Splenic Trauma
The spleen is the most commonly injured organ in blunt abdominal trauma. It receives 5% of the cardiac output, accounts for 25% of the total reticuloendothelial cell mass, and plays a major role in clearing the plasma antigens. Recognition of this fundamental role in the immune response during the last century has led to greater efforts to preserve the spleen after injury. Nonoperative management is now widely accepted in carefully selected, hemodynamically stable patients. Development of sophisticated and accurate diagnostic imaging techniques, such as multislice computed tomography (CT), has been a major driving force behind these changes. The accurate diagnosis of splenic injury has therefore assumed an increasingly important role in the evaluation of the traumatized patient. It is very difficult to exclude solid organ injury in patients with blunt abdominal trauma without CT. CT greatly facilitates selection of patients who are treated nonoperatively by allowing accurate identification and characterization of splenic injuries as well as of other associated injuries. Both CT and ultrasound are important in the immediate follow-up of these patients, although ultrasound may fail to demonstrate injury in the absence of hemoperitoneum.
Epidemiology
The spleen can be injured by various mechanisms, including blunt abdominal trauma, penetrating injuries, and iatrogenic and intraoperative accidents. Splenic injury accounts for approximately 25% of all solid abdominal organ injuries. Motor vehicle accidents and motor sports produce most splenic injuries, followed by direct blows and falls. Associated injuries of the central nervous system, liver, kidney, and hollow viscera occur in 10% to 40% of blunt splenic injuries, and these may alter therapeutic options.
Penetrating trauma of the chest or abdomen can also result in splenic injury. Whereas penetrating trauma may involve the spleen, the spleen is less frequently injured compared with the small and large intestine. Up to 40% of all splenectomies are performed for iatrogenic injury. The risk of splenic injury is highest during left hemicolectomy (1%-8%), open antireflux procedures (3%-20%), left nephrectomy (4%-13%), and exposure and reconstruction of the proximal abdominal aorta and its branches (21%-60%); most iatrogenic injuries result from excessive retraction and disruption of ligamentous attachments. Penetrating iatrogenic splenic injuries during interventional procedures involving the left kidney can occur because of the variable relationship of the spleen and the left kidney. Splenic injury is an uncommon complication of colonoscopy that may be unsuspected clinically but evident on CT scans.
Clinical Findings
The clinical diagnosis of splenic injury after blunt abdominal trauma can be difficult. As many as 40% of patients with significant intra-abdominal trauma may have no apparent signs or symptoms on their initial presentation to the emergency department. In the setting of blunt abdominal trauma, non-CT criteria can identify only 12% of patients without intra-abdominal injuries and 22% of patients without major injuries. Laboratory analysis in combination with physical examination findings can contribute significantly to the identification of intra-abdominal injuries after blunt trauma. However, diagnostic clues can be masked in the presence of intracranial or spinal injury, shock, or intoxication. One study has shown clinically significant findings on CT in 19% of trauma patients with no obvious signs of chest or abdominal injury.
The patient’s complaints may include left upper quadrant tenderness or referred left shoulder pain (Kehr’s sign), which may be elicited best by placing patients in the Trendelenburg position. Rib fractures are found in 7% to 10% of patients with multiple trauma. Hypotension and overt shock occur in approximately 30% to 40% of patients with splenic injuries, although this number continues to decline with advances in field resuscitation and transport. Signs of persistent intraperitoneal hemorrhage or hemodynamic instability are clear indications for surgery. Many surgeons continue to advocate the use of diagnostic peritoneal lavage (DPL) for the evaluation of splenic injuries, especially in the unstable or multiply injured patient. The relative value of DPL compared with CT continues to be debated; however, a major limitation of DPL is its lack of specificity as the injured organ may be difficult to identify and the grade of injury cannot be determined. Care should also be exercised when DPL is performed before abdominal CT as the lavage fluid may reduce attenuation of hemoperitoneum because of dilution.
Pathophysiology
The spleen is particularly susceptible to injury after blunt trauma because of its complex ligamentous attachments and spongy parenchymal consistency. The spleen is firmly attached to the retroperitoneum by the lienorenal and phrenicolienal ligaments. It is also attached to the mobile colon and stomach by the gastrolienal and cololienal ligaments. The spleen is divided into four or six segments by arterial supply, whereas the venous system is highly anastomotic and does not follow a predictable segmental anatomy. The arterial branch vessels enter the spleen perpendicular to the long axis, allowing segmental resection ( Fig. 106-1 ). The spleen is enclosed within a thin capsule derived from the peritoneum. In pediatric patients, the splenic capsule is relatively thicker and contains more elastic and contractile elements.

The spleen can be injured by sudden compression or contrecoup mechanisms during rapid deceleration. In deceleration injuries, the mobility of the stomach and the transverse colon is transferred to the spleen, which results in ligamentous-capsular avulsions or vascular injury to the pedicle or short gastric vessels. Blunt compression can occur from a direct blow or transmitted shock wave and usually results in parenchymal injuries and venous bleeding along segmental anatomic lines. With greater energy transfer, blunt injury does not respect segmental anatomy, and stellate fractures occur with extensive arterial and venous bleeding. Injuries that result in parenchymal hematomas with an intact capsule are less common than was originally believed but may account for the 1% to 2% incidence of delayed splenic rupture.
The sequelae of penetrating splenic injury depend on the wounding instrument and its trajectory. In contrast to blunt trauma, penetrating trauma does not respect segmental anatomy and tends to have more vascular disruption. Penetrating trauma also has a higher incidence of associated organ injury, including the gut, which typically necessitates exploration. An abnormal spleen is prone to injury by trivial trauma.
The enlarged spleen is more prone to blunt injury and is exposed beneath the rib cage. Splenomegaly can result from a variety of disease states, including portal hypertension, blood dyscrasias, infection, and lymphoproliferative disorders.
Radiologic Findings
Imaging of patients with abdominal trauma is secondary to initial resuscitation efforts and clinical evaluation. Although plain films are part of most standard trauma protocols, the appropriateness of cross-sectional imaging depends on the clinical situation. Hemodynamically unstable patients or individuals with critical nonabdominal injuries that require immediate attention are not suitable candidates for CT and are typically evaluated by DPL or are explored immediately. However, in hemodynamically stable patients, imaging can play an invaluable role in detecting and staging splenic injury. Imaging can also be useful in the follow-up and postoperative evaluation of these patients.
Computed Tomography
CT has become the “gold standard” for the diagnosis of splenic injuries after trauma. CT has an accuracy exceeding 95% in the detection of splenic injuries. However, these impressive results can be obtained only by use of meticulous CT technique. Streak artifacts from the patient’s arms, external wires and hardware, nasogastric tubes, and gastric distention or gastric air-fluid levels should be avoided or minimized. Contrast-enhanced multislice CT is the current method of choice for evaluation of trauma patients with suspected abdominal injury in most institutions. Multislice CT scanning with bolus technique is preferred to optimize injury detection and to minimize delay within the department. Multislice scanners with fast tube rotation minimize scanning time and motion artifact.
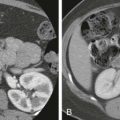
Assessment of splenic injury should include evaluation for hematoma, extent of laceration, active extravasation of contrast material, and associated vascular injuries. Splenic hematomas are hyperdense relative to the splenic parenchyma on unenhanced CT and generally hypodense on contrast-enhanced CT. Splenic hematomas may be intraparenchymal, subcapsular, or perisplenic. Intrasplenic hematomas ( Fig. 106-2 ) typically appear as hypodense areas within the splenic parenchyma after administration of contrast medium. These intrasplenic hematomas may be nearly isodense in some cases, particularly after inadequate administration of contrast material.

Splenic lacerations on CT appear as linear, low-attenuation foci that may not extend completely across the spleen ( Fig. 106-3 ). Lacerations may be single, multiple, or stellate ( Fig. 106-4 ). Splenic fractures ( Fig. 106-5 ) are defined as lacerations that extend completely across the splenic parenchyma and commonly involve the splenic hilum. Intraparenchymal lacerations become smaller and less dense with smoother margins over time. This healing may take weeks, and follow-up CT, particularly in the setting of an uncomplicated clinical course, is not helpful and does not affect management. Follow-up imaging after hospital discharge is not advocated by many centers.



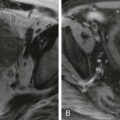
Subcapsular hematomas follow the splenic contour and compress the parenchyma. Subcapsular hematomas ( Fig. 106-6 ) typically appear as crescentic fluid collections along the lateral aspect of the spleen, which may be difficult to distinguish from perisplenic fluid ( Fig. 106-7 ). These hematomas become less dense over time and may mimic free intraperitoneal fluid. However, mass effect on the splenic parenchyma and its location between the enhancing capsule and the parenchyma distinguishes it from free fluid. Subcapsular hematomas usually resolve within 4 to 6 weeks. These hematomas are not associated with delayed splenic rupture and are not an indication for splenorrhaphy.


Severe disruption of the splenic parenchyma results in a “shattered” spleen ( Fig. 106-8 ). Vascular pedicle injuries usually result in significant hemorrhage and cardiovascular instability and are usually not referred for CT evaluation. These patients do have a characteristic CT appearance with nonenhancement of the caudal portion of the spleen and preservation of upper pole perfusion through the short gastric arteries. Active hemorrhage appears as areas of irregular collection of contrast material that can be distinguished from adjacent clot by its density ( Fig. 106-9 ). Extravasated contrast material has a higher mean attenuation than hematoma (132 HU vs 51 HU). In general, contrast material extravasation has a higher likelihood of splenic hemorrhage at laparotomy. Laparotomy in these patients may be avoided by prophylactic embolization of the proximal main splenic artery.


Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree