, Joon Woo Lee1 and Jong Won Kwon2
(1)
Department of Radiology, Seoul National University Bundang Hospital, Seongnam, Kyonggi-do, Republic of Korea
(2)
Department of Radiology, Samsung Medical Center, Seoul, Republic of Korea
Abstract
Spinal vascular malformations consist of dural arteriovenous (AV) fistulae, spinal cord arteriovenous malformation, and juxtamedullary (perimedullary) arteriovenous fistula. Intramedullary cavernous hemangioma is also a type of congenital spinal vascular malformation. Spinal vascular malformations can be differentiated into true congenital lesions and acquired lesions, the latter being the dural arteriovenous (AV) fistulae, whereas arteriovenous malformations (AVM) and cavernous hemangiomas belong to the congenital lesions of the spine.
Spinal vascular malformations consist of dural arteriovenous (AV) fistulae, spinal cord arteriovenous malformation, and juxtamedullary (perimedullary) arteriovenous fistula. Intramedullary cavernous hemangioma is also a type of congenital spinal vascular malformation. Spinal vascular malformations can be differentiated into true congenital lesions and acquired lesions, the latter being the dural arteriovenous (AV) fistulae, whereas arteriovenous malformations (AVM) and cavernous hemangiomas belong to the congenital lesions of the spine.
15.1 Vascular Anatomy and Imaging Modalities
The spinal cord blood supply consists of one anterior and two posterior spinal arteries. At the lower cervical and upper two thoracic cord, the anterior spinal artery (ASA) is supplied by two to four anterior radicular arteries that arise from the ascending cervical, deep cervical, vertebral, and supreme intercostal arteries. In the midthoracic cord, radicular arteries are less prominent. The thoracolumbar region is supplied by the artery of Adamkiewicz (Krings et al. 2007). The ASA provides approximately 70 % of the cord blood supply via deep penetrating arteries. There is no anastomosis within the cord, and these penetrating arteries are end arteries. The posterior portion of the spinal cord (about 30 %) is supplied by the two posterior spinal arteries, which form a plexus and variable arterial networks.
Spinal vascular malformations consist of dural arteriovenous (AV) fistulae, spinal cord arteriovenous malformation, and juxtamedullary (perimedullary) arteriovenous fistula (Table 15.1). Intramedullary cavernous hemangioma is also considered as a type of congenital spinal vascular malformation. Depending on the type of vascular malformation, initial symptoms may vary between acute intramedullary or subarachnoid hemorrhages and subacute venous congestion resulting in progressive myelopathy. The steal phenomenon and space-occupying effect of the vascular malformations are also possible pathomechanisms. While acute manifestations of spinal vascular malformations are diagnosed early in the course of the disease, the subacute venous congestion might result in nonspecific neurologic symptoms and delayed diagnosis.
When spinal vascular malformations are suspected, MRI should be the first diagnostic modality. MRI can detect intramedullary lesions such as edema or venous congestion, intramedullary hemorrhages, intradural extramedullary lesions such as subarachnoid hemorrhage or dilated vessels, and possible extradural manifestations of spinal vascular malformations. MR imaging should be able to identify the location of the AVM in relation to the spinal cord and the dura. On MRI, however, the AVM type cannot be differentiated. Spinal MRI still has possible artifacts, such as pulsation artifacts (which should not be mistaken for dilated epidural vessels), truncation artifacts (which should not be mistaken for syringohydromyelia), or chemical shift artifacts. MR angiography is a helpful tool to find out the diagnosis although conventional spinal angiography remains the diagnostic modality of choice.
Conventional spinal angiography is necessary to define the exact type of vascular malformation and to plan the appropriate therapy. A complete spinal angiography includes all vessels that may feed the spinal cord, i.e., all intercostal and lumbar segmental arteries, cervical feeders including both vertebral arteries, the thyrocervical and costocervical trunk, the ascending cervical artery, and the iliolumbar arteries.
Table 15.1
Classification of Spinal Vascular Malformations
Type | Dural AVF | Spinal cord AVM | Perimedullary AVF | Cavernoma |
|---|---|---|---|---|
Etiology | Acquired | Congenital | Congenital | |
Feeding artery | Radiculomeningeal (dural branch of radicular artery) | Radiculomedullary (anterior spinal) or radiculopial (posterior spinal) | Not applicable | |
Draining vein | Radicular vein, perimedullary veins (retrograde) | Intramedullary and superficial spinal cord veins, epidural venous plexus (antegrade) | Not applicable | |
Pathophysiology | Chronic venous congestion | Intramedullary or subarachnoid hemorrhage, chronic venous congestion, mass effect | Hemorrhage and progressive myelopathy | |
Age of onset (years) | 40–60 | <20 | 20–40 | 20–60 |
Location | Dura, thoracolumbar level | Intramedullary | Surface of the cord | Intramedullary |
Imaging | Perimedullary dilated vessels, cord edema, cord enhancement | Intramedullary nidus, well-defined serpentine flow voids within the cord | No nidus, dilated vessels at the surface of the cord, venous congestion, hemorrhage, mass effect | Intramedullary discrete mass, hemosiderin deposit |
Therapy | Surgery or glue embolization | Particle or glue embolization | Type I: surgery; type II, III: coil embolization | Surgery |
15.2 Dural Arteriovenous (AV) Fistula
Dural arteriovenous fistula (DAVF) is an abnormal direct connection (fistula) between a meningeal artery (dural branch of radicular artery) and a meningeal vein or dural venous sinus. Spinal dural arteriovenous fistulas (SDAVFs) are the most common spinal vascular malformation and can result in progressive myelopathy. Usually, they become symptomatic in elderly men and are typically located at the lower thoracolumbar level. SDAVFs are presumed to be acquired lesions; however, the exact etiology is not known. The AV fistula between the radiculomeningeal artery and the radicular vein is located inside the dura mater close to the spinal nerve root. The increase in the pressure of perimedullary venous plexus diminishes the AV pressure gradient and leads to venous congestion, cord edema, and the clinical results of chronic hypoxia and progressive myelopathy (Krings et al. 2005). The symptoms of venous congestion are nonspecific and include sensory disturbance, paraparesis, lower back pain, impotence, and sphincter disturbance. These neurologic symptoms are progressive with time and are often ascending, and bowel and bladder incontinence and urinary retention can be developed. Because of the slowly progressive course of the disease and the unspecific symptoms, diagnostic imaging often occurs too late.
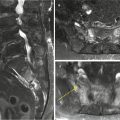
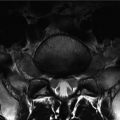
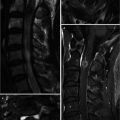
On MR imaging, perimedullary dilated vessels, cord edema, and cord enhancement are important diagnostic features of SDAVFs (Koenig et al. 1989). The dilated and coiled perimedullary vessels can be seen on the T2-weighted images as flow voids, which are often more prominent on the dorsal surface compared with the ventral surface. On T2-weighted images, the cord edema is shown as ill-defined central hyperintensity over multiple segments that are often accompanied by hypointense rim, most likely representing deoxygenated blood within the dilated capillary vessels surrounding the congestive edema (Hurst and Grossman 2000). In the further course of the disease, the cord will become atrophic (Krings and Geibprasert 2009). The swollen cord is slightly hypointense and enlarged on T1-weighted images. On postcontrast study, diffuse enhancement may be seen within the cord as a sign of chronic venous congestion with a breakdown of the blood–spinal cord barrier and necrotic transformation of the spinal cord (De Marco et al. 1990).
Spinal angiography is necessary to determine the exact level of the fistula and to confirm the feeding artery and the draining veins. After injection into the segmental artery feeding the AV fistula, the early venous filling and the retrograde opacification of the radiculomedullary veins are visualized. Often an extensive network of dilated perimedullary veins is visible. This network may even recruit supply from dural arteries that ascend or descend from adjacent radiculomeningeal arteries.
15.3 Spinal Cord Arteriovenous Malformation (AVM)
Spinal cord AVMs (glomerular AVMs, plexiform or nidus-type AVMs) are the most often encountered spinal cord AVMs (20–30 % of all spinal vascular shunts), with a nidus resembling closely those of a brain AVM (Rosenblum et al. 1987). This type of malformation usually is located intramedullary but may extend to dorsal subpial; surface. Because of the many anastomoses between the anterior and posterior arterial feeding system of the spine, these AVMs are typically fed by multiple arteries derived from both the anterior and posterior system. Drainage is into dilated spinal cord vessels. Associated aneurysms of the feeding arteries and the nidus are common. The conus medullaris AVM represents a distinct type located on the conus medullaris or cauda equina and can extend along the filum terminale.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree