Clinical Presentation
The patient is a 62-year-old man with 3-year history of progressive neck pain, low back pain, bilateral shoulder pain, proximal muscle pain and weakness, and paresthesias. The patient had difficulty elevating his upper extremities on physical examination. The initial clinical diagnosis was cervical and lumbar osteoarthritis, shoulder capsulitis and bursitis, and possible fibromyalgia.
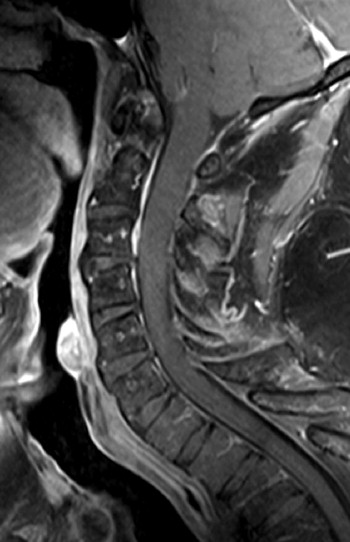
Imaging Presentation
Magnetic resonance (MR) imaging revealed a diffuse expansile process involving the medulla and cervical spinal cord extending inferiorly to approximately the C5 level. The intramedullary process is T1 isointense and T2 hyperintense, with no distinct margins between the abnormal process and the normal spinal cord ( Figs. 68-1 and 68-2 ) . There were no areas of contrast enhancement visible within the lesion ( Fig. 68-3 ) .


Discussion
Only 5% of spine tumors are intramedullary in location. However, 90% of all intramedullary cord tumors are gliomas, either astrocytomas or ependymomas. In adults, 60% of these are ependymomas and approximately 30% are astrocytomas. Hemangioblastoma is the third most common intramedullary tumor, accounting for approximately 5%. Intramedullary metastases comprise 4% of intramedullary tumors. Ganglioglioma, oligodendroglioma, xanthoastrocytoma, paraganglioma, primitive neuroectodermal tumor (PNET), and lymphoma can also arise within the spinal cord but are rare.
Intramedullary spinal cord astrocytoma is the most common intramedullary tumor in a child and the second most common intramedullary tumor in an adult. In children, 60% of intramedullary tumors are astrocytomas. These tumors range from WHO (World Health Organization) grade 1 to grade 4; 90 % of intramedullary astrocytomas are low-grade tumors (grade 1 or 2). WHO grade 1 astrocytomas are usually pilocytic astrocytomas and typically involve the spinal cord over multiple vertebral segments and may involve the entire spinal cord. The majority of intramedullary astrocytomas are WHO grade 2 fibrillary astrocytomas. WHO grade 3 and grade 4 tumors are uncommon, representing less than 10% of intramedullary gliomas. Most high-grade astrocytomas are WHO grade 3 anaplastic astrocytomas. WHO grade 4 cord astrocytoma, glioblastoma multiforme, is rare. The 5-year survival rate for cord astrocytoma is 75% to 80% for low-grade tumors, and the prognosis for high-grade tumors is extremely poor. Pilocytic astrocytomas have the best prognosis.
Cellular ependymomas are the most common subtype; these are malignant tumors, usually classified as WHO grade 2, but sometimes as grade 3. Anaplastic (WHO grade III) ependymomas have a tendency to disseminate throughout the central nervous system (CNS), often depositing tumors in multiple locations within the spinal canal, resulting in so called drop metastases . Intracranial seeding from spinal cord gliomas rarely occurs.
Intramedullary gliomas most commonly arise in the cervical cord, and less frequently in the thoracic spinal cord; 50% of cord astrocytomas occur in the upper thoracic cord. Ependymomas can occur throughout the cord. The myxopapillary ependymoma is the most common tumor occurring in the conus/cauda equina region. Cord astrocytomas and ependymomas usually have a slow, insidious clinical onset with myelopathy, neck pain, and stiffness, and may cause scoliosis in a child, adolescent, or young adult. These patients may present with progressive paraparesis and paresthesias. In children, back or neck pain and lower extremity paresis are the most common manifesting symptoms. Gait disturbance, occipital headache, kyphoscoliosis, torticollis, and bladder/bowel dysfunction may also occur.
There are six histologic subtypes of ependymomas: cellular (most common type), papillary, clear cell, tanycytic, myxopapillary, and melanotic (the least common). Ependymomas histologically display characteristic perivascular pseudorosettes or less commonly perivascular rosettes. Cord gliomas may have positive immunohistochemical markers including GFAP (glial fibrillary acid protein), S-100 protein, and synaptophysin. Mitoses are usually lacking in ependymomas. Astrocytomas have variable mitoses and usually high cellularity. Rosenthal fibers and hyalinized vessels are characteristically present in pilocytic astrocytomas.
Imaging Features
It may not be possible to differentiate an intramedullary astrocytoma from an ependymoma based on imaging features alone. Both can cause enlargement of the spinal canal, visible on radiographs. Tumoral cysts may be associated with spinal cord astrocytoma or ependymoma, but are more commonly associated with ependymoma, typically occurring rostral or caudal to the solid, enhancing portion of the tumor ( Figs. 68-4 to 68-6 ) .




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








