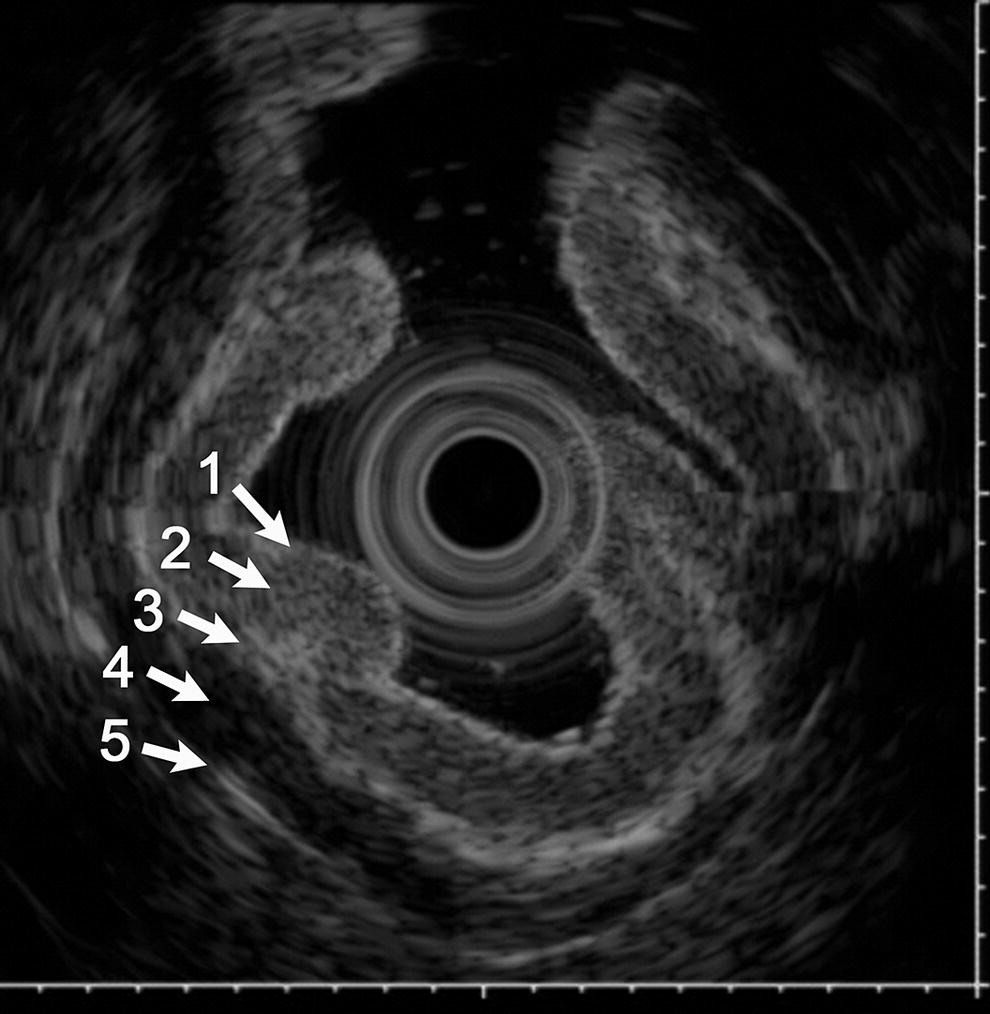
Joo Ha Hwang Stanford University, Palo Alto, CA, USA Endoscopic ultrasound (EUS) examination of the stomach is often performed to evaluate subepithelial lesions, staging of mucosa‐associated lymphoid tumor (MALT) lymphomas, staging of gastric cancer, and evaluation of thickened gastric folds. Examination can be performed using mechanically scanning or electronic array echoendoscopes, or with ultrasound catheter probes. The basic technique for performing EUS imaging of the gastric wall initially requires clearing the gastric lumen of any mucus or debris. The lumen should be thoroughly irrigated with water and suctioned. If there are excessive amounts of bubbles in the gastric lumen, a small amount of simethicone can be added to the irrigating water and suctioned. Once the gastric lumen has been cleared the gastric lumen should be decompressed and then filled with clean water. Ideally, degassed water should be used to fill the gastric lumen; however, this is often not available and clean water typically is sufficient. However, efforts should be made to minimize the presence of bubbles within the water as this will degrade the image quality. It is important to make sure that all air is aspirated from areas where imaging is to be performed. When filling the gastric lumen with the patient on their left side, the fundus and body will fill preferentially due to gravity. If the area of interest is in the antral wall, positioning the patient on their right side may be necessary to safely fill the gastric lumen with water for imaging. Filling of the gastric lumen with water places the patient at risk of aspiration; therefore, precautions should be taken to protect against an aspiration event. After aspirating the air out of the lumen and distending the gastric lumen with water, the gastric wall can be surveyed with a radial scanning echoendoscope by starting the exam with the ultrasound probe in the antrum and slowly withdrawing the probe (Figure 4.1). If only a focal area needs to be examined, the use of a water‐filled balloon can be used, especially for evaluating non‐mucosal lesions such as subepithelial tumors. However, the use of a water‐filled balloon creates an additional interface echo that impacts the image quality at the balloon–mucosa interface. Therefore, a water‐filled balloon should not be used to provide acoustic coupling to mucosal lesions. It is also important to perform imaging within the focal region of the transducer. The mechanical radial scanning echoendoscopes and catheter probes have a fixed natural focus where the best image resolution is obtained. The focal distance can easily be determined by adjusting the distance of the transducer from the gastric wall. The best resolution will be seen when the area of interest is at the focus of the imaging transducer. Electronic array echoendoscopes (radial and curvilinear) have the ability to electronically adjust the location of the focal region; therefore, when imaging the gastric wall, the focal region should be adjusted accordingly. For imaging superficial lesions, the use of a catheter probe through a double‐channel endoscope allows for visual guidance of probe placement. The use of a double‐channel endoscope allows for one channel to be used for the ultrasound catheter probe and the other channel to be used for injecting water into the gastric lumen and suctioning water and air from the gastric lumen. Ultrasound catheter probes are available in frequencies of 12, 20, and 30 MHz. The image resolution increases with increasing frequency; however, penetration (depth of imaging) decreases as frequency increases. The stomach has a well‐developed five‐layered wall structure (Video 4.1). This is easily visualized when water is placed in the lumen. The second layer is often prominent because of the relatively thick columnar mucosa and glands (Figure 4.2). The fourth layer is often thicker in the distal stomach compared to the proximal stomach. The fifth layer generally corresponds to surrounding structures and perigastric fat as the serosa is too thin to be resolved with endoscopic ultrasound. EUS imaging of the gastrointestinal (GI) tract wall typically exhibits five layers; however, seven or nine layers can be resolved if imaging is performed at higher frequencies depending on the region of the GI tract being examined. Initial interpretation of the EUS images assumed direct correspondence of the layers seen on EUS to those seen on histology. It was presumed that the first echogenic layer represented the mucosa, the second echolucent layer the muscularis mucosae, the third echogenic layer the submucosa, the fourth echolucent layer the muscularis propria, and the fifth echogenic layer the serosa and subserosal fat. However, it was later proven that this was an incorrect interpretation of the EUS images of the GI tract wall. In fact, it was demonstrated that the five layers seen on EUS imaging correspond to the following (Figures 4.2 and 4.3). Figure 4.1 Circumferential image of the gastric wall after filling and distending the gastric lumen with water. Image is taken with an electronic radial array echoendoscope at 5 MHz. Figure 4.2 Five‐layer structure of the gastric wall demonstrating a relatively thick mucosal layer (layers I and II). Image is taken with a 20 MHz catheter probe. Figure 4.3 Five‐layer structure of the gastric wall obtained with an electronic radial array echoendoscope at 5 MHz. If a high‐frequency (10 MHz or greater) transducer is used, seven or nine layers can potentially be identified on EUS imaging. These nine layers correspond to the following (Figure 4.4). An important aspect of EUS imaging in the stomach is to maintain orientation of the imaging plane to avoid tangential imaging, especially when evaluating mucosal lesions. Tangential imaging can result in overstaging of lesions. Figure 4.4 Nine‐layer structure of the gastric wall obtained with a 20 MHz catheter probe. The image is the same as Figure 4.2 except additional layers are identified. In conclusion, the only available in vivo method for examining the full thickness of the GI wall, beyond the mucosal surface, is EUS. It provides gastroenterologists with a valuable diagnostic tool to assess pathology in the GI tract to help guide clinical management of the patient. Selection of the correct transducer and using good technique are important in obtaining high‐quality images. When imaging the wall of the GI tract, the method of acoustic coupling is critical. Without good acoustic coupling to the mucosal surface, high‐quality images cannot be obtained. The highest frequency available should be used to image the wall of the GI tract since deep penetration is not necessary unless imaging a large tumor arising from the wall. Using a higher frequency transducer will result in better resolution and allow for better identification of the layers involved. Lower frequencies may be required to identify the size of a mass and if there is involvement with any adjacent structures (T‐staging), and to assess nodal involvement (N‐staging).
4
Stomach: Radial and Linear



Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree