Spine(I)
Physiologic Curves of the Spine in the Sagittal Plane
Cervical Lordosis
The degree of cervical lordosis can be measured on a lateral radiograph of the cervical spine or full spine. The most common technique is to measure the angle between a reference line through the atlas and a reference line parallel to the lower endplate of the C7 vertebra ( Fig. 8.1 ).
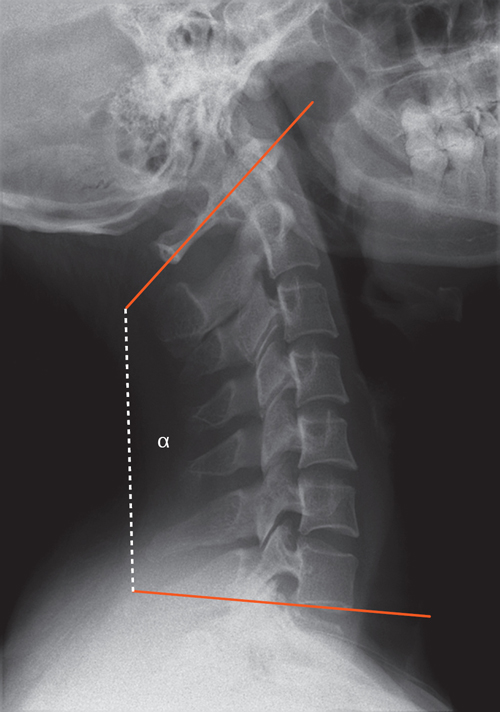
Cervical lordosis
• Mean value: | 40° |
• Normal range: | 35–45° |
Positioning the patient for a lateral radiograph of the cervical spine, with the arms and shoulders drawn downward, often alters the posture in a way that straightens the physiologic lordosis of the cervical spine. As a consequence, decreased cervical lordosis on a lateral radiograph should be considered abnormal only when interpreted within the context of other findings.
Thoracic Kyphosis
Thoracic kyphosis is evaluated on a lateral radiograph by measuring the angle between the upper endplate of the T4 vertebra and the lower endplate of the T12 vertebra ( Fig. 8.2 ). This angle is highly variable. Stagnara et al reported the following normal values:
Thoracic kyphosis
• Mean value: | 37° |
• Normal range: | 30–50° |
Lumbar Lordosis
Lordosis of the lumbar spine can be quantified on lateral radiographs. A common technique is to measure the angle formed by the upper endplate of L1 and the upper endplate of S1 or the lower endplate of L5 ( Fig. 8.3 ).

Lumbar lordosis (measured between L1 and L5)
• Mean value: | 43° |
• Normal range: | 14–69° |

Scoliosis
Cobb Angle
The American Scoliosis Research Society (ASRS) recommends the Cobb method as the standard measuring technique for quantifying spinal curvature in the frontal plane to obtain uniform and comparable values.
The measurement is performed on a standing anteroposterior (AP) radiograph of the full spine. The Cobb angle is measured between the vertebral bodies that are most tilted toward the concavity of the curve, or between the upper and lower endplates of these “end vertebrae” ( Fig. 8.4 ). By definition, the reference lines are drawn along the superior endplate of the upper end vertebra and the inferior endplate of the lower end vertebra. The angle formed by lines drawn perpendicular to the reference lines is the Cobb angle.

The end vertebrae of a spinal curve may be identical with the neutral vertebrae. The neutral vertebra is defined as the vertebral body between two curves that is the least rotated and has parallel endplates. Often, the neutral vertebrae are located one or two vertebrae farther away from the apical vertebra than the end vertebrae. The apical vertebra, which forms the apex of the curve, is the vertebral body that is the most rotated and shows the greatest deformity.
Ferguson Angle
The Ferguson angle can be determined as an alternative to the Cobb angle. This measurement starts by identifying the end vertebrae and apical vertebra of the spinal curve. The end vertebrae are the vertebral bodies in the upper and lower parts of the curve that appear the most tilted in the frontal plane. The apical vertebra lies at the apex of the curve and shows the greatest degree of rotation and deformity but the least amount of tilt. The centers of the end vertebrae and neutral vertebra are found as shown in Fig. 8.5 . The centers of the end vertebrae, which have near-parallel upper and lower endplates, are located by finding the intersection of diagonal lines through the vertebral body. Because the apical vertebra is more deformed, its center is defined by the intersection of lines bisecting the sides and endplates of the vertebral body. Two lines are then drawn connecting the centers of the end vertebrae and apical vertebra. These lines intersect at an angle, the complement of which equals the Ferguson angle ( Fig. 8.5 ).

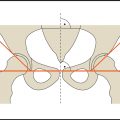
Risser Sign
The Risser sign can be used to assess skeletal maturity on a full-spine radiograph without the need for additional views. Risser observed in 1958 that ossification of the iliac apophysis begins as a bony “cap” on the anterolateral aspect of the iliac crest and progresses posteromedially toward the spine. Fusion of the apophysis to the ilium then progresses in a reverse direction.
Risser did not divide this process into grades or stages in his original publication. As a result, the classifications that appeared in later publications and textbooks show considerable variation. The classification shown in Fig. 8.6 is widely used and divides the iliac apophysis into fourths.
Risser recognized that ossification of the vertebral apophyses roughly paralleled the ossification of the iliac apophyses, so that the Risser sign could be used to assess the remaining growth potential of the spine. Because scoliosis tends to progress during the adolescent growth spurt, a higher Risser stage correlates with a more favorable prognosis.
The apophyses on the iliac crest appear ~ 4 months after the peak of the adolescent growth spurt (age 12–15 years), which roughly coincides with menarche in females. By the time the apophysis starts to fuse with the iliac crest, marking the transition to stage 5, the adolescent growth spurt is completed. Very little additional growth occurs after that time (no more than 1–2 cm of longitudinal spine growth). Definitive fusion of the iliac apophysis to the ilium takes ~ 2 years on average and is generally complete by 21–25 years of age.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree