KEY WORDS
Cauda Equina. The nerve root fibers arising from the terminal end of the spinal cord.
Cerebrospinal Fluid. Fluid that surrounds the spinal cord to protect it from rapid movement.
Conus Medullaris. The inferior (distal) termination of the spinal cord. The normal conus tip lies above the second to third lumbar (L2 to L3) level.
Dermal Sinus. A tract that extends from the skin surface to the deeper tissues. It may end in the subcutaneous tissues, or it may extend deeper to the level of the spinal cord.
Dermoid cyst. A cystic mass that contains hair and/or skin.
Diastematomyelia. Condition in which the spinal cord is split sagittally into two hemicords by a bony, cartilaginous, or fibrous septum.
Filum terminale. A cord-like structure that extends from the conus tip to the first coccygeal (S1) segment. It is surrounded by nerve roots of the cauda equina.
Hydromyelia. Dilatation of the central canal of the spinal cord.
Lipoma. Fat-containing mass that is usually associated with dysraphism, particularly in the form of a lipomeningocele.
Lipomyelomeningocele. This lesion is similar to that of a myelomeningocele, but with the addition of a lipoma.
Meningocele. An expanded subarachnoid space.
Myelocele. A form of spinal dysraphism in which the spinal cord is open and located at the level of the skin surface posteriorly.
Myelomeningocele. This lesion is similar to a myelocele except that it lies above the skin surface. There is no fluid-filled sac surrounding nerve fibers.
Neural Placode. The open spinal cord that protrudes onto the skin surface posteriorly.
Pilonidal Sinus. Deep hair-containing tract in the skin that overlies the sacrum and coccyx.
Spina Bifida. Refers to incomplete closure of the spine’s bony elements.
Spinal Dysraphism. Refers to a group of spinal anomalies, all of which have bony spina bifida and incomplete closure of the spinal canal, overlying soft tissues, and skin. The spinal canal contents may protrude posteriorly onto the skin.
Subarachnoid Space. Fluid-filled space that surrounds the cord and is lined by meninges. The outer meningeal layer, closest to the bony spine, is the dura mater. The inner layer, closest to the cord, contains the pia mater and the arachnoid. The subarachnoid space extends to about the second to fourth coccygeal (S2 to S4) level.
Syringomyelia. Fluid-filled space within the cord. Usually located outside of the central canal.
Tethered Cord. Abnormal low position of the spinal cord’s distal end in the spinal canal. The cord normally ends around L2 or L3.
The Clinical Problem
Sonography is an excellent method for evaluating the spinal canal and cord in neonates and young infants. The incompletely ossified midline posterior arches of the vertebral column provide an acoustic window that allows transmission of the ultrasound beam. The most common clinical indication for spinal sonography is a midline cutaneous lesion on the lower back, which has a high association with spinal dysraphism. Such lesions include skin dimples, hemangiomas, sinus tracts, hyperpigmented plaques, and hairy patches. Sonography is also performed in newborns with bony defects of the spine noted on plain radiographs (e.g., sacral absence) and/or the VATER syndrome (vertebral anomalies, anal atresia, tracheoesophageal fistula, renal and radial anomalies). Both of these conditions also have an increased frequency of dysraphism. Finally, sonography is performed in neonates with lower-extremity weakness or paralysis to detect cord compression or tethering and in newborns with suspected birth-related spinal cord injury to detect cord or nerve root lesions. Early detection of spinal lesions through the use of sonography may help treatment planning and decrease long-term morbidity.
High-resolution sonography can reliably show the spinal canal and its contents, and thus demonstrate the presence or absence of disease. If sonography is normal, no further imaging is necessary. If sonography shows spinal malformations, further imaging can be done with computed tomography or magnetic resonance imaging.
Sonographic Technique
Ultrasound of the spine is a reliable method of screening for spinal cord anomalies in infants <6 months of age. After 6 months of age, the acoustic window begins to close as a result of normal ossification of the posterior spinal elements. Subsequently, acoustic shadowing by the ossified spine makes evaluating intraspinal contents difficult.
Spinal sonography is performed with 7- to 15-MHz linear- or curved-array transducers. Scans are obtained with the neonate or infant in the prone position and with the legs flexed to create a relative kyphosis. This position produces splaying of the spinous processes, which improves acoustic access to the spinal canal. Scans are obtained with the transducer positioned in the midline over the unossified spinous processes. In infants with partially ossified posterior spinal elements and smaller acoustic windows, paramedian scans with the transducer positioned lateral and parallel to the spinous processes may improve visualization of spinal anatomy. Images are obtained in both longitudinal and transverse planes from the craniocervical junction to the cauda equina. A split-screen function or the newer extended field of view technology can help in demonstrating the relationship of pathology to normal structures. The level of the spine should be labeled on the image.
Normal Anatomy
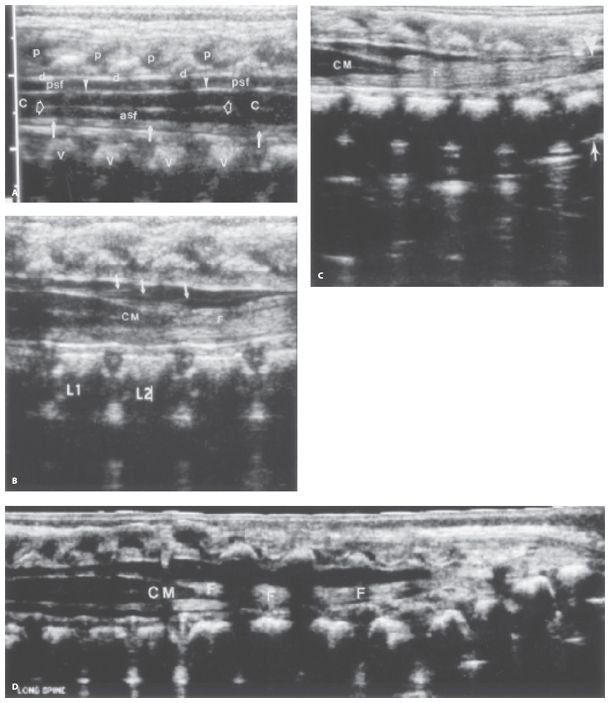
On longitudinal scans, the spinal cord is a hypoechoic tubular structure with echogenic anterior and posterior walls and an echogenic central complex, which represents the central canal. The spinal cord is bordered posteriorly by the hypoechoic cartilaginous spinous processes, the echogenic posterior dura mater, and the anechoic posterior subarachnoid space. The cord is bordered anteriorly by the anechoic anterior subarachnoid space and echogenic vertebral bodies. The cord gradually tapers at the level of the first or second lumbar vertebral body to form the conus medullaris. The conus medullaris is continuous with the fibrous filum terminale, which extends into the distal sacral canal. The filum terminale is an echogenic structure, which is surrounded by echogenic nerve roots (cauda equina). It inserts on the dorsal aspect of the first sacral segment (S1) (Fig. 37-1). Differentiation of the filum from adjacent nerve roots of the cauda equina is sometimes not possible by sonography. The subarachnoid space extends to about the second to fourth coccygeal (S2 to S4) level.
On transverse images, the spinal cord appears as a hypoechoic, round or oval structure with a central echogenic complex. Paired echogenic anterior and posterior nerve roots border the conus in the subarachnoid space. Transverse scans further caudad show the echogenic filum terminale surrounded by nerve roots (Fig. 37-2). The cartilaginous spinous processes, posterior subarachnoid space, and the dura mater are posterior to the spinal canal. Anterior to the spinal cord are the anterior subarachnoid space and vertebral bodies. The hypoechoic paravertebral muscles can be noted adjacent to the vertebral arches.
Figure 37-1. ![]() Normal longitudinal anatomy of the spinal cord. A. Longitudinal scan through the lower thoracic and upper lumbar region shows the hypoechoic cartilaginous spinous processes (p), echogenic posterior dura mater (d), hypoechoic fluid in the posterior subarachnoid space (psf), posterior surface of the spinal cord (arrowheads), hypoechoic cord (C) with central echogenic complex (open arrows), anterior surface of the cord (arrows), hypoechoic fluid in the anterior subarachnoid space (asf), and echogenic vertebral bodies (v). B. Longitudinal scan through the distal cord shows the smoothly tapering conus medullaris (CM), nerve roots (arrows), and the filum terminale (F). L1, first lumbar vertebral body; L2, second lumbar vertebral body. C. Longitudinal scan in another neonate shows a normal tapered conus medullaris (CM) and the most distal part (arrowhead) of the filum terminale (F). The filum terminale extends to the level of the S1 vertebral body (arrow). D. Longitudinal extended field of view image shows the conus medullaris (CM) and the entire extent of the filum terminale (F)
Normal longitudinal anatomy of the spinal cord. A. Longitudinal scan through the lower thoracic and upper lumbar region shows the hypoechoic cartilaginous spinous processes (p), echogenic posterior dura mater (d), hypoechoic fluid in the posterior subarachnoid space (psf), posterior surface of the spinal cord (arrowheads), hypoechoic cord (C) with central echogenic complex (open arrows), anterior surface of the cord (arrows), hypoechoic fluid in the anterior subarachnoid space (asf), and echogenic vertebral bodies (v). B. Longitudinal scan through the distal cord shows the smoothly tapering conus medullaris (CM), nerve roots (arrows), and the filum terminale (F). L1, first lumbar vertebral body; L2, second lumbar vertebral body. C. Longitudinal scan in another neonate shows a normal tapered conus medullaris (CM) and the most distal part (arrowhead) of the filum terminale (F). The filum terminale extends to the level of the S1 vertebral body (arrow). D. Longitudinal extended field of view image shows the conus medullaris (CM) and the entire extent of the filum terminale (F)
The spinal cord is largest in the cervical and lumbar regions and smallest at the thoracic level. In infants 1 to 3 months of age, the sagittal diameters of the cervical, thoracic, and lumbar portions of the cord are 5.3 ± 0.28, 4.4 ± 0.42, and 5.8 ± 0.66 mm, respectively. The cervical enlargement corresponds to the origin of the nerve roots that supply the upper extremities. The lumbar expansion reflects the large number of nerve roots supplying the lower extremities.
The normal conus medullaris in neonates is nearly always located above the L2–L3 disc space (Fig. 37-1
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree