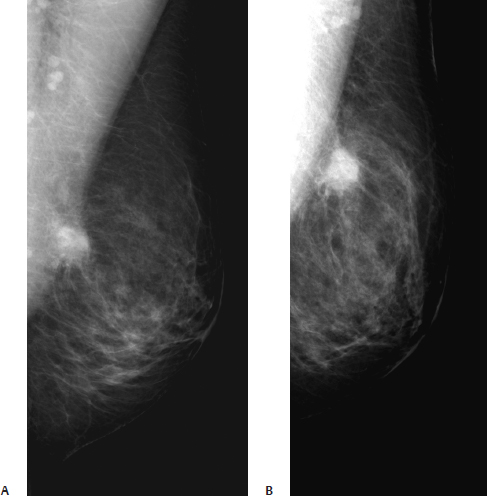
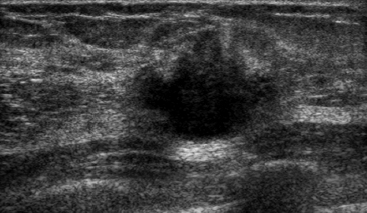
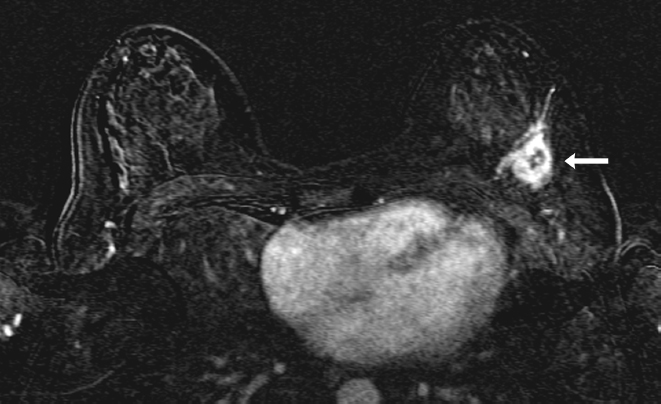
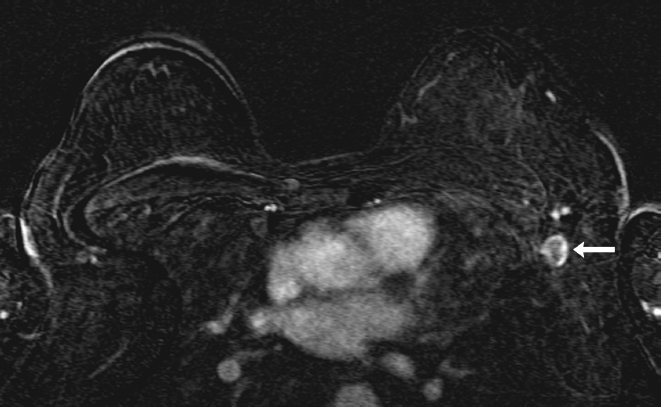
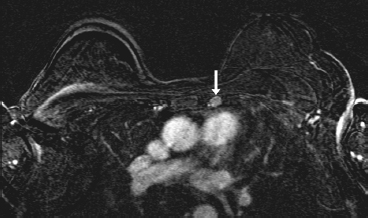
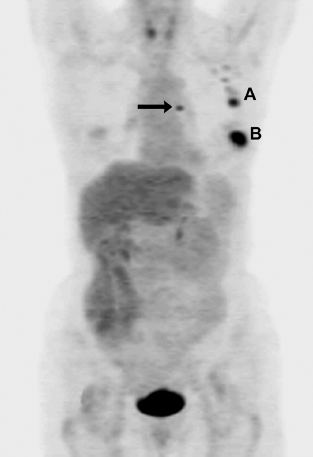
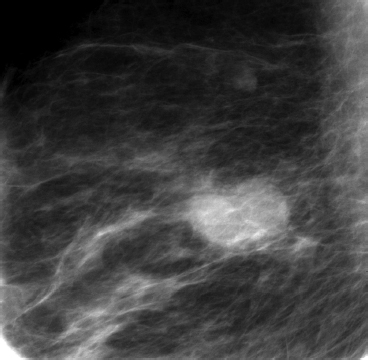
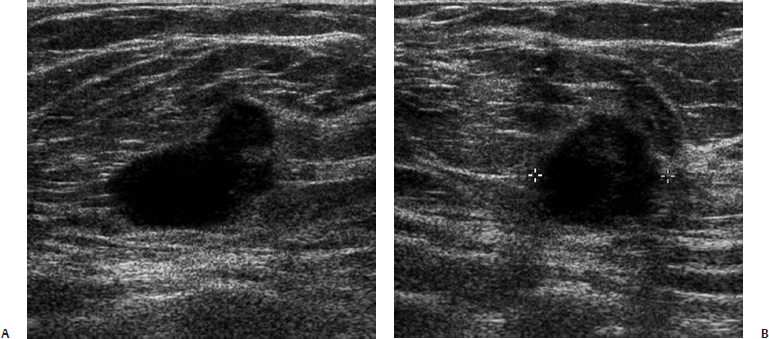
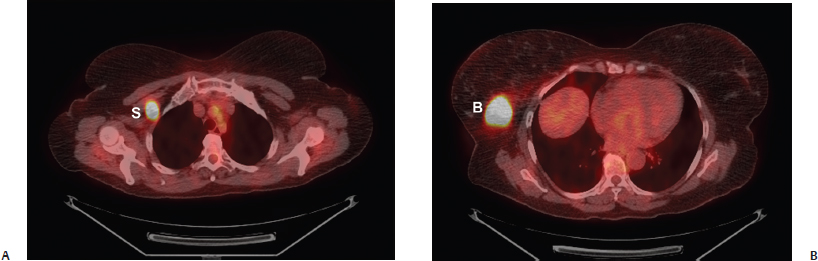
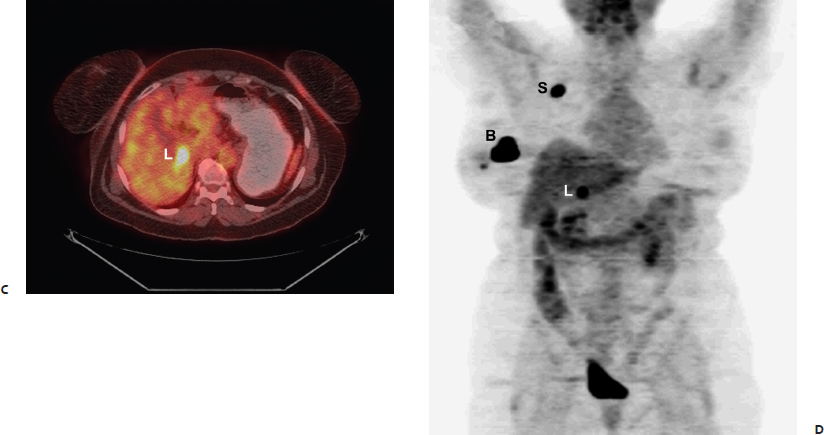
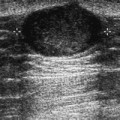
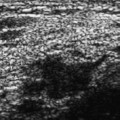
35 Staging A 63-year-old woman presents with a palpable left breast lump. • Firm lump in outer left breast near the 3 o’clock position Mass (Fig. 35.1) • Margin: ill defined • Shape: oval • Density: high Fig. 35.1 In the outer quadrant, there is an ill-defined oval mass. (A) Left MLO mammogram. (B) Left exaggerated craniocaudal (XCC) mammogram. Frequency (Fig. 35.2) • 14 MHz Fig. 35.2 Left breast antiradial sonogram. The mammographic mass and palpable lump correspond to an irregular hypoechoic solid mass near the 3 o’clock position that is associated with spiculations. The mass also distorts the Cooper’s ligament and surrounding glandular architecture. Fig. 35.3 Dynamic bolus T1-weighted, 2-minute subtraction axial bilateral breast MRI. The MRI is performed to further stage the tumor. The primary malignancy is a rapidly enhancing irregular mass in the left 3 o’clock position (arrow). Fig. 35.4 Dynamic bolus T1-weighted, 2-minute subtraction axial bilateral breast MRI. The MRI identifies an abnormal enhancing left axilla (arrow). Fig. 35.5 Dynamic bolus T1-weighted, 2-minute subtraction axial bilateral breast MRI. An abnormally enlarged internal mammary lymph node is evident (arrow). Fig. 35.6 Maximum projection intensity (MIP) positron emission tomography (PET) image. The PET exam demonstrates the primary malignancy (B) and confirms the presence of abnormal axillary nodes (A) and an internal mammary node (arrow). • Invasive ductal carcinoma • Left mammographic and sonographic mass: BI-RADS assessment category 5, highly suggestive of malignancy • Positron emission tomography (PET) is not recommended for routine staging for patients with early-stage breast cancer because in these patients PET is not as sensitive as sentinel lymph node biopsy for staging axillary metastases. A multicenter trial found that the sensitivity was 61%, and specificity was 80%. Because of a relatively high false-negative rate, sentinel lymph node biopsy or axillary dissection cannot be avoided if the PET scan is negative. PET has a higher sensitivity when the primary breast tumor is large (i.e., > 2 cm) and when the 18F-fluorodeoxyglucose (FDG) uptake of the tumor is high. • PET has been found to be more accurate than computed tomography (CT) for the identification of internal mammary and mediastinal metastases. Eubank WB, Mankoff DA, Takasugi J, et al. 18Fluorodeoxyglucose positron emission tomography to detect mediastinal or internal mammary metastases in breast cancer. J Clin Oncol 2001;19(15):3516–3523 Greco M, Crippa F, Agresti R, et al. Axillary lymph node staging in breast cancer by 2-fluoro-2-deoxy-D-glucose-positron emission tomography: clinical evaluation and alternative management. J Natl Cancer Inst 2001;93(8):630–635 van der Hoeven JJM, Krak NC, Hoekstra OS, et al. 18F-2-fluoro-2-deoxy-D-glucose positron emission tomography in staging of locally advanced breast cancer. J Clin Oncol 2004;22(7):1253–1259 Wahl RL, Siegel BA, Coleman RE, Gatsonis CG; PET Study Group. Prospective multicenter study of axillary nodal staging by positron emission tomography in breast cancer: a report of the staging breast cancer with PET Study Group. J Clin Oncol 2004;22(2):277–285 A 73-year-old woman presents for screening mammography. • Normal exam Mass (Fig. 35.7) • Margin: ill defined and irregular • Shape: oval • Density: high Fig. 35.7 Right MLO spot compression mammogram. There is an oval mass with ill-defined, irregular margins in the upper outer quadrant of the right breast. Frequency (Fig. 35.8) • 14 MHz Fig. 35.8 The mammographic mass corresponds to a sonographically solid, hypoechoic, mildly lobulated mass. The margins are mildly irregular on the antiradial image. (A) Right radial breast sonogram. (B) Right antiradial breast sonogram. Fig. 35.9 Because the patient’s tumor histologically is aggressive, a PET scan is performed, which demonstrates abnormal uptake in the liver (L), right supraclavicular lymph node (S), and right breast (B). The liver and nodal appearance is consistent with metastatic disease. (A) Axial positron emission tomography–computed tomography (PET-CT) of upper chest. (B) Axial PET-CT of lower chest. (C) Axial PET-CT of the abdomen. (D) Maximum intensity projection (MIP) PET image. • A 3.6 cm, high-grade infiltrating ductal carcinoma, estrogen and progesterone receptor negative, with overexpression of HER-2/neu (c-erb-B2) • Right mammographic and sonographic mass: BI-RADS assessment category 4, suspicious; biopsy should be considered. • PET is not recommended as a routine method to stage patients with early-stage breast cancer because they have a low probability of metastatic disease. However, PET has been found to be an excellent method to identify meta-static or recurrent disease. It has been shown to have slightly less than 95% sensitivity and 80 to 90% specificity for recurrent or metastatic disease. • When researchers have retrospectively examined PET scans of patients with more advanced disease, those patients with tumors in the inner breast are more likely to present with isolated extra-axillary disease and experience progressive disease compared with those with tumors in the outer breast. These extra-axillary sites include the brain, supraclavicular region, mediastinal or internal mammary nodes, bone, liver, lung, and pleura. Eubank WB, Mankoff D, Bhattacharya M, et al. Impact of FDG PET on defining the extent of disease and on the treatment of patients with recurrent or metastatic breast cancer. AJR Am J Roentgenol 2004;183(2):479–486
Case 35.1: Staging Locoregional Disease
Case History
Physical Examination
Mammogram
Ultrasound
Other Modalities: MRI and PET (Figs. 35.3, 35.4, 35.5, and 35.6)
Pathology
Management
Pearls and Pitfalls
Suggested Reading
Case 35.2: Staging Advanced Disease
Case History
Physical Examination
Mammogram
Ultrasound
Other Modalities: PET-CT (Fig. 35.9)
Pathology
Management (Mammography and Ultrasound Findings)
Pearls and Pitfalls
Suggested Reading
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree