Multiple sclerosis is a diffuse disease of the central nervous system, and MRI of the spinal cord is highly recommended in the clinical evaluation of patients suspected of having multiple sclerosis. Within the new diagnostic criteria, spinal cord MRI increases sensitivity and possibly specificity for MS, but further work is needed to investigate other criteria that may give greater weight to the presence of cord lesions in patients with clinically isolated syndromes or suspected relapsing-remitting multiple sclerosis. Techniques should be further studied and validated in studies comparing these techniques with clinical status and histopathology, however.
The presence of hyperintense T2 lesions in the brain is a completely nonspecific finding, and many other autoimmune mediated inflammatory disorders (OID) and cerebrovascular diseases are known to produce brain lesions that may mimic multiple sclerosis (MS) on T2-weighted MRI. Multifocal areas of high signal intensity within the cerebral white matter with or without similar areas in the immediate periventricular region also may be seen on T2-weighted MRI in neurologically healthy people. The incidence of white matter abnormalities in the brain increases with age, and studies reported a prevalence of more than 30% in patients over the age of 60. Differential diagnosis between MS and OID or cerebrovascular disease can be difficult on T2-weighted brain examinations, especially if patients also show clinical signs of central nervous system (CNS) involvement.
Initial MR diagnostic criteria for MS were based on cerebral MR without inclusion of spinal cord MRI findings. These criteria were based on size, number, contrast enhancement, and location of focal abnormalities. The accuracy of these criteria was far from optimal, which resulted in a substantial number of misclassifications in a diagnostic setting. The spinal cord is frequently involved in MS, with more than 90% of patients who have MS showing abnormalities on T2-weighted MRI. In contrast to the brain, MS-like abnormalities are seldom found in the spinal cord of healthy volunteers, even past 50 years of age. Although spinal cord abnormalities have been reported in OID and cerebrovascular disease, appearance of such abnormalities may differ from those seen in MS. Spinal cord MRI may therefore be of great value, in addition to brain MRI, for the differential diagnosis of MS.
This article addresses conventional and quantitative techniques for spinal cord MRI in patients who have MS, their relation to clinical and histopathologic variables, and the diagnostic value of spinal cord MRI within the McDonald criteria for MS.
Technical features: which sequence to use
Imaging of the spinal cord in an adequate fashion is one of the most challenging features in MRI because images may be influenced by many sources of artifacts. Because of the location within the spinal canal, motion of the thorax, heart, and spinal cord, and additional turbulent and pulsatile flow of surrounding cerebrospinal fluid (CSF), ghosting artifacts, truncation artifacts, and patient movement artifacts may be present. The development of spinal phased array coils and fast sequences with flow compensation has enabled rapid imaging of the entire spinal cord within a reasonable time. A large rectangular field of view of 48 cm (18.90 in) enables visualization of the entire spinal cord within one sagittal image. Motion suppression for heartbeats, lung movement, and swallowing using cardiac gating, saturation bands, and phase encoding in the head-feet direction further optimizes spinal cord MRI.
Sagittal imaging
The gold standard MRI sequence to depict MS spinal cord abnormalities is dual-echo T2-weighted conventional spin echo (CSE), but other sequences, such as fast spin echo (FSE or TSE), short-tau inversion recovery (STIR), fluid attenuated inversion recovery (FLAIR), and gradient echo sequences also have been applied. Reports in literature are contradictory with regard to image quality and lesions sensitivity, with an exception for disappointing results using FLAIR sequences.
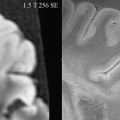
Regardless of sequence of choice, dual echo T2-weighted MRI should be considered because it offers unique benefits with regard to artifact interpretation and lesion detection. With an appropriate first short TE, an intermediate-weighted image is obtained in which CSF appears isointense to the normal spinal cord. Consequently, high signal intensity of CSF and pulsation artifacts, as observed on more heavily T2-weighted images, no longer hinders image interpretation. Subtle MS abnormalities in the spinal cord, which are slightly hyperintense to CSF on intermediate-weighted image scan, can be depicted. For the detection of diffuse MS abnormalities in the spinal cord, an intermediate-weighted image is of critical value because the abnormalities may be easily missed on more heavily T2-weighted images. For lesion location within the cord, the second (T2) echo is also helpful ( Fig. 1 ). Because of shorter acquisition time, FSE/TSE is preferred over CSE by some authors; however, FSE has a possible lower sensitivity for spinal cord abnormalities, especially diffuse. Reports that compared CSE and FSE/TSE sequences described nearly equal sensitivity for focal MS lesions in spinal cord ( Fig. 2 ). The use of a heavily T2-weighted single echo sequence alone decreased sensitivity for MS lesion detection substantially, however. With regard to inversion recovery sequences, FLAIR is considered not suitable for spinal cord MRI, although STIR or fast-STIR sequences seem to be useful for sagittal imaging and may depict additional lesions compared with CSE, although they are more susceptible to artifacts and less suitable as a stand-alone sequence.
In contrast to brain MRI findings, MS abnormalities are only rarely seen on sagittal T1-weighted images. When hypointense lesions are observed in a differential diagnostic setting, other diseases, such as Devic’s neuromyelitis optica (NMO) or even tumor, should be considered or excluded. Enhancing lesions may be seen on T1-weighted images, representing active MS pathology ( Fig. 3 ), although prevalence of these enhancing lesions is low compared with that of the brain. In an imaging protocol, in addition to brain examination, acquiring only postcontrast T1-weighted images may suffice.
Axial Imaging
Axial imaging of the spinal cord is more difficult compared with sagittal imaging because of CSF pulsation and motion artifacts, which may hinder image quality, and the small cross-sectional size of the spinal cord. Axial imaging is less time efficient for the detection of cord MS abnormalities because of structure geometry. Sagittal imaging is usually preferred, although axial imaging may serve as confirmation of MR findings on sagittal images. In the axial plane, high-resolution sequences are needed because of the small cross-sectional areas of lesions and spinal cord. Slice thickness of 3 to 4 mm and a pixel size of 1 mm 2 or less are preferred to obtain enough anatomic information, such as the location of abnormalities in specific columns and relation to central gray matter, besides contrast to noise of lesions compared with normal-appearing white matter (NAWM). Within the spinal cord, the different anatomy of the venous anastomosing network, compared with the brain, causes MS lesions to be primarily wedge shaped on axial sections and mostly located in the lateral and posterior columns, although they may appear in any column or gray matter.
Because of faster acquisition times and lower sensitivity to motion artifacts, TSE and gradient echo are usually preferred in the axial plane above CSE. The quality of gradient echo images can be improved further by the application of a magnetization transfer (MT) presaturation pulse. Thin-slice, T2-weighted, three-dimensional, FSE/TSE sequences also increase the detection of MS lesions but are more time consuming and artifact prone than two-dimensional FSE/TSE sequences. Comparison of sagittal and axial imaging for detection of MS abnormalities has not yet been studied, and no data have been published with regard to detection of diffuse abnormalities or differentiation of these abnormalities from focal lesions in the axial plane.
Depending on level of imaging, the size of the spinal cord may range from approximately 50 mm 2 to 100 mm 2 . In healthy controls, 90 mm 2 at level C2 may be considered normal; however, a large variability in size has been described, which limits the use for comparison of individuals. For measurement of the cross-sectional cord area (or volume), a heavily T1-weighted three-dimensional data set can be used to image voxels of approximately 1 mm 3 .
Diffuse and Focal Spinal Cord Abnormalities
MS spinal cord abnormalities consist of two types: focal lesions and diffuse abnormalities. Focal lesions are usually approximately one vertebra (maximum two segments) in length, are sharply delineated, are oval-shaped on the sagittal image, and are seen equally well on intermediate- and T2-weighted MRI. The so-called diffuse abnormalities are typically observed on intermediate-weighted MRI as areas of increased signal intensity, which is higher compared with that of the surrounding CSF (see Fig. 1 ). This diffuse abnormal signal is not well demarcated and is usually several segments long, although it appears frequently up to the whole length of the spinal cord and can be present in the entire diameter. Such diffuse abnormalities are difficult to recognize on T2-weighted images because spinal cord signal intensity is still lower than surrounding CSF.
On dual-echo SE images, focal spinal cord abnormalities in MS are often multiple. In a cohort of patients who were recently diagnosed with MS, already more than a median of three focal lesions were described, although a large range of abnormalities may be found, varying from a single focal lesion to a diffusely involved spinal cord with cases showing both focal and diffuse abnormalities ( Fig. 4 ). The latter is mostly the case in patients who have more advanced MS. Slightly more than 50% of focal cord lesions are found in the cervical cord. In the axial plane, these lesions are typically seen in the lateral and posterior columns and do not spare the central gray matter ( Fig. 5 ). They rarely cause focal swelling or atrophy of the spinal cord. In cases of more advanced MS, focal lesions may merge and form large confluent areas of high signal intensity exceeding two segments in length. Some patients may only show diffuse abnormalities along the entire cord length.
Sagittal imaging
The gold standard MRI sequence to depict MS spinal cord abnormalities is dual-echo T2-weighted conventional spin echo (CSE), but other sequences, such as fast spin echo (FSE or TSE), short-tau inversion recovery (STIR), fluid attenuated inversion recovery (FLAIR), and gradient echo sequences also have been applied. Reports in literature are contradictory with regard to image quality and lesions sensitivity, with an exception for disappointing results using FLAIR sequences.
Regardless of sequence of choice, dual echo T2-weighted MRI should be considered because it offers unique benefits with regard to artifact interpretation and lesion detection. With an appropriate first short TE, an intermediate-weighted image is obtained in which CSF appears isointense to the normal spinal cord. Consequently, high signal intensity of CSF and pulsation artifacts, as observed on more heavily T2-weighted images, no longer hinders image interpretation. Subtle MS abnormalities in the spinal cord, which are slightly hyperintense to CSF on intermediate-weighted image scan, can be depicted. For the detection of diffuse MS abnormalities in the spinal cord, an intermediate-weighted image is of critical value because the abnormalities may be easily missed on more heavily T2-weighted images. For lesion location within the cord, the second (T2) echo is also helpful ( Fig. 1 ). Because of shorter acquisition time, FSE/TSE is preferred over CSE by some authors; however, FSE has a possible lower sensitivity for spinal cord abnormalities, especially diffuse. Reports that compared CSE and FSE/TSE sequences described nearly equal sensitivity for focal MS lesions in spinal cord ( Fig. 2 ). The use of a heavily T2-weighted single echo sequence alone decreased sensitivity for MS lesion detection substantially, however. With regard to inversion recovery sequences, FLAIR is considered not suitable for spinal cord MRI, although STIR or fast-STIR sequences seem to be useful for sagittal imaging and may depict additional lesions compared with CSE, although they are more susceptible to artifacts and less suitable as a stand-alone sequence.
In contrast to brain MRI findings, MS abnormalities are only rarely seen on sagittal T1-weighted images. When hypointense lesions are observed in a differential diagnostic setting, other diseases, such as Devic’s neuromyelitis optica (NMO) or even tumor, should be considered or excluded. Enhancing lesions may be seen on T1-weighted images, representing active MS pathology ( Fig. 3 ), although prevalence of these enhancing lesions is low compared with that of the brain. In an imaging protocol, in addition to brain examination, acquiring only postcontrast T1-weighted images may suffice.
Axial Imaging
Axial imaging of the spinal cord is more difficult compared with sagittal imaging because of CSF pulsation and motion artifacts, which may hinder image quality, and the small cross-sectional size of the spinal cord. Axial imaging is less time efficient for the detection of cord MS abnormalities because of structure geometry. Sagittal imaging is usually preferred, although axial imaging may serve as confirmation of MR findings on sagittal images. In the axial plane, high-resolution sequences are needed because of the small cross-sectional areas of lesions and spinal cord. Slice thickness of 3 to 4 mm and a pixel size of 1 mm 2 or less are preferred to obtain enough anatomic information, such as the location of abnormalities in specific columns and relation to central gray matter, besides contrast to noise of lesions compared with normal-appearing white matter (NAWM). Within the spinal cord, the different anatomy of the venous anastomosing network, compared with the brain, causes MS lesions to be primarily wedge shaped on axial sections and mostly located in the lateral and posterior columns, although they may appear in any column or gray matter.
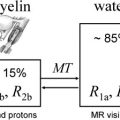
Because of faster acquisition times and lower sensitivity to motion artifacts, TSE and gradient echo are usually preferred in the axial plane above CSE. The quality of gradient echo images can be improved further by the application of a magnetization transfer (MT) presaturation pulse. Thin-slice, T2-weighted, three-dimensional, FSE/TSE sequences also increase the detection of MS lesions but are more time consuming and artifact prone than two-dimensional FSE/TSE sequences. Comparison of sagittal and axial imaging for detection of MS abnormalities has not yet been studied, and no data have been published with regard to detection of diffuse abnormalities or differentiation of these abnormalities from focal lesions in the axial plane.
Depending on level of imaging, the size of the spinal cord may range from approximately 50 mm 2 to 100 mm 2 . In healthy controls, 90 mm 2 at level C2 may be considered normal; however, a large variability in size has been described, which limits the use for comparison of individuals. For measurement of the cross-sectional cord area (or volume), a heavily T1-weighted three-dimensional data set can be used to image voxels of approximately 1 mm 3 .
Diffuse and Focal Spinal Cord Abnormalities
MS spinal cord abnormalities consist of two types: focal lesions and diffuse abnormalities. Focal lesions are usually approximately one vertebra (maximum two segments) in length, are sharply delineated, are oval-shaped on the sagittal image, and are seen equally well on intermediate- and T2-weighted MRI. The so-called diffuse abnormalities are typically observed on intermediate-weighted MRI as areas of increased signal intensity, which is higher compared with that of the surrounding CSF (see Fig. 1 ). This diffuse abnormal signal is not well demarcated and is usually several segments long, although it appears frequently up to the whole length of the spinal cord and can be present in the entire diameter. Such diffuse abnormalities are difficult to recognize on T2-weighted images because spinal cord signal intensity is still lower than surrounding CSF.
On dual-echo SE images, focal spinal cord abnormalities in MS are often multiple. In a cohort of patients who were recently diagnosed with MS, already more than a median of three focal lesions were described, although a large range of abnormalities may be found, varying from a single focal lesion to a diffusely involved spinal cord with cases showing both focal and diffuse abnormalities ( Fig. 4 ). The latter is mostly the case in patients who have more advanced MS. Slightly more than 50% of focal cord lesions are found in the cervical cord. In the axial plane, these lesions are typically seen in the lateral and posterior columns and do not spare the central gray matter ( Fig. 5 ). They rarely cause focal swelling or atrophy of the spinal cord. In cases of more advanced MS, focal lesions may merge and form large confluent areas of high signal intensity exceeding two segments in length. Some patients may only show diffuse abnormalities along the entire cord length.
Prevalence of spinal cord abnormalities and relation to the multiple sclerosis clinical phenotype
Prevalence of cord abnormalities in established MS is high, even in early stages of the disease. When focal and diffuse abnormalities are combined, up to 97% of patients who have MS may have abnormal spinal cord examinations. Results in publications may vary depending on patient selection and the imaging method used. In clinically isolated syndromes, the prevalence of spinal cord lesions is lower, especially if no spinal cord symptoms are present. Asymptomatic cord lesions are found in 30% to 40% of patients with clinically isolated syndromes, however; according to Poser, in patients who have recently diagnosed MS, criteria prevalence of abnormal cord examination may increase up to 83%.
With regard to the type and the extent of spinal cord abnormalities and MS phenotypes, a trend has been described. In patients who have relapsing-remitting MS (RRMS), spinal cord lesions typically consist of multiple focal lesions. In secondary progressive MS, abnormalities are more extensive; besides focal lesions, diffuse abnormalities are seen more frequently than in patients who have RRMS. Focal lesions also may become confluent as large, sharply delineated areas of high signal intensity. Spinal cord atrophy is common in this stage of the disease. In patients who have primary progressive MS (PPMS), cord abnormalities are extensive compared with brain abnormalities. In patients who have PPMS, focal and diffuse abnormalities have been described, although compared with the other MS phenotypes, diffuse abnormalities are more frequent. Imaging the spinal cord may help to diagnose PPMS in patients with few or no brain abnormalities.
Use of gadolinium
To appreciate disease activity and new lesion formation in a single MR examination, one has to acquire T1-weighted imaging after intravenous injection of gadolinium (Gd) in addition to T2-weighted imaging. Enhancing MS lesions on T1-weighted MRI after Gd injection reflect a disruption in the blood-brain barrier and active inflammation. Because the degree of leakage depends on the time after injection, a postinjection delay of 15 to 30 minutes should be considered.
Although the value of adding Gd-enhanced T1-weighted imaging in spinal cord studies has not been assessed as thoroughly as in the brain, delayed enhanced T1-weighted MRI may help to detect active spinal cord lesions in suspected cases of MS. Enhancing lesions seem to be found much less frequently in the spinal cord than in the brain, which limits the use of Gd enhancement in monitoring MS activity in the spinal cord. Enhancing MS cord lesions are usually small, no longer than two segments in cranial caudal length, are single, and show no or little perifocal edema or swelling of the cord. Gd enhancement in the spinal cord is often associated with new spinal cord symptoms ( Fig. 6 ). Adding postcontrast T1-weighted images to spinal cord MRI may be useful only when a new spinal cord lesion is suspected as the cause of a clinical relapse or when other diseases need to be excluded.
Brain and spinal cord abnormalities occur independently
In cross-sectional studies, no clear relation between the number of spinal cord lesions and the number or location of brain lesions has been found, which indicates that spinal cord abnormalities occur largely independently of brain lesions. No relation has been found between spinal cord atrophy and measurements of brain atrophy or number of brain lesions. To some extent, a relationship still seems plausible because brain abnormalities may cause secondary effects in the spinal cord, such as Wallerian degeneration. A relationship was found between T1 relaxation time measurements of brain tissue and spinal cord. Results also may be interpreted as an expression of diffuse disease involvement in brain and spinal cord, however.
The clinicoradiologic paradox: MRI correlation with symptoms and disability
A patient who has MS and little or no disability may have extensive brain MR abnormalities, whereas another patient with severe disability may have fewer abnormalities. This phenomenon is called the clinicoradiologic paradox. Solving this paradox, besides improving early diagnosis, is probably the most important research goal of MR research in patients who have MS.
There may be several causes for the poor correlation between conventional MRI and disability (Expanded Disability Status Scale). Among these factors, one should consider the lack of spatial resolution and, more importantly, the lack of pathologic specificity of T2-weighted MRI in MS. T2-weighted spinal cord abnormalities and clinical findings are only weakly associated. Compared with brain lesions, newly formed spinal cord lesions seem to be more related with new MS symptoms, although clinically silent lesions do occur in patients who have MS. Not all MS lesions in the spinal cord are clinically relevant. As in the brain, this may be caused by pathologic heterogeneity within spinal MS lesions.
To take a broad view: patients who have MS with spinal cord abnormalities are usually more disabled; patients who have PPMS tend to have the most extensive involvement, patients who have secondary progressive MS have intermediate involvement, and patients who have RRMS have the smallest spinal cord involvement when considering focal lesions and diffuse abnormalities. Diffuse cord abnormalities are associated with spinal symptoms, severe disability, and a PP disease course.
Currently, the best correlation between conventional MRI parameters and the Expanded Disability Status Scale has been found using spinal cord cross-sectional area/atrophy measurements. Spinal cord atrophy seems to be more severe in patients who have PPMS and secondary progressive MS, and it correlates with the appearance of diffuse abnormalities on sagittal MRI and disability. Spinal cord atrophy may occur independently of the amount of focal cord lesions, which suggests that the pathologic heterogeneity of spinal MS abnormalities exists and that mechanisms other than focal demyelination may be responsible for spinal cord atrophy. The changes in cross-sectional area of spinal cord are small, especially when compared with the wide range of cross-sectional area in healthy controls. As a consequence, the clinical use of spinal cord atrophy measurement is limited; however, there is a potential role for this measurement in long-term treatment trials aimed at the prevention of progressive tissue loss.
The clinicoradiologic paradox indicates that pathologic changes are variable between MS lesions and also must be present outside focal MS abnormalities. To study MS lesions and NAWM changes objectively, new quantitative MR techniques must be considered and findings from this approach must be assessed in terms of their histopathologic substrate.
Histopathologic associations
Only a few postmortem studies that have compared histopathologic changes in the spinal cord with MR characteristics in patients who have MS have been performed. A strong correlation between the extent of demyelination and signal intensity abnormalities, as depicted with high-resolution, intermediate-weighted MR images, was described. Signal intensity increases on intermediate-weighted images were not specific for axonal loss, however. Histopathologic findings described were heterogeneous and ranged from demyelination with active inflammation to severe gliosis. Axonal loss seemed to occur independently of demyelination and was described in focal and diffuse signal intensity abnormalities and was extensively present in the NAWM. Up to 30% of axonal loss in NAWM of spinal cords of patients who have MS compared with white matter of control individuals was found—a pathologic condition that was not visible on intermediate-weighted images at 4.7 T. Whether this finding is the result of Wallerian degeneration, a diffuse axonal injury process, or both remains unclear.
Quantitative MR techniques have revealed differences in relaxation times and magnetization exchange properties between controls and MS cases; quantitative MRI also revealed differences between types of MS histopathology. The degree of MR abnormality was found to be dominated by demyelination rather than axonal pathology, however. In contrast to the brain, T1 relaxation times were not able to distinguish between white matter of control specimens and NAWM. This phenomenon is apparently different from the situation in brain tissue, in which axonal loss is accompanied not only by atrophy but also by widening of extracellular spaces, which leads to abnormal relaxation mechanisms that are expressed on T1-weighted brain images as “black holes.” These differences may be explained by the central location of gray matter in the spinal cord, in contrast to brain, and consequently by the possibility of white matter collapse and resulting atrophy of the cord.
With regard to spinal cord atrophy, good correlations have been described with T1 relaxation time increase (and to a lesser extent with MT ratio [MTR] decrease and T2 relaxation time increase). Because these MR parameters are likely to primarily represent demyelination, it seems that cord atrophy itself is a feature that represents not only axonal loss but also loss of myelin, in which axonal density variance may occur independently of myelin density. This finding suggests that cord area measurement, which has been proposed as a clinically relevant marker for disease progression, may not be regarded as a direct measure of the number of axons present in the spinal cord. Considering initial promising results with regard to relation of clinical disability scores and diffusion-weighted (DW) MRI, it would be of interest to perform high-resolution DW MRI and relate findings with quantitative histopathology to define DW MRI sensitivity to axonal loss and demyelination.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree