of contrast agent, including focal, diffuse, patchy, or peripheral patterns (Pardatscher et al. 1992). Follow-up MR imaging may show resolution of the abnormal signal and normalization or atrophy of spinal cord. Differentiation between ATM and MS is clinically important but is not easy with imaging alone (Table 10.3). MR imaging of the brain is a useful further study, which may reveal typical findings of MS (Campi et al. 1995). Of the patients with spinal cord MS, 90 % had intracranial MS plaques. Small, ovoid, enhancing spinal cord lesions without cord swelling have a high possibility of MS.
With MR imaging, most focal plaques of MS are less than 2 vertebral body lengths in size, occupied less than half the cross-sectional diameter of the cord, and were characteristically peripherally located with respect to a transverse cross-sectional reference (Tartaglino et al. 1995). Approximately two-thirds of the MS lesions in the spinal cord are present in the cervical region, and more than half of the patients with MS with cord plaques had multiple plaques.
Table 10.3
Acute transverse myelitis versus multiple sclerosis
Acute transverse myelitis | Multiple sclerosis | |
|---|---|---|
Location on axial image | Centrally | Peripheral, usually dorsolateral |
Extent on sagittal | ≥2 vertebral segments long | <2 vertebral segments long |
Extent on axial | Both halves of cross-sectional area | <1/2 cross-sectional area |
Brain involvement | No | Frequent concomitant brain involvement |
10.4 Neuromyelitis Optica
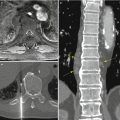
Neuromyelitis optica (NMO), also known as Devic’s disease, is an autoimmune, inflammatory disorder involving the optic nerves (optic neuritis) and spinal cord (myelitis). Spinal cord lesions lead to muscle weakness of the extremities, reduced sensation, and bladder dysfunction.
Diagnosis of neuromyelitis optica requires two absolute criteria plus at least two of three supportive criteria (Makhani et al. 2013). Absolute criteria are optic neuritis and acute myelitis. Supportive criteria are brain MR findings not indicating multiple sclerosis at onset, more extensive (≥ 3 vertebral segments) T2 hyperintensity on spinal cord MRI, and NMO-IgG seropositive status. Longitudinally extensive transverse myelitis (>3 segments) is the characteristic of NMO (Table 10.4). Lesions are usually localized to the cervical and upper thoracic cord.
Table 10.4
MRI characteristics of cord lesions in multiple sclerosis and neuromyelitis optica
MS | NMO |
|---|---|
Lesions shorter than two vertebral segments | Lesions extending over three or more vertebral segments |
Involvement of a portion of the cord | Involvement of the central part of the cord |
No T1 hypointensity | T1 hypointensity |
Rare cord swelling | Cord swelling (acute phase) |
Rare atrophy | Atrophy (chronic phase) |
10.5 Acute Disseminated Encephalomyelitis (ADEM)
Acute disseminated encephalomyelitis (ADEM) is postinfectious or postvaccinated immune-mediated inflammatory disorder of the white matter. The MR findings of ADEM are similar to those of multiple sclerosis, and it is indistinguishable on single study. But the clinical course of ADEM is monophasic and relapse of the disease is rare unlike multiple sclerosis. The spinal MRI shows multifocal flame-shaped white matter lesions with slight cord swelling. The brain is almost always involved and brain MRI should be included whenever suspicious cord lesion is found.
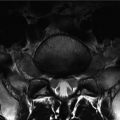
10.6 Acute Spinal Cord Infarction
The clinical feature of acute spinal cord infarction is motor, sensory, and autonomic disturbance of sudden onset. Infarction most often occurs in the lower thoracic cord, which is supplied by the artery of Adamkiewicz. Spinal cord infarction usually involves the anterior spinal artery territory, the gray matter of the anterior horns being more prone to ischemia than the peripheral white matter (Goh et al. 2011). On MR imaging, bilaterally symmetric foci of T2 hyperintensity are seen in the anterior column (owl-eye appearance) of the spinal cord. Sometimes, the T2 hyperintensity involves central gray matter. The peripheral white matter is usually spared. Diffusion-weighted imaging (DWI) of the spine will help make earlier and more confident diagnosis of infarction.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree