James J. Rankine The cervical spine and thoracolumbar junction are the most common sites of spinal trauma. Specifically, the most common sites for fractures and dislocations are the lower cervical spine (C4–7), the thoracolumbar junction (T10–L2) and the craniocervical junction (C1–2). These mobile areas, particularly the cervical spine, can be injured with relatively little force. Patients with cervical trauma may present as ‘walking wounded’ to the accident and emergency departments with no other injuries and so despite the increasing use of CT as a first-line investigation, many patients with cervical trauma continue to be initially investigated with conventional radiographs. Approximately 15% of spinal fractures occur at more than one level and are non-contiguous, so the clinician must carefully assess the whole spine.1 In contrast to the cervical and lumbar spine, the thoracic spine is a relatively rigid structure, restricted in mobility by the thoracic cage. The thoracic spine, ribs and sternum constitute a bony ring and in common with fractures of bony rings elsewhere in the body, the ring often fractures at more than one point. A displaced fracture of the sternum should raise clinical suspicions of a fracture of the thoracic spine. Since greater forces are usually required to cause a thoracic spine fracture, associated vascular injury should be considered. For these reasons thoracic and lumbar trauma is most appropriately imaged as part of a polytrauma CT with intravenous contrast medium. Patients with osteoporosis may sustain thoracic axial load compressive fractures with little or no history of injury and are often initially assessed by conventional radiographs. The lack of force involved in the injury should not imply to the clinician that these are fractures that always run a benign course. The compressed vertebral body can develop avascular necrosis, leading to delayed post-traumatic collapse and spinal deformity, termed Kummell’s disease.2 It is important that these patients are followed up clinically, and where appropriate their osteoporosis is pharmacologically treated. Conventional radiographs cannot exclude injury in any part of the spine. While CT is sensitive to bony injury, it cannot exclude ligamentous disruption. This is particularly important in cervical trauma where the spine can be rendered unstable due to ligamentous disruption without any bony injury. The removal of spinal immobilisation in the light of negative conventional radiographs, or CT, should be performed in a controlled manner under senior supervision. Any clinical concerns, which are principally the degree of pain on gentle movement or the development of any neurological signs or symptoms, warrants an MRI examination, regardless of the findings on CT or conventional radiographs. It is important that the clinician managing a patient with spinal trauma is aware of the limitations of conventional radiographs and CT. Patients with spinal injury should have regular neurological observations performed. Any clinical deterioration in the neurology warrants an urgent assessment by MRI to investigate the possibility of an epidural haematoma, which can be surgically drained. Urgent surgical intervention cannot correct any neurological dysfunction sustained at the time of injury, but can prevent worsening neurological damage from an expanding epidural haematoma compressing the spinal cord.
Spinal Trauma
Clinical Aspects
Imaging Techniques and Evaluation
Cervical Spine
Conventional Radiographs
A full conventional radiographic examination of the cervical spine as a minimum includes a lateral view, anteroposterior (AP) view and an AP odontoid peg view. The lateral view should include the cervical–thoracic junction, and if not then a ‘swimmer’s’ view is performed where the arm adjacent to the radiographic plate is elevated and the beam is centred above the shoulder further from the plate and angled 15° in a cephalad direction. A full conventional radiographic examination is most appropriate in injury isolated to the cervical spine, with relatively low forces and where removal of immobilisation and clinical reassessment would be considered with negative findings. In many other situations, especially in the context of polytrauma, it is more appropriate to proceed directly to CT without conventional radiographs. Many institutions continue to perform a lateral radiograph as part of the initial assessment of the patient in the resuscitation room. Of the conventional radiographic projections, the lateral is the single most useful but with such rapid access to CT now available in most institutions the value of performing any conventional radiographs is debatable. The lateral radiograph no longer constitutes part of the primary survey in the ATLS guidelines3 but cervical immobilisation must continue until the spine can be radiologically and clinically cleared.
Despite the diminishing role of conventional radiographs they remain a common means of initially assessing many patients and, since the principles of interpreting the radiographs also apply to the interpretation of the sagittal and coronal reformats produced by a CT examination, it remains an important skill.
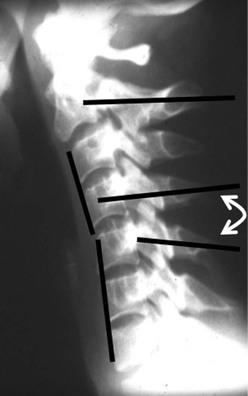
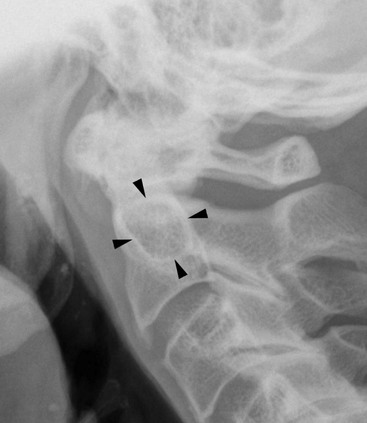
Alignment is assessed by visually assessing the spinal lines on the lateral radiograph (Fig. 59-1). They should all appear smooth and without interruption. The anterior spinal line passes along anterior borders of the vertebral bodies and the anterior aspect of the odontoid peg. The distance between the anterior arch of C1 and the odontoid peg should not exceed 3 mm in adults and 5 mm in children. The posterior spinal line passes along the posterior borders of the vertebral bodies. The junction of the laminae with the spinous processes forms the spinolaminar line. The lamina of C2 is normally up to 2 mm posterior to the spinolaminar line. The facet joint line marks the posterior aspect of the facet joints and in a true lateral projection the facet joints on each side are superimposed, giving a single line. The distance between this line and the spinolaminar line should be the same at all levels. The appearance of a double facet joint line at a particular level is evidence of an abnormality of rotation at that level which is usually caused by a fracture dislocation of the facet joints (Fig. 59-2). The appearance of a double facet joint line is termed the ‘bow tie’ sign.
Slight anterior subluxation of C2 on C3 is a common normal appearance in children. In this situation the malalignment causes disruption of the anterior spinal line and the spinolaminar line (Fig. 59-3). This distinguishes it from the Hangman’s fracture, where the anterior spinal line is disrupted but the spinolaminar line is not, since the posterior elements are no longer connected to the vertebral body (see later).
Malalignment can occur with angulation of the spine in the absence of anterior subluxation. The distance between the spinous processes should be roughly equal at all levels, taking into account the normal downward slope of the C7 spinous process A kyphotic angulation of the spine associated with widening of the gap between two spinous processes implies rupture of the posterior ligamentous structures at that level (Fig. 59-4).
Noting the central position of the spinous processes assesses alignment on the AP radiograph. The spinous processes of the cervical spine may appear bifid (the spinous process separates into two portions). This is a normal anatomical finding at many levels and in this situation the central point of the posterior elements is the point midway between the two tubercles of the spinous process (which may be unequal in size).
When assessing the AP through mouth odontoid peg view, normal alignment is demonstrated by noting that the lateral margins of the C1–C2 facet joints are symmetrically aligned with no overlap. On the lateral view the integrity of Harris’ ring should be examined at the base of the odontoid peg. This ring does not represent a distinct anatomical structure but is a composite shadow that includes the C2 body (Fig. 59-5).
The bones are assessed for fractures, cortical disruption and separate bony fragments. A well-corticated round opacity situated at the site of the anterior longitudinal ligament should not be mistaken for an avulsion. The lack of cortical disruption of the adjacent vertebral body and the absence of soft-tissue swelling are indicators of this normal finding, which is thought to represent a remnant of an ununited secondary vertebral ossification centre.
Soft-tissue swelling is assessed on the lateral radiograph. Superior to the level of the larynx the distance between the anterior aspect of the vertebral bodies and the posterior aspect of the air in the oropharynx should be no greater than one-third of the AP diameter of a vertebral body width. Inferior to the level of the larynx (usually C3 or C4 and frequently seen due to calcification in the laryngeal cartilage) it should be no greater than the AP diameter of the vertebral body. Intubation distorts the soft tissues behind the oropharynx, making the interpretation of soft-tissue swelling unreliable in intubated patients.
Lateral flexion and extension radiographs have traditionally been used to assess stability of the spine. Movement of the acutely injured spine in the presence of ligamentous disruption can cause neurological injury so there is no role for flexion and extension radiographs in the acutely injured spine. The stability of the spine and the presence of ligamentous disruption should be assessed by MRI. There remains a role for flexion and extension radiographs in the assessment of delayed instability, but this is likely to be some months after the acute event and should only take place after appropriate imaging and treatment of the acutely injured spine.
CT
CT of the cervical spine should include the spine from the cranio-cervical junction to the level of the third thoracic vertebral body. The precise imaging parameters will depend on the CT system being used, but an appropriately thin slice thickness should be selected to allow good-quality coronal and sagittal reformats. The alignment and soft-tissue swelling is assessed on these reformats using the same basic principles as the interpretation of the conventional radiograph. The axial sections are particularly useful for diagnosing bone fractures.
The presence of malalignment and soft-tissue swelling will often give an indication of ligamentous disruption in the absence of any bony injury but this is not always the case. If there is continued clinical concern following a normal CT, then MRI is warranted as CT cannot exclude a purely ligamentous disruption.
MRI
MRI of the cervical spine is best performed with the standard head and neck coils for the particular system being used to allow the best resolution with a small field of view. As there are frequently fractures at multiple levels the whole of the spine should be imaged in the sagittal plane. Axial sections can be planned from the sagittal slices and targeted at areas of abnormality. The principles of the sequences used and the image interpretation apply equally to the cervical spine and thoracolumbar spine.
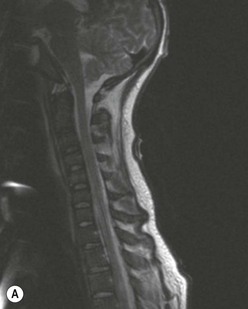
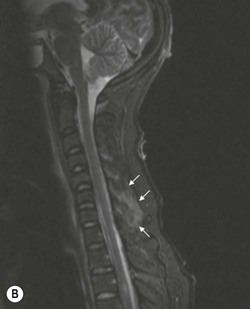
The sagittal sequences should include T1- and T2-weighted fat-saturated sequences. A short tau inversion recovery (STIR) sequence can be used as an alternative to the T2-weighted fat-saturated sequence since it is a robust sequence that provides reliable fat suppression. Bone and soft-tissue injury is more clearly demonstrated with fat-saturated sequences and injuries can be missed on standard turbo spin echo T2-weighted sequences (Fig. 59-6).
Gradient echo sequences may be used when assessing neurological injury since these better demonstrate haemorrhage, an important prognostic indicator for poor neurological recovery.
Thoracolumbar Spine
Conventional Radiographs
The conventional radiographic examination of the thoracic and lumbar spine includes AP and lateral views. The upper thoracic spine is particularly difficult to image on the lateral view due to the substantial overlying bone and soft tissues of the shoulders. CT, as part of a polytrauma CT protocol, most appropriately images the thoracic spine, as greater forces are required to cause a fracture of the relatively rigid thoracic cage. Conventional radiographs of the thoracic spine are rightly becoming a rare investigation.
Soft-tissue swelling due to a paravertebral haematoma is best demonstrated on the AP view of the thoracic spine where it causes focal widening of the mediastinum. Alignment is assessed on both the AP and lateral views. There should be an equal distance between the spinous processes and on the AP view the spinous process should be central with a symmetrical appearance of the pedicles and vertebral body.
The greater degree of mobility of the spine at the thoracolumbar junction renders this area particularly prone to injury and it is a relatively easy area to demonstrate with conventional radiographs due to the even quantity of overlying soft tissue. Patients with osteoporosis can sustain vertebral body compression fractures with fairly minimal forces. Often the challenge in interpreting the conventional radiograph is in determining what is an acute injury and what is old. Acute fractures tend to have sharp cortical margins and lucent fracture lines, whereas old injuries have smooth cortical margins and sclerosis. Ultimately, clinical correlation and, if necessary, MRI are a more reliable indicator of the age of a fracture than conventional radiographs.
A limbus vertebrae is a common developmental abnormality that should not be confused with an acute injury (Fig. 59-7). In the lumbar spine it most commonly affects the superior endplate of L4. These usually occur during adolescence before the endplates develop their full structural integrity. The intervertebral disc can prolapse anteriorly, lifting off the ring apophysis, typically occurring without any history of injury. The typical site and well-corticated appearance of the bone fragment are clues that this is not an acute injury.
CT
CT of the thoracic and lumbar spine should be performed as part of a polytrauma CT protocol that includes an intravenous contrast agent for the assessment of vascular injury. The precise imaging parameters will depend on the particular CT system but the axial imaging should allow sagittal and coronal reformats of sufficient diagnostic quality. The sagittal reformats of the thoracic spine should include the sternum since this is part of the bony ring of the thoracic cage and the integrity of the sternum is important in the stability of a thoracic fracture.
Because of the relatively rigid nature of the thoracic spine, injury usually involves bony fractures. CT is therefore very useful for diagnosing or excluding a thoracic spine injury. The thoracolumbar junction, on the other hand, is a relatively mobile structure and behaves more like the cervical spine in that purely ligamentous injury can occur without bony fractures. The presence of epidural fat within the spinal canal adjacent to the ligamentum flavum provides a natural soft-tissue contrast for assessing the posterior ligaments, an anatomical feature which is not present in the cervical spine (see later). However, ultimately, MRI remains the gold standard for assessing purely ligamentous injury.
Specific Injury Patterns
Cervical Spine
Atlanto-Occipital Dissociation
Dissociation between the cranium and cervical spine is an unusual injury since it is usually incompatible with life. It more commonly occurs in children. A simple assessment of normal cranial–cervical alignment is provided by tracing a line down the clivus that should extend onto the tip of the odontoid process. With cranio-cervical dislocation this line will fall anterior or posterior to the tip of the odontoid peg (Fig. 59-8).