Gross and Microscopic Anatomy
The spleen is a reticuloendothelial lymphoid organ located in the left upper abdomen, posterolateral to the stomach, tail of the pancreas, and colic flexure. The adult spleen is 10 to 12 cm in length and weighs an average of 168 g in the adult man and 135 g in the adult woman. Splenic weight positively correlates to height, body weight, body mass index, and body surface area. The spleen is most commonly located between the 9th and 12th ribs with its long axis in line with the 11th rib.
The visceral peritoneum is reflected at its hilum to form two “pedicles”; one is reflected over the gastrosplenic ligament, and the other is reflected posteriorly over the tail of the pancreas and lienorenal ligament ( Fig. 102-1 ). The tail of the pancreas lies within the lienorenal ligament together with the splenic vessels, lymphatics, and nerves and extends to the splenic hilum.
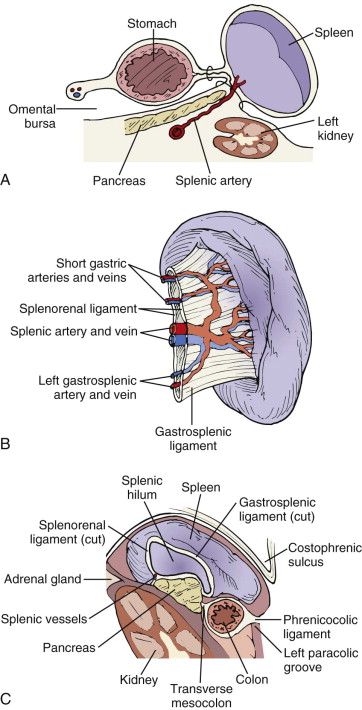
The superior convex surface of the spleen abuts the concavity of the diaphragm and is closely related to the posterior costophrenic recess and the left lung base. The posterior aspect of the spleen lies adjacent to the left adrenal gland or left kidney, and in up to one third of normal cases, part of the spleen is retrorenal. The anterior surface is related to the splenic flexure of the colon and connected to it by the splenocolic ligament. The splenophrenic, splenorenal, and gastrosplenic ligaments also fix the spleen in its position. The visceral or concave surface of the spleen is related to the stomach and tail of the pancreas in addition to the left kidney and the colon. The splenic hilum occupies approximately 25% to 33% of the splenic surface area.
The splenic artery, a branch of the celiac axis, runs a transverse and often tortuous course along the upper border of the pancreas to reach the splenic hilum, where it divides into five or more major branches. The splenic vein is formed at the splenic hilum and runs in the lienorenal ligament anterior to the left kidney, the left diaphragmatic crus, and the aorta in a groove along the dorsal aspect of the pancreas ( Fig. 102-2 ). It joins the inferior mesenteric vein and then the superior mesenteric vein behind the head of the pancreas to form the portal vein. The spleen provides 40% of the blood volume of the portal circulation. The lymphatic vessels are subcapsular and are formed by the drainage of large trabecular tributaries. These vessels drain into the pancreaticolienal nodes at the splenic hilum.

The framework of the spleen consists of collagenous fibrous and elastic tissue forming the capsule (which is less that 1.5 mm thick), trabeculae, and reticular fibers ( Fig. 102-3 ). Blood enters the trabeculae through splenic arterial branches and exits through central arteries (in the white pulp) that are surrounded by the periarteriolar lymphoid sheaths, whose enlargements at irregular intervals are known as malpighian bodies.

The lymphatic sheaths and follicles make up the white pulp of the spleen. The blood vessels transport blood to the sinusoids in the red pulp. Capillaries may open directly into sinusoids or may first pass through spaces in the red pulp. The red pulp performs the phagocytic function of the spleen.
The spleen has between two and five arterial segments, with the avascular plane running parallel to the short axis of the spleen. There are typically two polar arteries and variable segmental arteries supplying the interpolar portion.
The splenic nerve supply is derived from the celiac plexus. It is located along the splenic artery and sends postganglionic sympathetic fibers that innervate the splenic white pulp. These fibers distribute with the vascular and trabecular systems and associate mainly with the central artery and its branches, the periarteriolar lymphatic sheath, the marginal sinus, and the parafollicular zone, with occasional fibers in the follicles.
Physiology
About 4% of the cardiac output or 150 mL of blood per minute flows through the spleen. This amounts to 350 L of blood per day. The normal transit time of blood in the spleen is 20 to 25 seconds.
The spleen discriminates between normal and abnormal cells and selectively sequesters abnormal and aged red or white blood cells and platelets. The microcirculation of the spleen is thought to direct 10% of splenic arterial blood directly into the venous sinuses and 90% through the red pulp, whose endothelial pores and macrophages remove abnormal particles. Abnormal red blood cells, viruses, bacteria, nuclear remnants (Howell-Jolly bodies), and parasites are removed, with normal erythrocytes left intact. It is not certain what factors sensitize an aged blood cell to splenic destruction; however, it has been suggested that aging erythrocytes have stiffened membranes, which slows or halts their passage through the narrow network of splenic cords, making them an easy target for phagocytosis. About 30% of platelets are normally sequestered within the spleen. When splenomegaly is present, up to 80% of platelets may be sequestered.
The role of the spleen in the immune response is incompletely understood, but it is important in the initiation of humoral and cellular immune responses. The lymphatic tissue in the spleen is unique in that the white pulp of the spleen is perfused by blood rather than by lymph. Thus, it is able to respond rapidly to antigens introduced into the bloodstream. The spleen produces a tetrapeptide known as tuftsin that coats leukocytes and facilitates phagocytosis. The absence of tuftsin in splenectomized patients may contribute to the increased incidence of infection reported in these patients by impairing opsonization of bacteria. The spleen is the main site of immunoglobulin M antibody synthesis. Serum immunoglobulin M levels have been shown to decrease significantly after splenectomy.
Whereas the storage function is not considered to be well developed in the human spleen, it can on average contain 200 to 250 mL of blood and can maintain red blood cell volume in the face of bleeding unless the blood loss is marked. Red blood cells are released into the circulation by splenic contraction, which is controlled by the actions of postganglionic fibers on the capsule and trabeculae. Platelets and white blood cells are also stored within the spleen. In splenomegaly (increased storage), pancytopenia can occur; in asplenia (no storage), one may see panthrombocythemia.
Radiologic Anatomy and Technique
Splenic size and morphology can be assessed by physical examination or imaging studies. Palpation and percussion of the spleen can be complementary to imaging but are insensitive. Individuals with a large body habitus and up to 10% of normal children do have palpable spleens. Thus, there is an important role for radiographic imaging in diagnosis of suspected splenic disease.
Plain Film Radiography
The spleen ( Fig. 102-4 ) is often partially outlined on plain films by fat in the greater omentum and distal transverse mesocolon and by the adjacent air-filled stomach or colon. The ventral surface of the spleen may be outlined by fat on lateral views of the chest or abdomen, particularly if the spleen is enlarged. The normal spleen can be visualized in fewer than 100 of 500 (20%) plain films, and the splenic tip can be seen in about 44% of cases. The long axis of the spleen usually parallels the posterior ribs and generally does not project significantly below the costal margin. Plain film radiography is useful for detection of moderate or massive splenomegaly and splenic calcifications as commonly seen in granulomatous disease (tuberculosis, histoplasmosis, brucellosis). Curvilinear calcifications may be seen with chronic hematoma, healed abscess, and cysts. Thorotrast deposition, although of historical interest only, is also usually visible on plain films as a fine reticular pattern.

Nuclear Scintigraphy
Splenic scintigraphic evaluation is commonly performed with technetium Tc 99m sulfur colloid ( Fig. 102-5 ). Indications include detection of congenital abnormalities of the spleen and assessment of splenic size, accessory or residual splenic tissue, heterotopic splenic tissue, splenic atrophy, and asplenic states. Splenic lesions larger than 1 cm may be evaluated with planar imaging, but smaller lesions require single photon emission computed tomography (SPECT) or SPECT/CT.

Positron Emission Tomography
Fluorine-18 fluorodeoxyglucose ( 18 F-FDG) positron emission tomography/computed tomography (PET/CT) is established as a powerful imaging tool for cancer detection and monitoring of response to therapy. There is faint radiotracer uptake in normal splenic tissue ( Fig. 102-6 ). Diffuse increased splenic uptake can be present with the use of marrow-stimulating factors and hematopoietic disorders, as the spleen is a site of extramedullary hematopoiesis. Focal or diffuse pathologic increased 18 F-FDG uptake is present in malignant neoplasms that involve the spleen.

Angiography
The splenic artery is approximately 13 cm in length (range, 8-32 cm). Trifurcation of the celiac trunk into the hepatic, splenic, and left gastric arteries is considered conventional and can be found in 85% of humans. The splenic artery usually originates just distal to the left gastric artery. In 15% of cases, all three branches of the celiac trunk arise at the same point. Normal variations include origin of the splenic artery from the ventral or right surface of the celiac axis and origin from the aorta or superior mesenteric artery. A branch supplying the upper splenic pole may originate separately from the celiac axis, giving the appearance of a double splenic artery. The splenic artery can be divided into suprapancreatic, pancreatic, prepancreatic, and perihilar segments. Its tortuosity is variable and increases with age. The most tortuous segment is usually the pancreatic segment, which runs along the dorsal surface of the pancreas and gives off small pancreatic branches. The pancreatic tail and the perihilar segment run between the spleen and the tail of the pancreas.
There are two basic splenic shapes based on arterial configuration: the distributed type and the compact type. The distributed configuration (70% of cases) consists of a short splenic artery with numerous small branches that penetrate the splenic hilum in a distributed fashion. The compact configuration (30% of cases) has a narrow hilum in which the arterial branches are few and large.
The splenic artery also supplies portions of the pancreatic body and tail. The dorsal pancreatic artery arises from the first 1 to 3 cm (suprapancreatic segment) of the splenic artery and the greater pancreatic artery (arteria pancreatica magna), which arises from the middle segment of the splenic artery and supplies the tail of the pancreas. Another branch, the artery of Buhler, may course inferiorly to communicate with the superior mesenteric artery. The short gastric arteries and the left gastroepiploic artery usually arise just proximal to the first division of the splenic artery.
In the parenchymal phase of splenic arteriography, splenic density is dependent on the ratio of splenic volume to the volume of contrast material injected. It is often homogeneous or slightly speckled. Venous anatomy is normally visualized about 7 seconds after arterial injection. Splenic venous anatomy can also be demonstrated with splenoportography.
Ultrasound
Ultrasound can be useful in evaluating the spleen, which is best scanned in the left anterior oblique, right lateral decubitus, or prone position. Ultrasound evaluation is best performed with a curved array transducer with a median frequency of 3 to 5 MHz. Use of a subcostal or oblique intercostal plane can increase the sonographic window. An anterior approach is often limited by gastric or colonic gas. Transverse and longitudinal (coronal) imaging should be obtained ( Fig. 102-7 ). Full or varying degrees of inspiration will improve visualization of the paradiaphragmatic portion of the spleen, which is the most difficult to image. It is often helpful to fill the stomach with fluid for scanning in the supine position. The transducer may be moved in an arc along the intercostal space or in a sector motion. A convex transducer may improve visualization of the “blind areas” adjacent to the dome of the diaphragm. Care should be taken in differentiating a prominent lateral segment of the left lobe of the liver, which may wrap around the spleen. When there is a paucity of intra-abdominal fat in thin patients, as in children and young women, the lateral segment of the left lobe may give the appearance of a pseudoperisplenic lesion. This can simulate a fluid collection superior and lateral to the spleen.











