, Joon Woo Lee1 and Jong Won Kwon2
(1)
Department of Radiology, Seoul National University Bundang Hospital, Seongnam, Kyonggi-do, Republic of Korea
(2)
Department of Radiology, Samsung Medical Center, Seoul, Republic of Korea
11.1.1 Multiplicity
11.1.2 Clinical Information
11.1.3 Location
11.1.4 Margins
11.1.5 Matrix
11.1.6 Pattern of Morphology
11.1.7 Signal Intensity
11.2.1 Multiple Myeloma
11.2.2 Spinal Lymphoma
11.2.3 Leukemia
11.4.1 Leptomeningeal Seeding
11.4.2 Intramedullary Metastasis
11.5 Illustration: Tumor
11.5.1 Bone Island
11.5.2 Hemangioma
11.5.3 Osteoblastoma
11.5.4 Osteoid Osteoma
11.5.5 Aneurysmal Bone Cyst
11.5.6 Giant Cell Tumor
11.5.7 Fibrous Dysplasia
11.5.9 Chordoma
11.5.10 Chondrosarcoma
11.5.11 Osteosarcoma
11.5.12 Ewing Sarcoma
11.5.13 Multiple Myeloma
11.5.14 Lymphoma
11.5.15 Neurogenic Tumors
11.5.16 Meningioma
11.5.17 Metastasis
Abstract
Spinal neoplasms are classified into three categories by the involvement sites: intramedullary, intradural extramedullary, and extradural compartment. The most common spinal bone tumor is metastasis, while primary bone tumors are much less frequent. Spinal bone metastasis was covered in the chapter on Common Bone Marrow Disorder, and primary intramedullary tumors were dealt with in the chapter on Spinal Cord Pathology. In this chapter, we will describe primary spinal bone tumors, hematologic malignancies, intradural extramedullary tumors, and intradural metastasis.
Spinal neoplasms are classified into three categories by the involvement sites: intramedullary, intradural extramedullary, and extradural compartment. The most common spinal bone tumor is metastasis, while primary bone tumors are much less frequent. Spinal bone metastasis was covered in the chapter on Common Bone Marrow Disorder, and primary intramedullary tumors were dealt with in the chapter on Spinal Cord Pathology. In this chapter, we will describe primary spinal bone tumors, hematologic malignancies, intradural extramedullary tumors, and intradural metastasis.
11.1 Primary Spinal Bone Tumors
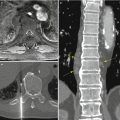
Benign vertebral lesions are usually asymptomatic and incidentally detected (Table 11.1), while malignant tumors cause back pain and sometimes manifest neurologic symptoms (Table 11.2). Initial imaging is usually plain radiography, which is not sensitive unlike in appendicular bones because of the complex anatomy of the vertebrae. Plain radiography, however, helps the surgeon in making a decision regarding overall spinal balance and the need for stabilization. CT is useful in the evaluation of bone destruction and calcified tumor matrix. CT helps evaluate the risk for vertebral body collapse. MR imaging is the best imaging modality for the evaluation of the epidural space and neural structures. T1-weighted MR images can delineate bone marrow architecture and fat content within masses. Postcontrast study is helpful to depict soft tissue vascularity and to differentiate cystic lesions from solid masses. Conventional angiography is invasive and usually used for preoperative embolization of the spinal tumors. Angiography is useful in determining the precise relationship between the tumor and the spinal vessels, especially in the evaluation of the artery of Adamkiewicz in the thoracolumbar region.
Cervical spinal tumors should be evaluated to describe their relationship to the vertebral arteries. In thoracic spinal tumors, it is necessary to depict the relationship to the ribs, posterior mediastinum, and pleura. Lumbar spinal tumors may involve the retroperitoneum. Sacral tumors can extend to the sacroiliac joints.
The differential diagnosis of spinal tumors can be narrowed down by evaluating the imaging findings including morphology or signal intensity of lesions, as well as enhancement patterns. Besides imaging findings, the age of the patient, number of the lesions, and location in the spine are most important in the differential diagnosis.
Table 11.1
Benign osseous tumors and tumorlike lesions of the spine
Lesion | Location | Imaging |
|---|---|---|
Hemangioma | Vertebral body | White polka dots on CT, prominent vertical trabeculae, hyperintensity on T1- and T2-weighted image (vessel and fat) |
Aggressive hemangioma: expansile, extraosseous extension | ||
Bone island | Vertebral body | Focal dense sclerosis, hypointensity on all MR sequences |
Osteoid osteoma | Neural arch (L, C-spine) | Lucent nidus with surrounding reactive sclerosis, size <2 cm |
Osteoblastoma | Neural arch (C-spine) | Expansile lytic lesion, multiple matrix mineralization, secondary ABC change |
Osteochondroma | Spinous, transverse process | Continuity of the lesion with marrow and cortex of the underlying bone, pedunculated/sessile lesion, cartilaginous cap |
Giant cell tumor | Vertebral body (sacrum) | Expansile, lytic, no mineralization, thin sclerotic rim, soft tissue component, secondary ABC change |
Aneurysmal bone cyst | Posterior elements | Multiloculated, expansile osteolytic lesion, fluid–fluid levels, internal septations |
Fibrous dysplasia | Anywhere | Polyostotic, mildly expansile osteolytic, ground-glass attenuation with CT |
Langerhans cell histiocytosis | Vertebral body | Uniform vertebral collapse (vertebra plana), no surround sclerosis, well detected on CT or enhanced MRI |
Table 11.2
Malignant osseous tumors of the spine
Lesion | Location | Imaging |
|---|---|---|
Chordoma | Vertebral body, midline (sacrum) | Midline expansile osteolytic lesion with soft tissue mass, hypointense septations (fibrous tissue) |
Chondrosarcoma | Vertebral body | Chondroid matrix mineralization (rings and arcs), large calcified mass |
Ewing sarcoma | Vertebral body (sacrum) | Invasive bone destruction and large soft tissue mass |
Osteosarcoma | Posterior element | Dense mineralization, sclerotic or mixed lesion with soft tissue invasion, periosteal reaction |
Telangiectatic type: osteolytic mass | ||
Lymphoma | Vertebral body | Permeative bone destruction, hyperostosis diffuse mottled pattern |
Multiple myeloma | Vertebral body | Diffuse or variegated osteolytic lesions, radiolucent areas or decreased bone density, plasmacytoma: mini-brain sign |
11.1.1 Multiplicity
Multiple lesions are most commonly seen in metastases. Multiple lesions in the spine with a known history of primary lung or breast cancer are most likely to be metastases. The most common multiple primary spinal tumors are lymphoproliferative lesions including multiple myeloma and lymphoma. Benign conditions that can present as multiple spinal lesions are Langerhans cell histiocytosis (LCH), hemangiomas, bone island (enostosis), and fibrous dysplasia.
11.1.2 Clinical Information
Night pain and painful scoliosis is highly suggestive of osteoblastoma or osteoid osteoma. In a young patient, osteoblastoma, Langerhans cell histiocytosis (LCH), and Ewing sarcoma predominate, whereas giant cell tumor is usually seen in the middle aged. In patients over 30 years of age, most tumors are malignant except for hemangiomas.
11.1.3 Location
Chordoma, giant cell tumor (GCT), and plasmacytoma are frequently located in the sacrum (Table 11.3). Hemangiomas are seen in the vertebral body, varying in size. The vertebral body is also favored by chordomas and Ewing sarcomas. Benign conditions commonly involving the posterior elements are osteoblastoma, aneurysmal bone cyst (ABC), and osteochondroma. Many lesions extend into the vertebral body or the posterior elements without confining in place. ABC mainly affects the pedicles but may spread to the body. Plasmacytoma develops in the vertebral body but is likely to extend into the posterior elements (Table 11.4).
Table 11.3
Differential diagnoses of sacral tumors
Chordoma | Giant cell tumor | |
|---|---|---|
Age | 30–60(40) | 10–30 |
M:F | M > F | M < F |
Nature | Malignancy | Benign |
Location | Midline or paramidline location | Eccentric location |
CT finding | Intratumoral calcification | Thin sclerotic rim |
T2 signal intensity | Very high | Low to intermediate |
Enhancement | Homogeneous | Heterogeneous |
Contents | Myxoid and mucin | Cyst, hemosiderin |
Table 11.4
Spine tumor according to location
Vertebral body, eccentric | Hemangioma, giant cell tumor, plasmacytoma |
Vertebral body, central | Chordoma, Ewing sarcoma, Langerhans cell histiocytoma |
Posterior column | Osteoblastoma, aneurysmal bone cyst, osteosarcoma, Osteochondroma |
11.1.4 Margins
Geographic bone destruction with sclerotic margins is seen with benign conditions such as hemangioma, bone islands, osteoid osteoma, osteoblastoma, and ABC. Ill-defined margins and permeative bone destruction are seen in malignant tumors such as osteosarcoma, Ewing sarcoma, and metastatic disease. Periosteal reaction is seen in osteosarcoma.
11.1.5 Matrix
Calcification within a lucent nidus surrounded by extensive reactive sclerosis is typically seen in osteoid osteoma and osteoblastoma on CT. Purely osteoblastic lesions show low signal intensity on T1- and T2-weighted MR images. The possible diagnosis of osteoblastic tumors includes bone island, osteosarcoma, and osteoblastic metastasis. Ring and arc-type calcification and enhancement pattern are characteristically seen in tumors containing cartilaginous components such as osteochondroma, chondrosarcoma, and chordoma. Cartilage-forming tumors can exhibit punctate or amorphous calcifications at plain radiography and CT. These calcifications appear as hypointense foci at MR imaging. Fibrous dysplasia typically shows as ground-glass attenuation with CT.
11.1.6 Pattern of Morphology
Expansile lesions are seen in ABC, osteoblastoma, and occasionally in aggressive hemangioma. Malignant lesions such as chordoma, Ewing sarcoma, and chondrosarcoma also have a tendency for soft tissue extension. These lesions tend to be symptomatic.
Fluid–fluid levels are seen in primary ABC and secondary ABC changes in GCT, osteoblastoma, and telangiectatic osteosarcoma. Secondary ABC has solid component, unlike primary ABC. Mini-brain sign is seen in plasmacytoma mimicking the MR appearance of brain. Vertebra plana is seen in LCH and sometimes in giant cell tumor.
11.1.7 Signal Intensity
Most pathological lesions have a tendency to have low signal intensity on T1-weighted image and high signal intensity on T2-weighted image. There are several exceptions. Hemangioma has increased signal intensity on T1-weighted image indicating the presence of fat. Low signal intensity on T2-weighted image is seen in GCT due to high collagen content and hemosiderin. Enhancement after administration of contrast agent can help characterize the tumor. Ring and arc pattern of enhancement is characteristic of cartilaginous tumors.
11.2 Hematologic Malignancies
11.2.1 Multiple Myeloma
On MRI, multiple myeloma can be displayed as five different infiltration patterns (Baur-Melnyk and Reiser 2009). First, the bone marrow signal is normal appearance in patients with low-grade infiltration with plasma cell. In such cases, normal pattern of bone marrow signal in MRI does not exclude the diagnosis of multiple myeloma. Second pattern is focal myeloma infiltration. This pattern is similar to metastases of solid malignant tumors. Third pattern is diffuse bone marrow infiltration, characterized by homogeneous hypointensity on T1-weighted images and diffuse enhancement on postcontrast images. This pattern is usually high-grade diffuse involvement of multiple myeloma. Fourth pattern is a combined focal and diffuse infiltration. Fifth pattern is variegated involvement (a so-called salt-and-pepper pattern), which is pathognomonic of multiple myeloma (Table 11.5).
Myelomatous infiltration results in diffuse osteopenia and vertebral compression fracture. This is difficult to distinguish from benign osteoporotic compression fracture. Both pathological fractures and osteoporotic fractures are common in old age group. MR imaging can help to differentiate the diagnoses in these situations.
Table 11.5
Metastasis versus multiple myeloma
Metastasis | Multiple myeloma | |
|---|---|---|
Common findings | Hypointensity on T1-weighted image, multiple lesions | |
Mineralization | Sclerosis, osteolytic, mixed pattern | Diffuse or variegated osteolytic lesions |
Size | Large and variable size | Small and uniform size |
Bone scan | Increased uptake | Photon defect |
Involvement | Variable | Number >5 per vertebral body, >3 contiguous vertebral bodies |
11.2.2 Spinal Lymphoma
Primary bone lymphomas are mainly diffuse large B-cell lymphomas. Spinal involvement may manifest as paraspinal, vertebral, and epidural masses. Vertebral involvement results more frequently from hematogenous spread rather than from direct bone invasion from adjacent lymph nodes. Vertebral lesions may have a sclerotic, lytic, or mixed appearance. The sclerotic (ivory vertebra) and mixed patterns are more common in Hodgkin disease. The appearance of vertebral lymphoma at CT and MR imaging is usually nonspecific. Focal bone marrow replacement and a surrounding soft tissue mass without cortical bone destruction may suggest lymphoma. But it can be seen with other small round cell tumors such as Ewing sarcoma.
11.2.3 Leukemia
Leukemias are composed of marrow accumulations of mature and immature granulocytes in myeloid and lymphocytes in lymphocytic leukemia. MRI usually shows diffusely low signal intensity of the bone marrow on T1-weighted images. The signal intensity is thought to be correlated with the aggressiveness of the chronic lymphocytic leukemia.
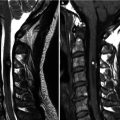
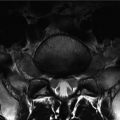
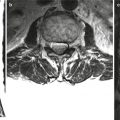
11.3 Intradural Extramedullary Tumors
Intradural extramedullary tumors are mainly composed of nerve sheath tumors and meningiomas (Table 11.6). Nerve sheath tumors are the most common intraspinal tumors and have two histologic types, schwannoma and neurofibroma. Most intraspinal nerve sheath tumor is solitary schwannoma, whereas neurofibroma can be multiple and usually associated with neurofibromatosis type I. Nerve sheath tumors are well-defined, solid masses of intermediate signal intensity on T1-weighted images. On T2-weighted images, they have variable signal intensity, sometimes a target appearance. Enhancement is variable and can be strong and homogeneous in most cases. Neurofibromas tend to encase the nerve roots and schwannomas which displace the nerve root due to their asymmetric growth. Schwannomas commonly have hemorrhage and cyst formation, which are rare in neurofibromas. When the tumor is solitary, however, differentiation of schwannoma and neurofibroma on MR imaging is very difficult.
Meningiomas of the spine often have calcifications. Most of meningiomas have similar signal intensity to the spinal cord on T1- and T2-weighted images. Meningiomas enhance strongly and homogeneously after administration of contrast agent and the attached dura to the masses can be enhanced (dural tail sign) (De Verdelhan et al. 2005).
Table 11.6
Schwannoma versus meningioma
Schwannoma | Meningioma | |
|---|---|---|
Age | Fourth decades | Fifth to sixth decades |
Sex | M = F | M < F |
Origin | Nerve sheath in peripheral nerve system | Dura matter |
Location
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|