Author (year)
n
Disease
Targeting
Use of plug
Unilateral or bilateral treatment
Prescription dose (maximum dose, Gy)
Follow-up
Effects
Complication rate (%)
Complication
Pan (1996) [8]
8
Parkinson’s disease
Based on Schaltenbrand and Wahren atlas
Yes
Unilateral
160–180
4.5 months
Tremor disappears in 3 cases, reduction in 3 cases
12.5
Transient hemiparesis and edema
Friedman (1999) [9]
15
Parkinson’s disease 3
7–8 mm anterior to PC, 11–13 mm lateral to ACPC line, 2 mm above ACPC line
No
Unilateral
120–140
3 months
2.1 decrease in TRS
46.7
Edema, etc.
Essential tremor 12
Duma (1999) [10]
38
Parkinson’s disease
6 mm posterior to the midpoint of ACPC, 15 mm lateral to ACPC line, 4 mm superior to ACPC line
No
Unilateral 34
120–160
Median 30 months
Reducing and eliminating tremor in 90 %
2.6
Dysarthria
Bilateral 4
50 % isodose line medially to IC
Duma (2007) [11]
42
Parkinson’s disease
6 mm posterior to the midpoint of ACPC, 15 mm lateral to ACPC line, 4 mm superior to ACPC line
No
Unilateral 38
120–160
Median 30 months
Good or excellent 54 %
1.3
Paresthesia, motor weakness, dysphasia
Essential tremor
Bilateral 4
30 % isodose line medially to IC
Niranjan (2000) [12]
11
Essential tremor 8
25 % of the ACPC distance anterior to PC, laterality 1/2 third ventricle width + 11 mm from ACPC, 2 mm superior to the ACPC line
No (model U)
Unilateral
130–150
Median 6 months
Tremor reduction in all
9.1
Hemiparesis, dysarthria
Multiple sclerosis 3
Mathieu (2007) [13]
6
Multiple sclerosis
25 % of the ACPC distance + 1 or 2 mm anterior to PC, laterality 1/2 third ventricle width + 11 mm from ACPC, 2 or 2.5 mm superior to the ACPC line
No
Unilateral
130–150
Median 27.5 months
Tremor reduction in all
16.7
Hemiparesis
Kondziolka (2008) [14]
31
Essential tremor
25 % of the ACPC distance + 1 mm anterior to PC, laterality 1/2 third ventricle width + 11 mm from ACPC, 2.5 mm superior to the ACPC line. The 20 % isodose line medial to the internal capsule
Yes
Unilateral
130–140
Median 36 months
Improvement in 88.0 %
7.7
Hemiparesis, speech disturbance, dysphagia
Young (2010) [15]
161
Essential tremor
Based on Schaltenbrand and Wahren atlas
No
Unilateral 130
141–152
Mean 44 ± 33 months
Writing, 77 %; drawing, 81 %
8.4
Sensory loss, motor impairment, speech disturbance, etc.
Staged bilateral 42
Lim (2010) [16]
18
Parkinson’s disease 3
25 % of ACPC + 1 mm to PC, 11 mm lateral to third ventricle wall, 2–3 mm above ACPC
Yes
Unilateral
130–140
Mean 19.2 ± 7.3 months
Improvement in tremor rating score ADL score
16.7
Thalamic hemorrhage, sensory disturbance
Essential tremor 15
Ohye (2012) [7]
72
Parkinson’s disease 59
Longitudinal thalamic length 45 %, 2 mm inside external border of internal capsule, 3–4 dorsally to ACPC
Yes
Unilateral
130
24 months
Improvement in 81.1 %
1.4
Motor weakness
Essential tremor 13
Indication of GK Thalamotomy
Indications of GK thalamotomy for the treatment of intractable tremor are determined in accordance with more conventional stereotactic surgery. While DBS or conventional thalamotomy is available, the use of GK thalamotomy has been reserved for specific patients, such as those who are poor candidates for conventional surgery (e.g., due to advanced age or ongoing anticoagulant therapy).
Intractable tremors could be classified as components of ET, PD, or multiple sclerosis. The most common disease treated by GK thalamotomy is ET. ET is a common adult movement disorder, with prevalence estimates derived from population studies ranging from 0.4 to 5 % [17, 18]. The incidence and prevalence of ET both increase with advancing age [18], and conventional thalamotomy or DBS is not often recommended for aged patients with ET.
PD is another indication for GK thalamotomy; however, subthalamic DBS improves symptoms of rigidity, bradykinesia and motor fluctuation, as well as tremor [19]. In a systematic review of PD progression, the non-tremor dominant subtype at disease onset appeared to favor rapid progression to Hoehn and Yahr stage III [20]. Tremor seems to predict a slow progression of PD. If intractable tremor causes significant functional impairment, GK thalamotomy is an option for tremor reduction [7].
Target Coordination
Although the efficacy of GK thalamotomy for intractable tremor has been evaluated, the prescription dose and target selection varied greatly among the studies reviewed (see Table 55.1). Previous studies have selected the ventralis intermedius nucleus (VIM) as the target for treating intractable tremor. In the majority of studies, target determination was based on the anterior commissure-posterior commissure (ACPC) line. Anterior-posterior coordination was 6–8 mm anterior to PC, or 25 % of the ACPC line from PC, while right-left coordination was 11–13 mm lateral to the ACPC line, and rostral-caudal coordination was 2–4 mm above the ACPC line. Anatomical investigation of formalin-fixed human brains indicated the anterior tip of ventroposterior nucleus [21]. Ohye et al. adjusted the tentative target based on the ACPC line, so that the center of the radiation beam would cover 45 % of the longitudinal axis of the thalamus for actual irradiation [22]. No neurophysiological information aids the refinement of the target and is in fact a disadvantage in GK thalamotomy. Sato et al. performed depth recordings around the region of the supposedly optimum target for tremor, as determined in usual thalamotomy, to provide indirect support for GK thalamotomy, and demonstrated a rhythmic discharge time locked to tremor, and the presence of kinesthetic neurons within the expected target area [23]. Extensive experience using stereotactic thalamotomy with microelectrode recordings might support GK thalamotomy, which has the disadvantage of involving no neurophysiological examination.
Tolerance of the Internal Capsule
Accurate lateral coordinates are crucial to prevent radiation injury to the internal capsule. Duma et al. adjusted the 50 % isodose line medially to the internal capsule [24]. Kondziolka et al. retained 20 % of the isodose line of the 4-mm collimator medially to the internal capsule [14]. The tolerance of the internal capsule thus remains unclear. However, Maruyama et al. used diffusion tensor tractography of the pyramidal tract when dose planning of GK surgery for treatment of an arteriovenous malformation and calculated the tolerance of the pyramidal tract [25, 26]. The maximum dose to the pyramidal tract and 20- or 25-Gy volume in the pyramidal tract significantly correlated with the motor complication. Interestingly, the internal capsule was found to be more fragile than the coronal radiation. A plugging technique to reduce the dose of radiation to the internal capsule was applied in several recent studies (Fig. 55.1) [7, 14, 16]. It is now generally accepted that the maximum dose of radiation to the internal capsule should be less than 20–25 Gy.


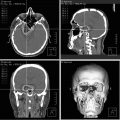
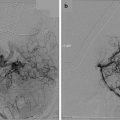
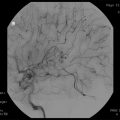
Fig. 55.1
Representative GK thalamotomy treatment plan. Treatment plan (MRI) of right hemisphere GK thalamotomy for intractable left-hand tremor and isodose lines (15 and 50 %) is indicated. The dose to the internal capsule is reduced by using the plugging technique
Prescribed Dose
GK treatment has been commonly performed using a 4-mm collimator. The prescribed dose varied among the different studies (see Table 55.1). Steiner et al. reported that a dose of 150 Gy was necessary for the reproducible creation of a human brain lesion, using an autopsy series of GK thalamotomy that used to treat intractable cancer pain [27]. In the reports published in the early 1990s, a relatively high dose was selected for lesioning; however, in more recent reports, a maximum dose of 130–140 Gy was recommended for thalamotomy using GK [7, 14, 16]. Okun et al. reported five cases with complications of GK thalamotomy, including two cases of bilateral lesioning [6]. Radiation effects were found to have expanded into the internal capsule and mesencephalon, which caused further motor complications and pseudobulbar symptoms. However, the prescribed dose should be noted; the target was irradiated at a maximum dose of 200 Gy. Such a high dose is not currently used for the patients with intractable tremor.
Radiation Efficacy
Previous reports demonstrated the effectiveness of GK thalamotomy in treatment of tremor; however, the evaluation of tremor reduction was not uniform (Table 55.1). The Unified Parkinson’s Disease Rating Scale (UPDRS) [28], the Fahn-Tolosa-Marin Tremor Rating Scale [29], and tremor-cessation rates were all used to grade tremor and other symptoms, before and after treatment. Overall, 70–90 % of the tremor patients obtained an anti-tremor effect from GK surgery. Differences in the outcomes of GK surgery in different primary diseases remain unclear due to insufficient numbers of patients.
In order to clarify the safety and ascertain optimally effective conditions for performing unilateral GK thalamotomy for treatment of intractable tremors, a prospective multi-institutional study was published by the Japan Leksell Gamma Knife Society (JLGK0301). The study included blinded videotaped assessments and demonstrated the efficacy of GK surgery for the treatment of both tremor and rigidity in PD; however, no effects on bradykinesia or gait disturbance were found [7].
A slow improvement over several months tended to characterize the clinical course following GK thalamotomy, in contrast to the immediate effect of radiofrequency coagulation. The period over which improvements in clinical symptoms were observed varied widely, from several days to approximately 1 year (Table 55.2) [7–9, 24, 30–32]. A single session of high-dose irradiation requires time to produce the desired lesion. Leksell described autopsy cases in his first report of GK thalamotomy [3]. Lesions irradiated at 200–250 Gy were confirmed pathologically 2 and 5 months after treatment, and the lesions contained necrosis with a marginal gliotic zone. Radiosurgical lesions are dependent on the dose received, volume of tissue irradiated, and time [33, 34]. The low dose of irradiation (130–140) used more recently would require some time to produce the lesion following GK thalamotomy. However, some of the patients treated by GK thalamotomy experienced treatment effects even before coagulation necrosis occurred. Kondziolka demonstrated that the lower doses (80 Gy) used to treat trigeminal neuralgia cause incomplete axonal degeneration in a baboon model [35]. Early changes, prior to coagulative necrosis in the thalamus, might occur after GK surgery and cause an early improvement in clinical symptoms.
Table 55.2
Onset of clinical effects after gamma knife thalamotomy
Author (year) | Dose (Gy) | Onset of clinical effects |
|---|---|---|
Lindquist (1992) [31] | 180 | 1 month |
Friehs (1995) [32] | 160 | 3–4 weeks |
Pan (1996) [8] | 160–180 | 3 days (1 case) |
Young (1998) [33] | 120–160 | 2–3 months |
Duma (1998) [24] | 120 (160) | 1 week to 8 months (2 months) |
Friedman (1999) [9] | 120–140 | 4 weeks |
Ohye (2012) [7] | 130 | 3 months |
Comparison of GK Thalamotomy and Conventional Thalamic Surgery
The anti-tremor effects of GK thalamotomy should be compared with those of other surgical treatment options. However, a head-to-head comparison with other surgical procedures was limited, because various methods of tremor evaluation and variable follow-up terms were applied in each study. Based on tremor-cessation rates, VIM DBS resulted in a tremor-absent state in 67–96 % of both PD and ET patients [36, 37]. VIM thalamotomy also abolished tremor in 65–89 % of PD and ET patients. The tremor-cessation rate achieved with GK thalamotomy was, however, relatively low; 79 % of the patients had good tremor control, including slight or infrequent tremors, which is similar to the results of VIM thalamotomy [37, 38].
Microelectrode Recording After GK Thalamotomy
Some failed cases of GK thalamotomy have been reported. Some of these cases received subsequent conventional thalamotomy, or DBS. In these cases, intraoperative monitoring revealed the radiation effects through electrical activity in the thalamus. Normal neuronal and tremor rhythm were demonstrated in and adjacent to the lesion of the previously irradiated target [39]. Target deviation to the anterior and medial direction, or rhythmic tremor discharge located close to the internal capsule, was less effective. This seems to reflect technical limit of GK thalamotomy at present. We have relatively limited knowledge of the effects of radiation on neuronal activity in the thalamus. Terao et al. reported their microelectrode findings after GK thalamotomy and demonstrated a reorganization of kinesthetic cells in the irradiated VIM [40]. Changes in the somatotopography of kinesthetic cells might make it difficult to perform a secondary surgery on these failed cases.
Complications
Reported complications from GK thalamotomy varied between 1.4 and 46.7 % (Table 55.1). These complications mainly consisted of hemiparesis and speech disturbances. Most of the reported complications were transient; however, some of patients suffered from severe sequelae [6]. A high prescribed dose of radiation seemed to be associated with more complications.
Siderowf et al. reported involuntary movements resulting from GK thalamotomy [41]. Magnetic resonance (MR) images revealed extended edema involving the thalamus, basal ganglia, and midbrain. Dystonia and choreoathetosis emerged, despite a good response to treatment with a marked reduction in the tremor.
Okun et al. reported pseudobulbar laughter following GK thalamotomy [42]; in this case, the tremor persisted following GK thalamotomy. MR images demonstrated extended edema, involving the internal capsule and posterior thalamus. The prescribed dose was unknown in both of these cases. Extended perifocal edema to the neuronal structures surrounding the target site is the expected cause of these complications. Ohye et al. reported thalamic reaction on MR images following GK thalamotomy [7]. Extended T2 elongation surrounding the GK lesion occurred in 10.9 % of the patients, and the prediction of a thalamic reaction was difficult in spite of a uniform treatment protocol.
Gamma Knife Pallidotomy
Posteroventral pallidotomy (PVP) has been used to treat patients with advanced PD, since Laitinen et al. [43] reintroduced PVP and confirmed the results that Leksell and Svennilson et al. [44] and others described earlier [45, 46]. Reviews of controlled studies demonstrated an improvement in quality of life following surgery [47, 48]. Procedures without the need for battery replacement, risk of infection, or hardware problems seemed to be beneficial for some patients with PD. To date, DBS of the subthalamic nucleus and pallidum has become the dominant surgical procedure used for the treatment of PD.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree